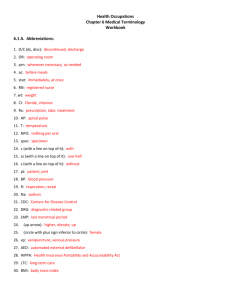
outline3521
advertisement
Pterygiumectomy I. Definition of pterygium A wing-like progressive growth of fibrovascular tissue involving the interpalpebral epibulbar conjunctiva and cornea II. Indications A. B. C. D. E. III. Loss of clarity within visual axis Increasing corneal astigmatism Chronic irritation and inflammation Cosmesis Motility restriction Surgical approaches A. B. C. D. E. Bare scleral excision / avulsion Conjunctival flap Conjunctival autograft Peripheral lamellar keratoplasty Adjunctive therapy 1. Chemotherapy 2. Radiation therapy IV. V. Normal postoperative follow-up A. 1 day, 1 week, 3 weeks, 5 weeks, 3 months B. Patch 1st night C. D. Vicoden ES 1 tablet q 4 hrs prn for pain TobraDex 1 drop qid x 1 week E. Then Pred Forte 1 drop qid with taper until quiet F. G. Artificial tears 1 drop qid x 1 month and regularly thereafter UV protection Complications A. Recurrence (bare sclera 40%, autograft <10%) B. C. D. E. F. G. Subepithelial scarring Scleral melt – mitomycin C Muscle insertion damage Graft inversion Dellen Steroid complication Penetrating Keratoplasty I. Indications A. B. C. D. II. Visual Structural Therapeutic Cosmetic PKP surgical techniques A. B. Anesthesia Corneal trephine 1. 7.5mm diameter button removed 2. 8.0mm diameter donor C. Suturing 1. 2. 3. 4. D. Single running suture – adjustable Interrupted sutures – if corneal scarring secondary to inflammation Double running Running and interrupted combination Advantages of suture adjustment 1. More rapid visual rehabilitation 2. Decreased early postoperative astigmatism 3. Increased regular corneal topography 4. Better visual acuity in early postoperative period III. Postoperative evaluation A. Ideal one day post-op Epithelium intact, clear graft, sutures intact, negative Seidel, formed anterior chamber, normal IOP B. Medications 1. Pred Forte 1 drop q2 hrs - qid 2. Ocuflox 1 drop qid 3. Celluvisc 1 drop qid (and qhs) 4. Artificial tears prn C. Follow-up intervals (variable) 1 day, 3 days, 1 week, 3 weeks, 5 weeks, 2 months, 3 months, 6 months D. Complications 1. Graft rejection – early, late 2. Endophthalmitis 3. Glaucoma 4. Wound leak 5. Delayed reepithelialization LASIK I. Immediate preoperative patient preparation A. B. C. D. E. II. III. Immediate preoperative surgical considerations A. B. C. Primary vs. enhancement Socket configurations – deep set/shallow set Corneal curvature D. Treatment zone based on pupil size, Rx, and pachymetry Operative procedure A. B. C. D. E. F. G. H. IV. VI. Patient positioning Topical anesthesia Suction ring Microkeratome Pre-ablation flap management Fixation and monitoring Ablation Post-ablation flap management Intraoperative challenges A. B. C. D. E. V. Optometric preoperative evaluation and documentation review Corneal topography, pachymetry, scotopic pupil size, excimer Rx and refractive target Informed consent Sedation Laser data entry Stall Suction loss Rolled epithelium Thin/incomplete cap Free cap Immediate postoperative evaluation and considerations A. Slit lamp evaluation B. Flap repositioning indications C. Postoperative patient instructions Postoperative challenges A. B. C. Epithelial defects Cap striae Epithelial ingrowth D. E. Cap interfaces infiltrate – diffuse lamellar keratitis (DLK) Dry eye