NOTES
advertisement

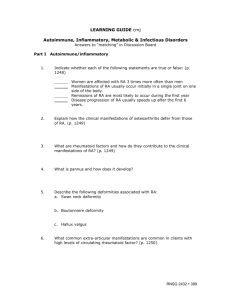
NOTES Musculoskeletal cmj Module #17: Musculoskeletal: Autoimmune, Inflammatory, Metabolic, & Infectious Disorders. Part I Autoimmune/Inflammatory (RA/SLE/ALk/Sclero/Lyme) Etiology/Pathophysiology (general) Complete PDS-Ms Michaels A. Normal physiology- autoimmune/inflammatory musculoskeletal disorders. 1. Commonly called “arthritis”; more than 100 types of “arthritic” disorders affecting skeletal system: focus- “chronic systemic disorder” 2. Diffuse inflammatory lesions and degenerative changes in connective tissue 3. *Review osteoarthritis (p. 1239-1241) Rheumatoid Arthritis A. Etiology/Pathophysiology of Rheumatoid Arthritis 1. Normal antbodies become autoantibodies (rheumatoid factors or RF); attack host tissues which bind with target antigens in blood and with synovial membranes > immune complexes. 2. Synovial membrane damaged from inflammatory and immune processes > erosion of articular cartilage and inflammation of ligaments and tendons. Moderately advanced pannus formation 3. Granulation tissue (pannus) forms over denuded areas of synovial membrane and scar tissue > immobilizing joint. (p. 1249 Fig 39-5). See joint changes and deformities in Power Point as disease progresses (refer to PPT slides in “Required” resources). What is “pannus” (p. 1249) 4. Diarthroidal or synovial joints - primarily involved. 5. Compare to osteoarthritis (as above). B. Common Manifestations/Complications of Rheumatoid Arthritis 1. Joint manifestations a. Onset insidious; may be acute after stressor b. Systemic manifestations (See p.1251) RNSG 2432 381 c. Joint swelling- stiffness, warmth, tenderness and pain; usually multiple joints; symmetric involvement, small, non-weight bearing joints d. Proximal interphalangeal and metacarpophalangeal joints of fingers, wrists, knees, ankles, and toes most frequent. Assessment RA Deformities that may occur with RA Synotenovitis Ulnar drift Swan neck deformity Boutonniere deformity e. Joint deformity results: swan neck and boutoniere; wrist deformity, etc. See p. 1250 fig 39-6 2. Exra-articular manifestations a. While disease active: fatigue: fatigue, weakness, anorexia, weight loss, low-grade fever b. Anemia; skeletal muscle atrophy c. “Rheumatoid nodules” or subcutaneous nodules; develop in subcutaneous tissue in areas subject to pressure on forearm * do not cause problems except pressure areas, disfiguring… Hammer toes Subcutaneous nodules (disappear and appear without warning) 382 RNSG 2432 What are these? d. Pleural effusion, pericarditis, etc C. Therapeutic Interventions for Rheumatoid Arthritis 1. Diagnostic tests *key is R/O other causes (*need to understand this) a. Client history and physical assessment b. Rheumatoid factors (RF), autoantibodies to IgG present in 75% of persons with RA c. Elevation of ESR d. Examination of synovial fluid; signs associated with inflammation e. X-rays of affected joints show changes f. CBC: moderate anemia with elevated platelets 2. Treatment/Medications- (goal control pain and inflammation, preserve function and prevent deformity) *understand this; use with other autoimmune diseases!! Know the drugs!! a. Medications (see text p. 1252-1254; Table 39-5 and table 39-6) Aspirin and NSAIDS, mild analgesics to relieve manifestations, have little effect on disease progression Low dose oral corticosteroids Diverse group of disease-modifying (DMARD’s) or slow-acting anti-rheumatic drugs (know actions, side effects, etc) including gold compounds, d-penicillinamine, antimalarial agents, sulfasalazine, Leflunomide; Etanercept (Arava); Immunosuppressive and cytoxic drugs; intra-articular corticosteroids, new group (biologic response modifiers). How do biologic response modifiers work? (p. 1253) Medications RA ASA & NSAIDS Corticosteroids; low dose DMARDs (Diverse group) of remitting agents: including antimalarial (plaquinal) *eye effects; Penicillamine gold *dermatitis, blood dyscrasia; and Immunosuppressive agents as methotrexate and cyclosporine Biologic response modifiers Adalimumab (Humira) Infliximab (Remicade) RNSG 2432 383 b. Balanced program of rest and exercise Instructions in joint protection Exercise to maintain ROM and muscle strength, low impact exercise Physical and occupational therapy Heat and cold therapy: analgesia and muscle-relaxation Assistive devices and splints -help rest joints and prevent contractures c. Diet: well balanced; some benefit form omega-3 fatty acids d. Surgery - restore joint function e. Teaching Arthritis tutorial (click here-excellent resource for client with arthritis & for health professional) f. Comprehensive approach a must. 3. Nursing Diagnosis (priority) a. Chronic pain b. Fatigue c. Ineffective Role Performance d. Disturbed Body Image ________________________________________________________________ Systemic Lupus Erythematosis (SLE) (click here for more) A. Etiology/Pathophysiology of Lupus *How lupus differs form other autoimmune diseases…understand this! 1. Production of large variety of autoantibodies against normal components of body especially the nucleic acids > development of immune complexes which leads to tissue damage in multiple organs (wide spread damage especially kidney and CNS)* 2. Result of disturbed immunoregulatory disturbance caused by some combination of genetic (three times more frequent in African-American population), hormonal (starts in childbearing years; mostly females) and environmental (stimulated by sunlight; stress) factors. 3. Reaction to some medications (procainamide, hydralazine, isoniazid, chlorpromazine) causes syndrome similar to lupus- usually resolves when medication discontinued. B. Common Manifestations/Complications of SLE (see text illustration p. 1262) 1. Early manifestations: fever, anorexia, malaise, weight loss, multiple arthralgias, symmetric, non-deforming polyarthritis Characteristic butterfly rash associated with SLE, especially discoid lupus erythematous Barry’s lupus 384 RNSG 2432 2. Skin manifestations: butterfly rash (p. 1261 Fig 39.8) across cheeks and bridge of nose accompanied by photosensitivity; alopecia common 3. 50% -have renal involvement including protenuria >lead to renal failure in 10% 4. Cardiovascular: pericarditis most common; early atherosclerosis, vasculitis, etc 5. Hematologic manifestations; anemia, leucopenia, thrombocytopenia 6. Neurologic involvement: seizures, organic brain syndrome, psychosis, memory loss, etc 7. Ocular system: conjunctivitis, photophobia, retinal vasculitis 8. GI symptoms: anorexia, nausea, abdominal pain diarrhea 9. Note: some patients will have only “Discoid lupus” skin involvement, rather than the systemic form C. Therapeutic Interventions of SLE *again similar to RA 1. Diagnostic tests- difficult to diagnose due to diversity of symptoms) a. Clinical history, physical examination b. *Anti-DNA: of various antibodies, this antibody is more specific for SLE, rarely found in any other disorder c. ESR; elevated especially during exacerabations d. *Serum complement levels decreased when antigen-antibody complexes form (exacerbation) * if you don’t recall this response go to text p. 243-245 CBC; severe anemia, leucopenia, other alterations Urinalysis: mild proteinuria, hematuria, blood cell casts BUN and creatinine: determine renal function Kidney biopsy 2. Treatment/Medications- *determined by disease manifestations (has periods remission and exacerbation) a. Mild cases of SLE need only supportive care and possible aspirin and NSAIDs b. *Skin and arthritis manifestations treated with anti-malarial drugs and disease-modifying drugs (same as rheumatoid arthritis); see p. 1253-1254, Table 39-5 & 39-6) c. Severe cases - treated with high-dose corticosteroid therapy tapered as client’s disease allows: may require immunosuppressive agents (cyclophosphamide or azathioprine) alone or with steroids. d. Avoid sun exposure’ important to use sun screen e. May eventually require dialysis if renal involvement f. Teaching about disease process and lifestyle to manage stress 3. Nursing Diagnosis (priority) a. Priority determined by disease manifestations/body system involvement b. Impaired skin integrity c. Ineffective Protection d. Impaired Health Maintenance (include patient teaching as priority). (Link is excellent1) Ankylosing Spondylitis –(Marie Strempel disease) A. Etiology/Pathophysiology of Ankylosing Spondylitis RNSG 2432 385 1. Compare to rheumatoid arthritis: chronic inflammatory arthritis; affects primarily axial skeletal > pain and progressive stiffening and fusion of spine 2. Affects young males, as compared to females 3. Have inflammation, inflammation in sacroiliac joints; joints erodes, joint margins ossify -replaced by scar tissue 4. Joints of spine become involved, gradual calcification > ankylosis, joint consolidation and immobility 5. Cause unknown; strong genetic factor (HLA-B27) (90% have this antigen) What is HLA-B27? B. Common Manifestations/Complications of Ankylosing Spondylitis 1. Gradual and insidious; less severe than RA (See p. 1259 fig 39-7) 2. Bouts of low back pain worse at night, followed by morning stiffness relieved by activity 3. Back motion becomes limited; may become fused Ankylosing Spondylitis Insidious onset Morning backache Inflammation of spine; later spine ossification Oh my back hurts! 4. Systemic manifestations 5. Uveitis (inflammation of the iris) 6. Usually occurs intermittently with mild to moderate acute episodes a. Little risk of permanent severe disability C. Therapeutic Interventions of Ankylosing Spondylitis 1. Diagnostic tests- similar to RA; rule out other disease processes. 2. Treatment/Medications- similar to RA; multidimensional a. Management includes physical therapy and daily exercise; “good” posture important…do not spine to fuse is the above position, affect breathing, mobility severly b. Medications include NSAID’s, especially indomethacin, sulfasalazine (or asulfidine and steroids. c. Teaching; share this information (click here) link with patients; exercises ROM, posture (warm showers, regular NSAIDs, thoracic stretching and ROM exercises *refer to text for additional information to compare ankylosing spondylitis to RA. SLE. osteoarthritis _________________________________________________________________ 386 RNSG 2432 Systemic Sclerosis (Scleroderma) (click here for more information) A. Etiology/Pathophysiology of Scleroderma (hardening of skin) 1. Classified as “connective” tissue disease by some; still in category of auto-immune disease and rheumatoid “arthritis”type disease. 2. Chronic disease characterized by formation of excess fibrous connective tissue and diffuse fibrosis of skin and internal organs 3. Cause unknown; higher incidence in females; persons exposed to certain chemicals; onset between 30-50 4. Prognosis depends upon whether disease localized and limited (CREST syndrome); see p. 1275 or diffuse systemic sclerosis *Localized is Crest syndrome; 80% have this form” CREST Syndrome & scleroderma Sclerodactyl (localized scleroderma of fingers) Raynaud’s disease with ischemia RNSG 2432 387 Typical “hide-bound” appearance of skin 5. Associated with abnormal cellular immunity; develop fibrosis in tissues involving skin, blood vessels, lungs B. Common Manifestations/Complications of Scleroderma 1. 2. 3. 4. Initial marked thickening of skin-“ hide bound”, diffuse non-pitting swelling Eventually skin atrophies > taut and hyperpigmented (p. 1276, Fig. 39-10) Arthralgias and Raynaud’s phenomenon common Visceral organ involvement a. Dysphagia related to esophageal motility b. Pulmonary hypertension c. Pericarditis, cardiac dysrhythmias d. GI problems, including malabsorption e. Proteinuria, renal failure *Need to appreciate the significance of these potential changes to system function….”thickening of tissue > systemic problems” (Reference from Emergency Medicine has excellent photos of individuals with scleroderma.) C. Therapeutic Interventions for Scleroderma 1. Diagnostic tests- Same as for other rheumatoid diseases (R/O other causes) a. *Gammaglobulin level high; low levels of antinuclear antibodies b. Skin biopsy to confirm diagnosis (most important!) 2. **Treatments/medications: determined by disease manifestations. No “cure”. Treatment focus on specific visceral involvement: a. Immunosuppressive therapy and corticosteroids used with pulmonary fibrosis b. Calcium channel blockers and alpha-adrenergic blocking agents to treat Raynaud’s phenomenon c. H2 receptors to treat esophagitis d. ACE inhibitors to treat hypertension and renal involvement e. Physical therapy to maintain mobility of affected tissues especially in hands and face pertaining to ability to eat 388 RNSG 2432 3. Nursing Diagnosis/Nursing Care a. See Nursing diagnosis for RA 4. Nursing diagnosis and nursing care depend upon disease manifestation a. severe skin and organ involvement with inability absorb food and eventually require hyperalimentation b. respiratory compromise due to pulmonary fibrosis c. peripheral involvement > digits can be lost due to severe Raynaud’s phenomenon; develops a “hide bound” appearance d. may be unable to open his/her mouth to eat properly or provide own dental care. (See Power Point slides with Module Objectives e. Instructed to do the following: (important!) 1) Avoid cold 2) Provide skin protection (wear gloves) 3) Avoid infections 4) Eat small frequent meals (in upright position) 5) Stop smoking (due to vasoconstriction) ___________________________________________________________________ Lyme Disease (click here for more) A. Etiology/Pathophysiology of Lyme disease 1. Inflammatory disorder due to *spirochete Borrelia burgdorferi (enters skin at site of tick bite, incubates for 30 days and then migrates outward); transmitted by ticks carried by deer and mice; prevalent in mid-Atlantic, northeastern and north central areas of U.S. *summer months 2. Not an auto-immune disorder; similar “arthritic” manifestations in early stages; important to identify. B. Common Manifestations/Complications of Lyme disease 1. Initial manifestations: a. flu-like symptoms and skin rash b. “Bull’s eye skin lesion at site of tick bite c. Followed by fatigue, malaise, fever, chills myalgias d. Later more skin lesions and muscle and joint pain 2. Weeks to months later a. Bells palsy and meningitis b. Headache and neck stiffness c. Months to years later: chronic recurrent arthritis d. Progression highly individual; maybe permanent disability C. Therapeutic Interventions for Lyme disease RNSG 2432 389 1. Diagnostic tests: a. History of possible exposure to tick bite; recognize characteristic appearance of bite b. Antibodies to B. burgdorferi detected by ELISA or Western blot methods within 2-4 weeks of initial skin lesion c. Organism difficult and slow to culture from tissues or body fluids 2. Treatment/Medications: a. Early recognition and treatment vital to prevent complications b. Antibiotics such as doxycycline, tetracycline, amoxicillin, erythromycin taken for up to a month are effective. c. Arthritic manifestations are treated with aspirin or NSAIDs 3. Nursing Diagnosis/Nursing Care Focus is on prevention and teaching; review text; use this Lyme disease instructional link for helpful teaching information (required) Other Auto-Immune/Inflammatory Diseases Refer to text to read about polymyositis, reactive arthritis (Reiter’s syndrome), Sjogrens syndrome and fibromyalgia. (How are these diseases alike; how different?) (p. 1260, 1265, 1277+) Part II Metabolic Bone Disorders(Pagets and Gout) A. Etiology/Pathophysiology 1. Normal bone remodeling process -sequence of bone resorption and formation 2. Adults replace about 2% of trabecular bone (the porous type of bone found in the spine and all articulating joints) every 4 months through reabsorption of old bone by osteoclasts and formation of new bone by osteoblasts. What is bone reabsorption? 3. Osteoporosis and osteomalacia- types of metabolic disturbances previously covered (see text p. 1223-1230 to review disease process and nursing management) ___________________________________________________________________ Paget’s Disease (go here for more) A. Etiology/Pathophysiology 1. Progressive skeletal disorder-excessive metabolic bone activity > affected bones becoming larger; softer then brittle; abnormal structure 2. Affects femur, pelvis, vertebra, sacrum, sternum, skull 3. Relatively rare; affects more white males 4. Familial tendency 5. Slow progression with 2 stage process (keys of process!) a. Excessive orthoclastic bone resorption b. Excessive osteoblastic bone formation 6. *Bones initially soft -bowing occurs; then hard and brittle > fractures 390 RNSG 2432 What nursing problems can you identify from this slide? Musculoskeletal effects (pain long bones, deformities, deformity, pathological fx, compression fx) Neurological (hearing loss, spinal cord injuries, back pain ) CV (high cardiac output; inc temp over affected extremities) Metabolic (hypercalcemia, hypercalciuria) Case study B. Common Manifestations/Complications of Paget’s Disease (p. 1230) 1. Most asymptomatic 2. Localized pain of long bones, spine, pelvis, cranium; pain mild to moderate deep ache- aggravated by pressure and weight-bearing esp. at night and when resting 3. Flushing and warmth over affected areas; night-time pain 4. May develop pathological fractures 5. Nerve palsy syndrome from involvement of upper extremities; hearing loss* 6. Compression of spinal cord causing tetraplegia 7. Mental deterioration from skull involvement and brain compression 8. **Increased cardiac output due to need for increased blood flow to involved areas; may develop congestive heart failure 9. See p. 1231: Table 39-1; Differential Features of Osteoporosis Osteomalacia and Pagets) C. Therapeutic Interventions for Paget’s Disease 1. Diagnostic tests- X-ray (incidental finding)- localized areas of demineralization in early phase; later enlargement of bones with tiny cracks in long bones or bowing in weight-bearing bones a. Bone scans: show active Paget’s disease b. CT scans and MRI: show degenerative problems, spinal stenosis, nerve root impingement c. *Serum alkaline phosphatase: steady rise as disease progresses; decrease as disease “in remission” *What is serum alkaline phosphatase; how does it reflect bone activity? In what other disease processes does this level rise? (p. 582) d. Urinary collagen pyridinoline testing: indicator of rate of bone resorption RNSG 2432 391 2. Medications/Treatment a. Mild symptoms relieved by aspirin or NSAIDS b. Bone resorption slowed by various meds-: (see p. 1232 chart for implications in administering…know this!) Biphosphonates: calcium supplements also 1. Alendronate (Fosamax): full glass of water or empty stomach & take 30 minutes before food/medications; no lying down for 30 minutes afterward. 2. Pamidronate (Aredia); IV for 3 days, diluted in NS or D5W over 4 hours 3. Tiludronate (Skelid) Calcitonin: also as analgesic for bone pain & inhibits osteoclastic resorption of bone (p. 1231) 4. Salmon calcitonin (Calcimar);Human calcitonin (Cibacalcin) c. Surgery- ? required for joint replacement (hip/knee); nerve decompression if spinal stenosis (management of symptoms) 3. Nursing Diagnosis a. Chronic pain 1) Treatment depends upon location; brace 2) Heat and cold therapy b. Impaired Physical Mobility c. Knowledge deficit; need teaching about disease Gout (go here for more) A. Etiology/Pathophysiology of Gout 1. Syndrome due to inflammatory response due to production or excretion of uric acid > high levels of uric acid in blood/other body fluids as synovial fluid. 2. Metabolic disorder- *deposits of urates in connective tissues of body 3. Primary gout- elevated serum uric acid levels from inborn error of purine metabolism or dec. in renal uric acid excretion due to unknown cause. 4. Secondary gout: hyperuricemia from other disorders or treatments (ie rapid bone breakdown) What types of dieases might cause this?? a. Malignancies (leukemia) b. Chronic renal failure c. Certain medications, such as some diuretics 5. Uric acid- breakdown product of purine metabolism; normally excreted through urine and feces; Levels >7.0mg/dL (normal: 3.4-7.0 mg/mg/dL in males; 2.4-6.0 mg/dL in females) lead to formation of urate crystals in peripheral tissues (synovial membranes, cartilage, heart, earlobes, kidneys) and perpetuate inflammation. (Know normals) B. Common Manifestations/Complications of Gout (See p. 1234, acute and chronic) Have 3 stages in untreated gout 1. Hyperuricemia a. Uric acid levels average 9-10 mg/dL b. Recurrent attacks of inflammation of single joint (most often great toe) 392 RNSG 2432 c. May not progress beyond this stages 2. Acute gouty arthritis a. Acute attack- usually affect single joint b. May be triggered by trauma, alcohol ingestion, dietary excess, stressor, such as surgery or hospitalization c. Affected joint- red, hot, swollen, very painful and tender, often first metatarsophalangeal joint (great toe) PAINFUL! d. Accompanied by fever, elevated WBC and ESR e. Episode lasts hours to weeks -followed by asymptomatic period Tophaceous gout 3. Tophaceous (chronic ) gout a. Occurs when hyperuricemia not treated b. Tophi (sodium urate crystals) develop in cartilage, synovial membranes, tendons, soft tissues c. Skin over tophi -ulcerate exude chalky material and urate crystals d. Lead to kidney disease (uric acid stones can lead to acute renal failure) C. Therapeutic Interventions for Gout 1. Diagnostic tests a. Diagnosis with “classic” presentation: history and physical examination b. Uric acid: usually elevated above 7.5 mg/dL c. WBC: elevation as high as 20,000/mm3 during acute attack d. ESR: elevated e. 24 hour urine collection-determine uric acid production and excretion f. Fluid aspirated (arthrocentesis) from acutely inflamed joints-urate crystals (definitive diagnosis) RNSG 2432 393 2. Medications (See p. 1236 Medication Administration) *Know drugs and how they work/nursing implications!!! a. Used to terminate acute attack/prevent future ones b. Reduce serum uric acid levels c. Treat acute gout attack 1) NSAIDS, specifically indomethacin (Indocin) 2) Colchicine: interrupt cycle of urate crystal deposits and inflammation a) anti-inflammatory use limited to gout b) use limited by significant side effects (see text) 3) Corticosteroids, including intra-articular route 4) Analgesia, including narcotics d. Prophylactic therapy (*Refer to textbook description, implications for use) a) Uricosuric drugs-block tubular reabsorption of uric acid> inc. excretion of uric acid such as probenecid (Benemid) and sulfinpyrazone (Aprazone, Anturane, Zynol) b) Xanthine oxidase inhibitors- lower plasma uric acid levels allopurinol (Zyloprim) 3. Dietary Management a. Contributes only slightly: know *low purine diet (avoid all meats, seafood, yeast, beans, oatmeal, spinach, mushrooms) b. Loose weight; no fasting c. Avoid alcohol, foods that precipitate attack 4. Other Treatments a. Acute attack; bed rest 24 hours post attack! b. Liberal fluid intake (2000 cc)- inc. urate excretion; urinary alkalinizing agents (sodium bicarbonate and potassium)-minimize risk of uric acid stones. Important measure! 5. Nursing Diagnosis a. Acute pain b. Impaired Physical Mobility c. Knowledge Deficit (use this instructional link on Gout for your patients and you!) Part III Infectious Disorders ( Osteomyelitis/Septic Arthritis) Etiology/Pathophysiology 1. Caused by a pathogen 2. Involve bone and joint; difficult to treat 3. Chronic infections lead to pain, deformity, and disability Osteomyelitis A. Etiology/Pathophysiology of Osteomyelitis 1. Infection of bone, may occur as acute, subacute, or chronic 2. Consequence of bacteremia, invasion from contiguous focus of infection, skin breakdown; more prevalent in adults over age of 50 3. Usually bacterial in nature; most common-*Staphylococcus aureus 4. Sources of infection a. Direct contamination of bone from open wounds (trauma) 394 RNSG 2432 b. Complication of surgery c. Extension of chronic ulcers including venous, arterial, diabetic 5. *Infection develops in bone > may interfere with vascular supply to bone > necrosis occurs; difficult for antibiotics to reach the bacteria within the bone (See p. 1266, Fig. 39-9) (Sequestrum = dead bone.) Development of Osteomyelitis Bacteria invade bone Pressure within bone increases Periosteum elevates and bone DIES Infected bone separates = sequestrum Separated periosteum produces new bone = involcrum Sinus tract forms Figure 39.9 Osteomyellitis 6. Specific incidents of osteomyelitis a. Hematogenous osteomyelitis 1) Pathogens carried by blood, primarily older adults, persons with sickle cells anemia, Iv drug users 2) Site of infection usually spine, lumbar region b. Osteomyelitis from a contiguous infection 1) Infection from deep penetrating wounds, TJR, decubitus ulcers, neurosurgery 2) Diagnosis often not made until infection has become chronic -early signs masked by chronic inflammation; non-healing wound or fracture (very difficult to treat) RNSG 2432 395 c. Osteomyelitis associated with vascular insufficiency 1) Clients with PVD and diabetic neuropathy at risk 7. Infection often diagnosed when client seeks treatment for nonhealing wound, swollen toe, acute cellultitis > lead to amputation B. Common Manifestations/Complications of Osteomyelitis (see text p. 1268) (general) 1. Cardiovascular signs of infection/inflammation as tachycardia 2. GI effects as nausea and vomiting 3. Musculoskeletal effects as limp or disuse of involved extremity and localized tenderness 4. Integumentary effects as drainage and ulceration at site; swelling, erythemia and lymph node involvement 5. Other systemic effects of systemic effects of infection as fatigue, low grade temperature, etc. C. Therapeutic Interventions for Osteomyelitis 1. Diagnostic tests (see p. 1269 and Nursing Implications) a. MRI and CT scan > abscesses and soft tissue changes b. Radionucleotides bone scans: determine if infectious or inflammatory change in bone c. CBC and ESR:WBC and ESR elevated; prolonged have mild anemia d. Blood and tissue cultures: identify infectious organism and determine appropriate antibiotic therapy; history and physical assessment 2. Treatment (eradication of infection mandatory)* a. Medications 1) Antibiotics mandatory to prevent acute case from becoming chronic osteomyelitis 2) Initially treat as staph until results of culture are obtained 3) Definitive antibiotics prescribed according to culture results 4) Continue antibiotics for at least 4-6 weeks with intravenous or oral antibiotics 5) Pain medications may be required b. Surgery (see p. 1270 surgical debridement for osteomyelitis) 1) Needle aspiration or percutaneous needle biopsy for specimen; or during debridement procedure 2) *Surgical debridement-primary treatment for chronic cases; wound opened, irrigated; may require drainage tubes for irrigations, suction; antibiotics instilled or antibiotic beads placed. 3) In some cases > amputation c. Treatment lengthy, outcome uncertain; may develop sinus tracts; develop pathological fractures, chronic infections d. *Comparison Acute and Chronic osteomyelitis 1) Acute: refers to initial infection or infection of less than 1 month in duration; clinical manifestations: systemic (fever, night sweats, chills, restlessness, nausea, and malaise); local (constant bone pain, unrelieved by rest and worsens with activity, swelling, tenderness, and warmth at the infection site, and restricted movement of the affected part; later, drainage from sinus tract to the skin and/or the fracture site) 396 RNSG 2432 2) Chronic: bone infection that persists for longer than 1 month or infection that has failed to respond to initial course of antibiotic therapy; systemic signs may be diminished; with local signs of infection more common- inc. constant bone pain and swelling, tenderness and warmth at infection site >develop a constant draining sinus tract 3) *Diagnosis for both: bone or soft tissue biopsy-definitive a) Determine causative microorganism; blood culture; elevated WBC and ESR b) Radiological signs suggestive of osteomyelitis-do not appear until 10 days to weeks post clinical symptoms (may be chronic by this time); radionuclide bone scans (gallium and indium) c) MRI an CT scan also e. **Treatment: Acute and chronic -correct identification of organism/aggressive treatment/antiobiotics IV 1) IV -4-6 weeks- chronic osteomyelitis, follow-up with oral antibiotic therapy and follow-up through bone scans and ESR's to determine resolution of the infection 2) Surgical treatment required (chronic); including removal of poorly vascularized tissue and dead bone; need extended use of antibiotics and antibiotic impregnated polymethymethacrylate bead chains may also be implanted in wound bed-aid in fighting infection 3) Wound irrigation may also be required 4) Protection of limb or surgical site with casts or braces also frequently needed (at high risk for pathological fractures) 5) Hyperbaric oxygenation of 100% oxygen may be administered; treatment of chronic osteomyelitis > promote antibiotic activity and stimulate circulation and healing of infected tissue 6) Orthopedic prosthetic devices (if a source of infection) may need to be removed; myocutaneous flaps or skin and bone grafting to improve blood supply to area may be needed if destruction is extensive; in some cases; amputation 3. Nursing Diagnosis (priority) a. Risk for Infection b. Hyperthemia: interventions include maintenance of adequate fluid intake; appropriate antibiotics c. Acute pain d. Anxiety e. Knowledge deficit (teaching how (click here)nkto recognize signs and symptoms of infections) __________________________________________________________________ Septic Arthritis A. Etiology/Pathophysiology of Septic Arthritis 1. Occurs when joint space invaded by pathogen 2. Risk factors- persistent bacteremia (use of IV recreational drugs, endocarditis urinary tract infection); previous joint damage (trauma, RA); arthroscopic surgery and TJR 3. Common organisms causing disease-staph aureus, streptococci, E. coli, Pseudomonas and gonococci especially in those immunocompromised RNSG 2432 397 4. Infection in joint > synovitis and joint effusion; knee often affected. Synovial inflammation! Comparison acute rheumatoid arthritis and septic arthritis of the joint! Purulent exudate! B. Common Manifestations/Complications of Septic Arthritis 1. Onset: abrupt with pain and stiffness of affected joint which is red, swollen, hot and tender to touch 2. Systemic infection: chills and fever C. Therapeutic Interventions of Septic Arthritis 1. **Prompt treatment to preserve function…very important! (medical emergency) a. Diagnostic tests1) Joint aspiration and fluid sent for gram stain and culture: fluid usually cloudy due to high WBC count 2) X-ray will eventually show demineralization, bony erosion, joint space narrowing 3) CBC, WBC, ESR elevated b. Treatment1) Rest, joint immobilization and elevation 2) Systemic antibiotic therapy; based upon culture results; continued for at least 2 weeks after inflammation has subsided 3) Recurrent joint aspiration and re-culture 4) Physical therapy implemented during recovery to maintain joint function c. Education and supportive care to eliminate behavior that may have contributed to development of Septic Arthritis (go for more!) 398 RNSG 2432