Orthopaedics 4 – Osteoarticular Infections
advertisement

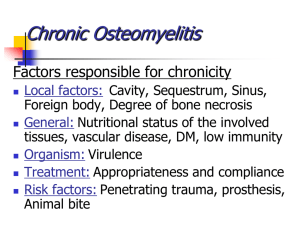
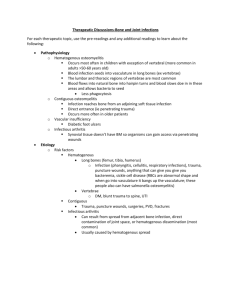
Orthopaedics 4 – Bone and Joint Infections Anil Chopra 1. Describe the natural causes of infection; septic arthritis and osteomyelitis 2. Outline the iatrogenic causes of infection following implants There are 3 common bone and joint infections: • Septic arthritis • Prosthetic joint infection • Osteomyelitis Blood supply of the bones: 10-20% of CO Long bone (3 routes): o Nutrient artery – most important source of arterial blood o Periosteal arteries – supply outer layer of cortical bone o Epiphyseal arteries Short, flat, irregular bone: superficial supply and nutrient artery Rich supply of blood to areas of red marrow (<18yrs – long bone diaphysis, adulthood – flat bones Septic Arthritis Septic arthritis is the infection of a joint. Pathogenesis: - The infection can spread in the blood - Can occur as a result of a complication with a diagnostic or therapeutic procedure. - In children it can be an extension of metaphyseal osteomyelitis. - Normally occurs at the knee and hip joints. - Common pathogens include o 0-3months: S. areus . B streptococcus (E. Coli N. Gonorrhoea) o 3-14 yrs: S. areus, Streptococcus pyrogens, Strep. Prenumonae H. influenza o 15-40 yrs: N. gonorrhoea, Streptococci, gram-negative bacilli o 40+ yrs: Staph Aureus most common organism o Chronic mono-articular septic arthritis: Brucella, Nosodia, Micro-bacteria fungi o Chronic polyarticular: Borrelia burgdorfei Symptoms: - Hot, red, swollen joint - Fever Complications: - impaired range of movement - pain Tests: - FBC, U&E, CRP, Blood cultures - Aspiration o Microscopy o Culture - Gram stain - ZN stain for TB - Arthroscopy Management: - wash out the pus from the joint - intensive care - antibiotics - Rest - Analgesic Prosthetic Joint Infection Pathogenesis: - if it occurs in less than 2 years of having the prosthetic joint, then the pathogen is likely to have come about as a result of surgery - if it occurs in more than 2 years of having the prosthetic joint, then the pathogen is likely to have spread haematogenously - normally caused by coagulase negative staphylococci Symptoms: - pus discharge from infected joint Management - Surgical debridement (removal of dead, damaged or infective tissue) - Intravenous antibiotics (vancomycin) Osteomyelitis Osteomyelitis is an infection of the bone itself. Classical Acute Osteomyelitis Pathogenesis - infection arises in metaphysis. - Spreads in blood - People with sickle cell anaemia are vulnerable - Longer bones normally affected Pathophysiology of Hematogenous Seeding When under pressure, exudates or abscess can extend through Volkmann canals into subperiosteal region, and from there into medullary cavity or epiphysis. Acute Haematogenous Osteomyelitis/ Septic Arthritis: Detail history: Neonates – birth trauma, premature baby who needed invasive support treatment (NICU) Children – antecedent URT infection, trauma (1-2% of ostemyelitis from puncture wound through sole of trainer) Adult – STD, IV drug users Elderly – Recurrent bacteraemia from distant source (UTI) Symptoms: - bone dysfunction (limping) - Pain - Tenderness - Fever - Disability - Deformity Involucrum Sequestrum Septic Arthritis Investigations: - bone scan – shows hotspots - Ultrasound: Sub periosteal collection - MRI: Shows Bone Marrow changes - Full blood count: increased WBC, high C reactive protein, raised ESR Management - Antibiotics (oxacillin, third generation cephalosporin, vancomycin) - surgery - Rest the limb - Drain or aspirate if abscess is obvious Adult Osteomyelitis Pathogenesis: caused by a number of infections Vertebral osteomyelitis 1 Vertebral osteomyelitis 2 Diabetic foot infection Osteomyelitis related to metalwork Symptoms: - bone and joint dysfunction - night sweats - infection of foot ulcer - normally affects lumbar spine - Red - Hot - Painful - Pus - Systemic upset (not in subacute / chronic) - Nerve compression (spine) Investigations: - MRI - Blood tests o Hb o ESR o WCC o CRP - Microbiology very important - Bone scan Treatment: - Laminectomy - Antibiotics - Joint immobility – (hard collar) - Mantoux - Aspirate - Culture - Diabteic control Chronic osteomyelitis: o Inappropriately treated acute osteomyelitis/failure of treatment of acute osteomyelitis o Compromised blood supply o Immunosuppresed o Diabetic o HIV/AIDS Anatomical classification of adult osteomyelitis