Rehabilitation of the Foot and Ankle
advertisement

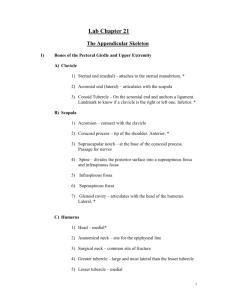
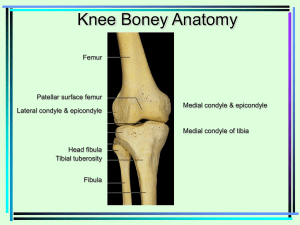
Rehabilitation of the Foot and Ankle Terminology 1. Sagittal Plane a. Medial to Lateral axis b. Dorsiflexion and Plantarflexion 2. Frontal Plane a. Anterior to Posterior axis b. Inversion and Eversion 3. Transverse Plane a. Superior to Inferior axis b. Abduction and Adduction Triplanar Movement Movement occurs simultaneously in the three body plane with motion about a single axis Axes of the talocrural joint, subtalar joint, and midtarsal joint go from posterior/lateral/inferior to anterior/medial/superior Movement includes pronation and supination Pronation = Supination = At each joint, the dominant component sof movement is based upon the orientation of the joint axis Orientation of the joint axis is based on joint structure Inferior Tibiofibular Joint Convex surface of medial fibula articulates with concave fibular notch on the tibia Syndesmosis joint Separates 3-5 mm with ankle dorsiflexion Talocrural Joint Structure - Distal tibia and fibula articulate with talus superior body of talus (trochlea) is convex from anterior to posterior and concave from medial to lateral lateral aspect of talus is longer than medial aspect - Medial concave body of talus articulates with convex medial malleolus - Lateral concave body of talus articulates with convex lateral malleolus Ligaments - Lateral Anterior talo-fibular Calcaneofibular Posterior talo-fibular - Medial Deltoid Motion - Axis - - Tip of lateral malleolus to tip of medial malleolus (posterior/lateral/inferior to anterior/medial/superior) Motion Pronation = Supination = Abduction/Adduction component due to superior shape of talus Requirements for gait 10 degrees of dorsiflexion with knee extension 20 degrees of plantarflexion Subtalar Joint Structure - Inferior talus articulates with superior calcaneous Posterior joint – concave posterior facet on body of talus articulates with convex posterior facet on calcaneous Anterior joint – convex surfaces of middle and anterior facets on neck of talus articulate with concave surfaces of middle facet on sustentaculum tali and anterior facet on neck of calcaneous Ligaments - Interosseous ligament - Cervical ligament Motion - Axis Posterior/lateral/inferior to anterior/medial/superior - Motion Pronation = Supination = OKC = CKC = - Subtalar joint motion during gait usually ranges between 8-12 degrees in the frontal plane Midtarsal Joint Talonavicular joint - Convex neck of talus articulates with concave proximal portion of navicular and middle and anterior facets of calcaneous - Motion Navicular glides dorso-;ateral and plantar-medial on the talus Calcaneo-cuboid joint - Convex distal calcaneous articulates with concave proximal portion of cuboid in dorso-lateral to plantar-medial direction - Concave distal calcaneous articulates with convex proximal portion of cuboid in dorso-medial to planter-lateral direction - Motion Cuboid glides dorso-lateral and plantar-medial on the calcaneous First Ray Structure o Distal navicular articulates with proximal medial cuneiform o Distal medial cuneiform articulates with proximal first metatarsal Motion o Axis is anterior/lateral/plantar to posterior/medial/dorsal o Dorsiflexion/inversion (tibialis anterior) o Plantarflexion/eversion (peroneus longus) Gait o Requires full 1st MTP joint extension o Need to maintain contact between 1st metatarsal with ground during propulsion phase Second Ray Structure o Distal navicular articulates with proximal middle cuneiform o Distal middle cuneiform articulates with proximal second metatarsal Forms the height of the transverse arch Third Ray Structure o Distal navicular articulates with medial facet of cuboid and proximal lateral cuneiform o Distal letaral cuneiform articulates with proximal third metatarsal Fourth Ray Structure o Distal cuboid articulates with proximal fourth and fifth metatarsals Plantar Fascia Continuation of triceps surae fascia Extends from tuberosities on calcaneous to plantar surface of MTP joints FOOT AND ANKLE PATHOLOGIES 1. Forefoot varus 2. Rearfoot varus 3. Ankle equines 4. Plantar fascitis 5. Miscellaneous a. Bunion b. Neuroma c. Turf Toe d. Peroneal tendon subluxation e. Calcaneous epiphysitis f. Metatarsalgia, metatarsal stress fracture 6. Ankle Sprains a. Grades of severity b. MOI for lateral ligament complex c. MOI for medial ligament complex d. MOI for distal tibiofibular ligament complex Ankle Sprain Rehabilitation: I. Inflammatory Phase - P.R.I.C.E. - proprioception - maintenance of CV fitness II. Fibroblastic/Repair Phase - Criteria for progression to phase II - ROM exercises - Flexibility - Strengthening - Proprioception - Weight bearing progression - bracing, taping, orthotics III. Remodeling Phase - Running, jumping, hopping drills - CV fitness - Sport-specific exercises Post-Surgical Rehabilitation: Reconnect peroneus brevis tendon (reinforce lat ankle) - Short leg cast/brace for ~6 weeks - weight bearing progression (* emphasis on normal gait mechanics) - Sagittal plane AROM begun @ 6 weeks - AROM inv/ev begun @ 8 weeks - Strengthening progression - Return to activity LOW LEG PATHOLOGIES 1. Achilles Tendonitis a. Hypovascular region b. Etiology c. Treatment/rehabilitation i. Inflammatory phase 1. 2. 3. ii. Fibroblastic/Repair phase 1. 2. 3. iii. Remodeling phase 1. 2. d. Prevention i. ii. iii. iv. v. 2. Tennis Leg a. Etiology b. Treatment/rehabilitation i. Inflammatory phase 1. 2. ii. Fibroblastic/Repair phase 1. 2. 3. iii. Remodeling phase 1. 2. 3. Compartment Syndromes a. Etiology b. Four compartments i. Anterior ii. Deep posterior iii. Superficial posterior iv. Lateral c. Three syndromes i. Acute ii. Acute-exertional iii. Chronic d. Faciotomy e. Treatment/rehabilitation i. Inflammatory phase 1. 2. 3. 4. ii. Fibroblastic/Repair phase 1. 2. 3. 4. iii. Remodeling phase 1. f. Stress Fractures i. Etiology ii. Tibia vs. Fibula g. Treatment/rehabilitation i. Inflammatory phase 1. 2. ii. Fibroblastic/Repair phase 1. 2. iii. Remodeling phase 1. 2.