Information Governance Dept of eHealth NHS Grampian Rosehill
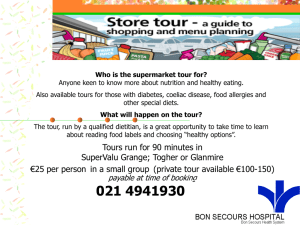
advertisement

Information Governance Dept of eHealth NHS Grampian Rosehill House Foresterhill Site Cornhill Road Aberdeen AB25 2ZG Date Your Ref Our Ref Enquiries to Extension Direct Line Email 7th July 2010 FOI/2010/201 Information Governance Team 51549 01224 551549 nhsg.foi@nhs.net Dear Freedom of Information (Scotland) Act 2002 I refer to your e-mail dated 14th June 2010, requesting: "…Given that 1 in 100 persons the UK suffer from coeliac disease - many of whom remain undiagnosed: …What is the current waiting time for endoscopy (biopsy) for persons with suspected coeliac disease/gluten intolerance after referral by their GP? …What steps do your consultants recommend patients follow prior to these biopsies - e.g. how long should one eat gluten for in preparation for the endoscopy? …What is the success rate of diagnosis of coeliac disease following endoscopy? …How long does a patient have to wait before receiving the results? …If the result is inconclusive, what other methods are used to form conclusive diagnosis of coeliac disease? …If a patient is presented at hospital with chronic stomach problems, are any tests carried out to rule out coeliac disease? …What provision is made by the catering department for inpatients and staff who have coeliac disease or other food intolerances/allergies?" I can now respond as follows: What is the current waiting time for endoscopy (biopsy) for persons with suspected coeliac disease/gluten intolerance after referral by their GP? The current waiting time for an endoscopic biopsy for a patient with suspected celiac disease is around 6 to 8 weeks at present. What steps do your consultants recommend patients follow prior to these biopsies e.g. how long should one eat gluten for in preparation for the endoscopy? Our current recommendation is that patients should not commence a gluten free diet until they have had a distal duodenal biopsy. If a patient is already on a strict gluten free diet and they wish to discuss duodenal biopsies, then usually a consultant would see them to do so. If they wish to go ahead with distal duodenal biopsies, then the consultant would recommend that the patient is on a gluten containing diet for a minimum of 3 months, and ideally for 6 months to allow interpretable results. What is the success rate of diagnosis of coeliac disease following endoscopy? NHS Grampian does not record the number of patients who have a positive diagnosis of celiac disease following an endoscopy; s17 of the Act refers – information not held. However, the gold standard for the diagnosis of coeliac disease would remain a distal duodenal biopsy showing pathological features compatible with coeliac disease. If these features are present then the success rate of the biopsy would be 100%. How long does a patient have to wait before receiving the results? The time taken for the patient to receive their results depends on the time required to report the biopsy, which is usually 10-14 days. The result is then returned to the Consultant and the letter is typed. The result would therefore reach the GP in around 4 weeks. If the result is inconclusive, what other methods are used to form conclusive diagnosis of coeliac disease? In NHS Grampian the standard laboratory test for coeliac disease is the IgA antiendomysial antibody. It is usually recommended that a patient also has their immunoglobulins checked to make sure that they do not have IgA deficiency. All patients should have an anti-endomysial antibody checked as part of the diagnostic process for coeliac disease. If the anti-endomysial antibody is positive and the distal duodenal biopsies are inconclusive, then it would be usual practice for the consultant to see the patient at the clinic to establish whether they have been taking gluten in their diet. If they have been on a normal diet and have a positive anti-endomysial antibody, then the consultant would usually ask for the biopsy to be reviewed at the pathology meeting. If even subtle changes of villous atrophy are present, the consultant would usually accept a diagnosis of coeliac disease. If the biopsy is absolutely normal, then the most likely diagnosis would be latent coeliac disease and the consultant would usually arrange follow-up for the patient perhaps every 1-2 years thereafter. If a patient has a negative anti-endomysial antibody and inconclusive distal duodenal biopsies, then NHS Grampian have access to IgG and IgA tissue transglutaminase which may clarify the diagnosis in a small percentage of patients. We can routinely test for antireticulin antibodies but these are not particularly sensitive. Anti-gliadin antibodies are available in NHS Grampian but are of virtually no diagnostic use in adults with coeliac disease. Finally we are able to get HLA profiling, but currently this is felt to be more useful in excluding coeliac disease, than in confirming a diagnosis. The results can also be very confusing. Usual practice is for the consultant to see patients who have an inconclusive diagnosis of coeliac disease and to discuss with them how they would like to proceed. The treatment is, therefore, individually tailored. If a patient is presented at hospital with chronic stomach problems, are any tests carried out to rule out coeliac disease? Patients who present with gastrointestinal symptoms, including irritable bowel syndrome, often have an anti endomysial antibody test and immunoglobulin profile taken as part of their assessment. The anti endomysial antibody is 95% sensitive and 95% specific. In other words it will be positive in around 95% of patients with coeliac disease and negative in 95% of patients who do not have coeliac disease. For many patients this may be all that is required. If there are stronger reasons to believe that a patient might be a coeliac, and in particular they have very strong features relating to wheat, or a positive family history of coeliac disease, then we will often arrange upper GI endoscopy and distal duodenal biopsies as part of their work up. We can also provide the following general information: In patients who present with iron deficiency anaemia or folic acid deficiency, it is common practice to obtain an anti-endomysial antibody and immunoglobulin profile. In addition, NHS Grampian has defined criteria for carrying out endoscopic investigation of patients with iron deficiency anaemia and in most cases this will also involve taking distal duodenal biopsies. If a patient has had a documented anti-endomysial antibody but has already commenced a gluten free diet we may carry out distal duodenal biopsies if it is felt that the result might be helpful. If the patient has already been on the diet for many months we may simply elect to follow the anti-endomysial antibody and see if it becomes negative. This would again be discussed with the patient on an individual basis. Finally if a patient has a negative antiendomysial and has been following a gluten free diet for more than 9 months, it may not be possible to reach a conclusion about whether they have coeliac disease or not. If they have coeliac disease and have been on a strict diet, then the distal duodenal biopsies may be normal and the anti-endomysial antibody may have been negative. Under these circumstances, the only option open would be a gluten challenge and the consultant would not recommend this except under very rare circumstances and only after complete discussion with the patient. Whilst a diagnosis of coeliac disease is dependant on blood tests and distal duodenal biopsies, the patient’s history and a clinical assessment is also relevant. Finally many patients who do not have coeliac disease, but who have irritable bowel syndrome, do sometimes get benefit from a wheat restricted diet and, therefore, issues of diagnosis and advice have to be tailored to the individual patient, usually after a full consultation. What provision is made by the catering department for inpatients and staff who have coeliac disease or other food intolerances/allergies? Currently, if a patient or member of staff with coeliac disease requires a gluten free diet or has a confirmed food intolerance/allergy the Catering Department can provide suitable meals when made aware of the situation. As part of recent activity following the implementation of a new Grampian Wide Menu and ordering systems a Patient Guide to Food & Fluid Provision information leaflet (one issued to every patient on admission) and supporting Ward Manual for the Provision of Food & Fluid for Hospital Patients has been introduced, detailing the process for obtaining a therapeutic diet and work is also progressing to produce a Therapeutic Diet Book which will contain a range of therapeutic meal choices for a range of therapeutic diets (including gluten free & common food intolerances) along with information on the dietary requirements for each diet type. Under section 20 (1) of the Act, if you are dissatisfied with the way NHS Grampian has dealt with your request, you have a right to request a review of our actions and decisions in relation to your request, and you have a right to appeal to the Scottish Information Commissioner. A request for review must be made within 40 working days and should, in the first instance, be in writing to: Directorate of Corporate Communications, Ashgrove House, Foresterhill, Aberdeen, AB25 2ZN or by email to grampian@nhs.net Requests for appeal should be made in writing to: Scottish Information Commissioner, Kinburn Castle, Doubledykes Road, St Andrews, Fife, KY16 9DS Telephone: 01334 464610, Fax: 01334 464611 e-mail: enquiries@itspublicknowledge.info Yours sincerely Chris Morrice Information Governance Manager NHS Grampian

![Joy Whelan [Community Dietitian WHSCT].](http://s2.studylib.net/store/data/005593477_1-7da42a40dfddf756c95fa7c2298e720b-300x300.png)