Chronic fatigue syndrome/ME-the epidemic
advertisement

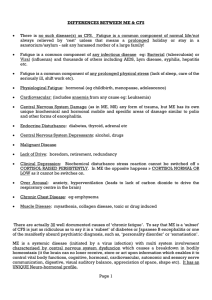
Chronic fatigue syndrome/MEthe epidemic MIRELLA LING Scope Definition of syndrome Common & uncommon exclusions Evidence based treatments NICE backed treatment Relapse management research Local topics/discussion More common than severe AIDS or than many cancers -300 in Worcestershire of 500,000 population 250,000 in UK 0.5% in 18-46 year olds,2% in adolescents 4 month cut off GPs can now refer in patients who had qualifying symptoms for 4 months per NICE though by Fukuda criteria no formal diagnosis to 6 months , so named as ‘post viral fatigue’ in discussion with patient We use term cfs/me in discussion with employers‘Post viral fatigue’ patients can not be protected under disability discrimination act-unlike cfs/me Definitions:Worcester uses-Fukuda(CDC) More than 4 of….. Self-reported impairment in short term memory or concentration Sore throat Tender cervical or axillary nodes Muscle pain Multijoint pain without redness or swelling Headaches of a new pattern or severity Unrefreshing sleep Post-exertional malaise lasting ≥24 hours Not predating and associated with 6 months fatigue with significant reduction in functioning-taken as 50% other symptoms from digestive disturbance/ intolerance to alcohol/light/noise/ autonomic nervous system problem/ palpitations support diagnosis Alternative definition Canadian criteria more immunological/neurological syndromes need to be included-stricter 2 neurological symptoms Preferred by ME patients Less chance of depression getting confused with ME Main ruleouts Fibromyalgia/chronic pain as main symptom even if also cfs PAIN CLINIC ALAN BENNETT OR RHEUMATOLOGY FOR HYDROTHERAPY Part treated depression or psychiatric disorder (Thyroid disease/NIDDM) Exclusions/look for if initial screen NAD Sleep apnoea Brain tumour Addisons/Cushings Myopathies-CK Coeliac HIV/chronic hep B/C Malignancy Haematological disorder-systemic mastocytosis Prior blood tests needed UE FBC ESR LFT TSH GLUCOSE CRP CALCIUM BONE PROFILE CK when indicated TTG = coeliac blood test or duodenal biopsy Treatments offered by Worcestershire clinic Diagnostic service with senior doctor Per PACE trial graded activity-physio CBT/psychology review Adaptive pacing/general advice forms a part Dietician- rarely used Service sees 15 referrals monthly inc out of Worcestershire Not increased 2008-2010.60% have cfs approx and all are referred though not always to team here may be Stourbridge etc Paeds see those to 16 or to 18 in full time education If we take over a pt from paeds-see as new and reassess;not always all new bloods Lyme disease Treatment of chronic Lyme not warranted under current NHS and British Infection society guidelines unless never treated & serologically proven by NHS (CE marked)lab Then only doxycycline 100mg bd (or amoxycillin 1g tds) 4 weeks for arthritis,2 weeks for early Lyme True neuro/cardio complications admit No evidence in mainstream journals for Lightening process still under review Mitochondrial studies/treatment Amygdala training (Gupta technique) Vitamin B12 to above normal level Magnesium injections Hyperbaric oxygen Mindfulness-but used in WRHin 0.5 session Stimulants eg Ritalin(methylphenidate) Low dose thyroxine Efamol marine No evidence for Routine vit D test/Rx The above treatments are therefore outside NHS treatment Vitamin D Don’t test routinely in cfs, use severe pain especially fingers/bones as guide or if patients have low serum calcium of which low vit D or magnesium may be causes Many healthy subjects have low vitamin D (in February when less sunlight if healthy subjects are tested 50-70% would be’deficient’ on blood testing by current limits),so caution needed and we don’t treat borderline levels Below 20 iu/ml total vit D and predominant pain/weakness even with normal calcium/alk phos may merit 3 months colecalciferol 10000 iu daily with 2 weekly bone profile Viral update XMRV,1 of 4 studies only showed excess XMRV in cfs pts No treatment options from this data