Bile duct Reconstruction in Liver Transplant Surgery
advertisement
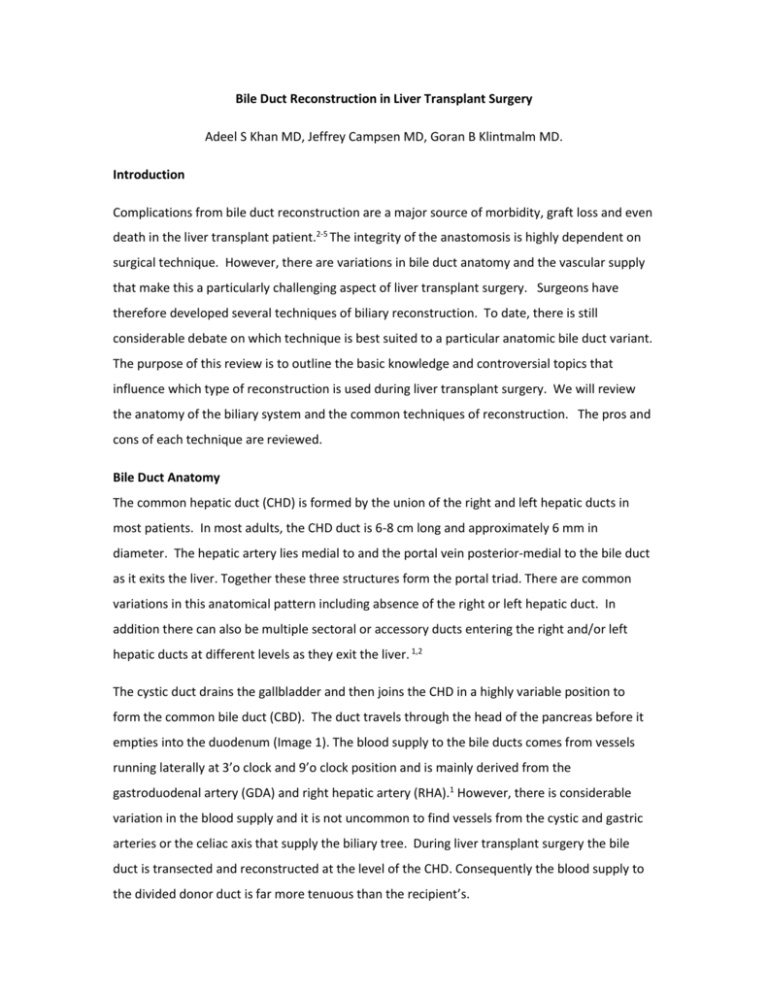
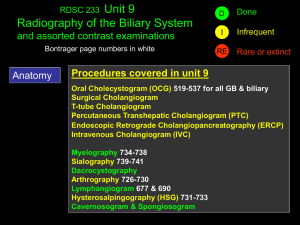
Bile Duct Reconstruction in Liver Transplant Surgery Adeel S Khan MD, Jeffrey Campsen MD, Goran B Klintmalm MD. Introduction Complications from bile duct reconstruction are a major source of morbidity, graft loss and even death in the liver transplant patient.2-5 The integrity of the anastomosis is highly dependent on surgical technique. However, there are variations in bile duct anatomy and the vascular supply that make this a particularly challenging aspect of liver transplant surgery. Surgeons have therefore developed several techniques of biliary reconstruction. To date, there is still considerable debate on which technique is best suited to a particular anatomic bile duct variant. The purpose of this review is to outline the basic knowledge and controversial topics that influence which type of reconstruction is used during liver transplant surgery. We will review the anatomy of the biliary system and the common techniques of reconstruction. The pros and cons of each technique are reviewed. Bile Duct Anatomy The common hepatic duct (CHD) is formed by the union of the right and left hepatic ducts in most patients. In most adults, the CHD duct is 6-8 cm long and approximately 6 mm in diameter. The hepatic artery lies medial to and the portal vein posterior-medial to the bile duct as it exits the liver. Together these three structures form the portal triad. There are common variations in this anatomical pattern including absence of the right or left hepatic duct. In addition there can also be multiple sectoral or accessory ducts entering the right and/or left hepatic ducts at different levels as they exit the liver. 1,2 The cystic duct drains the gallbladder and then joins the CHD in a highly variable position to form the common bile duct (CBD). The duct travels through the head of the pancreas before it empties into the duodenum (Image 1). The blood supply to the bile ducts comes from vessels running laterally at 3’o clock and 9’o clock position and is mainly derived from the gastroduodenal artery (GDA) and right hepatic artery (RHA).1 However, there is considerable variation in the blood supply and it is not uncommon to find vessels from the cystic and gastric arteries or the celiac axis that supply the biliary tree. During liver transplant surgery the bile duct is transected and reconstructed at the level of the CHD. Consequently the blood supply to the divided donor duct is far more tenuous than the recipient’s. Type of Anastomosis Bile duct reconstruction during liver transplantation is usually performed by an end to end anastomosis (choledocho-choledochostomy [DD]) between the donor and recipient common bile ducts. The next most common technique is an end to side Roux-en-Y hepaticojejunostomy (RYHJ).4-7, 12-14 In the latter procedure, the end of the hepatic duct is anastomosed to the side of the jejunum. Direct insertion of the common bile duct into the duodenum known as choledocho-duodenostomy (CD) is a third but less common option for biliary reconstruction.9 Duct-to-Duct Anastomosis (DD) (Choledochocholedochostomy): The common bile ducts of the donor and recipient can be anastomosed as an end-to-end choledocho-choledochostomy. This is the technique of choice for biliary anastomosis in deceased donor liver transplantation (DDLT). It is a technically easier and faster procedure than a RYHJ. The DD also avoids intestinal manipulation, maintains anti-reflux mechanism of sphincter of Oddi and provides easy access for endoscopic intervention in case of future anastomotic strictures.7,8,10,17 The anastomosis itself can be performed using interrupted or running mono-filament (absorbable or non absorbable) suture. It can be technically challenging if the ducts are very small or if there is a large size discrepancy between donor and recipient bile ducts. The latter issue is particularly important in pediatric liver transplantation. The most expeditious way to address the donor and recipient duct size discrepancy is to make a side-cut on the side of the smaller duct (usually donor side). With very large ducts a choledochoplasty of the oversized duct can be performed. Neuhaus et al from Germany described a technique of side-to-side anastomosis between the donor and recipient common bile ducts (choledocho-choledochostomy) instead of the more common end to end method. Studies have shown that this is as safe option for performing bile duct anastomosis and has a low complication rate.14 Roux-en-Y hepaticojejunostomy (RYHJ): In this technique, a loop of small bowel 10-20 cm distal to the ligament of Treitz is divided and brought up to the donor bile duct. An end to side anastomosis is then completed between the two (Image 2). The RYHJ is a preferred technique when the donor bile duct diameter is small (pediatric, split liver and living donor transplants) and in patients with extrahepatic biliary disease (eg. primary sclerosing cholangitis, Caroli’s disease and cholangio-carcinoma). There are unique complications associated with type of biliary reconstruction that are related to the surgical enteric anastomosis. This approach adds to the operative time because it involves small bowel resection and anastomosis. In addition, there is an increase the risk of peritonitis due to enteric leaks and bleeding complications. These complications are exacerbated by the high venous pressure associated with portal hypertension in some patients. There is also an increase the risk of developing ascending cholangitis from contamination with gut flora. Further, subsequent endoscopic intervention to treat bile duct narrowing is difficult if not impossible.7,8,10,12,17,22 Choledochoduodenostomy (CD): This technique involves direct anastomosis between the end of the bile duct and the side of the duodenum. The CD has been shown in a several studies to be a safe alternative to a Roux-en-Y when a duct-to-duct anastomosis cannot be performed.9 Advantages include the ease of postoperative access to the biliary system. However this type of anastomosis may expose the biliary system to enteric contents raising the risk of ascending cholangitis. (Image 3) Role of T-tube/stenting Insertion of biliary drainage catheters or T-tubes has been a topic of controversy in the transplant community. The rationale for using T-tubes includes the ease of access to the biliary system and protecting the anastomosis against narrowing by the insertion of an internal stent. In addition, the T-tubes allow physicians to monitor the quality of the bile and thus the function of the liver graft which can provide critical information in cases of primary non-function. It also allows endoscopic access to bile ducts to diagnose or repair a stenosis or leak. Some investigators think that T-tubes may protect the anastomosis from developing leaks by lowering the intra-ductal pressure.7 However initial randomized trials that examined the safety of T-tubes in liver transplant recipients showed that biliary complications occurred in up to 50% of patients.11-15 These complications included narrowing of the bile duct lumen, cholangitis, spontaneous dislodgement of the T-tube, and bile leaks following T-tube removal. These complications seem to be caused by impaired healing due to immunosuppression. Spasm of sphincter of Oddi is also thought to occur more frequently in patients with T-tubes. These findings discouraged transplant surgeons from using T-tubes and a recent meta-analysis confirmed this observation by demonstrating that most of the larger transplant centers now avoid the use of T-tubes in cadaveric liver transplants.15 Bile duct reconstruction in living donor liver transplantation Living donor liver transplantation (LDLT) is an accepted option to increase the donor organ pool 16,17,19,20 . The long term outcomes are comparable to deceased donor liver transplants. 23. Both the right and left hemi-liver are used in adult to adult living donation surgery. In contrast, the left lateral section (segments 2 and 3) is commonly used when an adult donates to a pediatric patient. The biliary reconstruction in LDLT patients tends to be more challenging than in cadaveric liver transplants because the ducts are smaller and can have multiple or irregular branching depending on the plane of transection. 17 Roux-en-Y hepaticojejunostomy (RYHJ) was considered the standard approach for LDLT biliary reconstruction until 1998 when Wachs et al reported the first case of duct-to-duct reconstruction for right hemi liver transplant. 16 Since then several studies have reported good outcomes using duct-to-duct biliary anastomosis for LDLT. 17,19,20 A single hepatic duct is favored for a DD anastomosis. If two ducts are present, a DD anastomosis can still be used if the openings are less than 3 mm apart. In this case, the duct is modified to create a single orifice. If the distance is greater than 3 mm then two separate hepaticojejunostomies are performed using a Roux-en-Y loop. 5 In 2005 Asonuma et al. described using the recipient cystic duct for biliary reconstruction in right liver donor transplantation when two bile duct orifices were present. 24 The advantages and disadvantages of using the different biliary reconstruction techniques are similar to those for deceased donor liver transplant as described above however, the outcomes in LDLT recipients are not as good due to higher rates of biliary complications seen with LDLT (see complications). The use of biliary drainage catheter or T-tube in LDLT is as controversial as their use in DDTL. Overall, T-tubes are rarely used in LDLT. 5,12,13,14,17 Complications of bile duct reconstruction Calne in 1976 described the biliary anastomosis as the “Achilles heel” of liver transplantation3. This observation still stands true today. Biliary complications after liver transplant occur in 934% of all liver transplant recipients. They are more common in LDLT due to smaller sized and often multiple ducts. 3,5,8,17,20 The most common complications seen are bile leaks and anastomotic strictures, Two thirds of these complications present in the first three months. 18 Bile leaks complicate up to 20% of liver transplant surgeries. Early bile leaks (<4 weeks) are generally considered a technical complication and usually occur at the site of anastomosis. 10 Causes can include loose or widely placed sutures, ischemic necrosis of the bile duct edges often from small and tightly placed sutures or from hepatic artery stenosis or thrombosis. 5, 10, 17 Because the biliary anastomosis relies on blood flow from the right hepatic artery, a reduction in blood supply can manifest as a bile leak. Late bile leaks are rare and are usually seen in patients with T-tubes after their intentional or inadvertent removal. 4,10,14,15 Bile leaks can present with altered liver function test and/or peritonitis from bilious ascites. If left untreated, this can progress to sepsis from an infected biloma. 6,18,22 Bile Duct strictures are seen in as many as 27% of liver transplants 7.Similar to bile leaks, early anastomotic strictures (<4 weeks) are commonly due to a technical problem such as tight sutures, purse-stringing of anastomosis or “back-walling” of posterior wall. Bile duct ischemia from hepatic artery stenosis, thrombosis or devascularized duct edges can also predispose to strictures. However, these generally present in a more indolent fashion. 4,6,10,17 Other factors that increase the risk of late anastomotic strictures include chronic ductopenic rejection, prolonged cold ischemia time (>12 hrs), ABO incompatibility, cytomegalovirus (CMV) infection and recurrent primary sclerosing cholangitis (PSC). 6,10 Patients present with a number of signs and symptoms of biliary obstruction including jaundice, itching, fever, and pain from cholangitis. There have been many studies and randomized trials comparing the outcomes of patients with DD and RYHJ reconstruction. The risk of bile leak in DDLT is not strongly associated with the method of biliary reconstruction. 18,21 Even though bile duct strictures can be seen with either approach, at least two large studies report higher stricture rates with RYHJ compared to DD. 2,21 A review of LDLT literature suggests that there are overall higher rates of bile leaks and biliary strictures compared with DDLT. 5,717,20 DD reconstruction appears to have a lower incidence of bile leaks but a higher incidence of biliary strictures when compared to RYHJ. 8 We have focused upon bile duct complications. However, there are other significant biliary complications after liver transplant. These include non-anastomotic strictures, ampullary dysfunction, hemobilia, choledocholithiasis and mucocele of cystic duct stump. 3,4,6,10 (Table 2) Diagnosis: All evaluations for biliary anastomotic leaks and strictures should include a full assessment for the presence of hepatic artery blood flow. Hepatic artery stenosis or thrombosis can be identified by duplex sonography or angiography. The diagnosis of both anastomotic strictures and leaks can be made with imaging techniques such as percutaneous transhepatic cholangiography (PTC) and endoscopic retrograde cholangiography (ERC). Ultrasonography is rarely helpful in diagnosing post transplant biliary strictures. Undrained extrahepatic bile collections can be diagnosed by computed tomography (CT) scan or ultrasound. 2,4,6,10,17,18 Magnetic resonance cholangio pancreatography (MRCP) is gaining popularity as a selective screening tool in patients with biliary complications. 6 Management of biliary complications Treatment strategies for biliary complications after liver transplant vary with the experience of each transplant center. 3,22 However, a few generalizations can be made. The first step in the management of biliary strictures or leaks aims to ensure hepatic arterial patency. Any inflow compromise must be definitively treated before a biliary intervention is attempted. Anastomotic bile leaks after liver transplants (both DD and RYHJ) are almost always managed surgically. Treatment may include the surgical revision of an anastomosis or the conversion of a DD to a RYHJ. Some centers have described success managing small anastomotic leaks after liver transplants with endoscopic stenting (DD) and PTC stenting with an internal-to-external drain (RYHJ). 3,6,12,21,22 but surgery remains the main stay of treatment. Endoscopic balloon dilation and stenting is generally the first step in treating biliary strictures after liver transplant. In patients with RYHJ where endoscopic intervention may not be possible, PTC dilation with an internal-external drain may be used. Long term results with management of early strictures are good but delayed strictures tend to be more resistant to therapy. Thus, patients may require multiple sessions over a 2-3 month period. Refractory strictures and strictures involving a long segment of bile duct usually require a surgical intervention in the form of conversion of DD to RYHJ or revision of RYHJ. 3,6,12,21,22 Some centers are more aggressive with management of biliary strictures and prefer early surgical intervention as opposed to multiple endoscopic dilations. Non anastomotic strictures are more refractory to balloon dilation and often require surgical intervention or re-transplant. Bleeding into the biliary tree can be managed with endoscopic retrieval of clot and embolization of involved vessel. Sludge and stone formation can be diagnosed and treated with ERC and PTC approached. The use of ursodeoxcholic acid may further delay new stone formation. Mucoceles of the cystic duct stump usually need surgical decompression because they recur if only drained . 6,21,22 Summary Bile duct complications are common in liver transplant recipients. They occur more frequently in LDLT recipients compared to DDLT. This is probably related to the smaller size of the bile ducts and more variation in the anatomic divisions of the hepatic duct. Surgeons have identified three common techniques for bile duct reconstruction: duct to duct, Roux-en Y hepaticojejunostomy and insertion of the bile duct into the duodenum. To date there is no consensus guiding the selection of one technique over another. The only exception is that most surgeons agree that RYHJ is preferential for patients with extrahepatic biliary disease. Complications of bile duct reconstruction occur with all surgical techniques. However, some complications are more commonly associated with one type of reconstruction compared to another. Important factors that are considered when choosing a technique for bile duct reconstruction includes LDLT vs. DDLT, bile duct anatomy, size discrepancy and access to the biliary tree to treat postoperative complications. References: 1. Adkins RB Jr, Chapman WC, Reddy VS. Embryology, anatomy and surgical applications of the extrahepatic biliary system. Surg Clin North Am. 2000 Feb;80(1):363-79 2. Colonna JO: Technical problems: biliary. In Transplantation of the liver, end 1. Edited by Busuttil R, Klintmalm G. Philadelphia: WB Saunders Co;1996:617-625 3. Perrakis A, Fortsch T, Schellerer V, Hohenberger W, Muller V. Biliary tract complications after orthotopic liver transplantation: still the “Achilles heel”? Transplantation proceedings 2010;42:4154-57 4. Pascher A, Neuhaus P. Biliary complications after deceased-donor orthotopic liver transplantation. J Hepatobiliary Pancreat Surg 2006;13:487-96 5. Chan SC, Fan ST. Biliary complications after liver transplantation. Hepatol Int 2008;2:399-404 6. Jagannath S, Kalloo AN. Biliary complications after liver transplantation. Curr treatment options in gastroenterology 2002;5:101-12 7. Feng XN, Ding CF, Xing MY, Cai MX, Zheng SS. Technical aspects of biliary reconstruction in adult living donor liver transplantation. Hepatobiliary Pancreat Dis Int. 2011;10(2):136-42 8. Yazumi S, Chiba T. Biliary complications after a right-lobe living donor liver transplantation. J Gastroenterol 2005;40:861-65 9. Bennet W, Zimmerman MA, Campsen J, Mandell MS. Bak T, Wachs M, Kam I. Choledochoduodenostomy is a safe alternative to Roux-en-Y choledochojejunostomy for biliary reconstruction in liver transplantation. World J Surg 2009;33:1022-25 10. Franco J. Biliary complications in liver transplant recipients. Current gastroenterology reports 2005;7:160-4 11. Weiss S, Schmidt S, Ulrich F, Pascher A, Schumacher G, Stockmann M, Puhl G, Guckelberger O, Neumann U, Pratschke J, Neuhaus P. Biliary reconstruction using side to side choledochocholedochostomy with or witout T-tube in deceased donor liver transplantation: A prospective randomized trial. Ann Surg. 2009;250(5):766-71 12. Vougas V, Rela M, Gane E, et al. A prospective randomized trial of bile duct reconstruction at liver transplantation: T tube or no T tube? Transpl Int. 1996;9:392–395 13. Scatton O, Meunier B, Cherqui D, et al. Randomized trial of choledochocholedochostomy with or without a T-tube in orthotopic liver transplantation. Ann Surg. 2001;233:432–437 14. Neuhaus P, Blumhardt G, Bechstein WO, Steffen R, Platz KP, Kech H. Technique and results of biliary reconstruction using side-to-side choledochocholedochostomy in 300 orthotopic liver transplants. Ann Surg. 1994;219(4):426-34 15. Riediger C, Muller MW, Michalski CW, Huser N, Schuster T, Kleeff J, et al. T-tube or no T-tube in the reconstruction of the biliary tract during orthotopic liver transplantation: systematic review and metaanalysis. Liver Transpl 2010;16:705-17 16. Wachs ME, Bak TE, Karrer FM, Everson GT, Shrestha R, Trouillot TE, et al. Adult living donor liver transplantation using a right hepatic lobe. Transplantation 1998;66:1313-1316 17. Liu CL, Lo CM, Fan ST. What is the best technique for right hemiliver living donor liver transplantation? With or without the middle hepatic vein? Duct-to-duct biliary anastomosis or Roux-en-Y hepaticojejunostomy? Journ Hepatol 2005;43:13-17 18. Scanga AE, Kowdley KV. Management of biliary complications following orthotopic liver transplantation. Current gastroenterology reports 2007;9:31-8 19. Grewal HP, Shokouh-Amiri MH, Vera S, Stratta R, Bargous W, Gaber AO. Surgical technique for right lobe adult living donor liver transplantation without venovenous bypass or portocaval shunting and with duct-to-duct biliary reconstruction. Ann Surg 2001;233:502-508 20. Malago M, Testa G, Hertl M, Lang H, Paul A, Frilling A, et al. Biliary reconstruction following right adult living donor liver transplantation end-to-end or end-to-side duct-to-duct anastomosis. Langenbecks Arch Surg 2002;387:37-44 21. Greif F, Bronsther OL, Van Thiel DH et al,: the incidence, timing, and management of biliary tract complications after orthotopic liver transplantation. Ann Surg 1994;219:40-45 22. Kuo OC, Lewis WD, Stokes K, et al: A comparison of operation, endoscopic retrograde cholangiography, and percutaneous transhepatic cholangiography in biliary complications after hepatic transplantation. J Am Coll Surg 1994 179:177 23. Olthoff KM, Merior RM, Ghobrial RM, Abecassis MM, Fair JH, Fisher RA, et al. Outcomes of 385 adultto-adult living donor liver transplant recipients: a report from the A2ALL consortium. Ann Sugg 2005;243(3):314-23 24. Asonuma K, Okajima H, Ueno M, Takeichi T et al. Feasibility of using the cystic duct for biliary reconstruction in right lobe living donor liver transplantation. Liver Transpl. 2005 Nov;11(11):1431-4 Table 1: Comparison of techniques of bile duct reconstruction during liver transplant. Technique Advantages Disadvantages Duct to Duct anastomosis (DD) Technical ease Technically difficult in LDLT, split liver (Choledocho-choledochostomy) Quick and pediatric transplant patients End to end anastomosis Preservation of anti-reflux mechanism Not recommended in pts with biliary Side to side anastomosis of sphincter of Oddi pathology (PSC, cholangio CA etc) Access for endoscopic intervention preserved Roux-en-Y Hepaticojejunostomy Duct size not an issue Longer operative time (RYHJ) Good option in pts with biliary Intestinal manipulation pathology (PSC, cholangio CA) Delay in return of GI function Bacterial contamination of bile duct Risk of enteric leaks, anastomotic bleeding and internal hernias Choledocho-duodenostomy Technical ease Risk of reflux of GI contents in duct (CD) Avoids intestinal manipulation causing cholangitis Access for endoscopic intervention maintained Table 2: Causes of biliary complications after liver transplant Complication Common Causes Anastomotic leaks Early (<4 weeks) Technical, ischemia Late (>4 weeks) T-tube removal Anastomotic strictures Early (<4 weeks) Technical, ischemia, post operative inflammation and edema Late (>4 weeks) Ischemia, chronic rejection, CMV infection, prolonged cold ischemia time, ABO incompatibility, recurrent biliary disease Non anastomotic strictures Ischemia, unclear etiology Choledocholithiasis Stasis, biliary stricture Ampullary dysfunction Denervation of ampullary region, CMV infection Mucocele of cystic duct stump Impaired drainage of cystic duct stump Hemobilia Liver biopsy, PTC Image 1: Anatomy of the biliary tree. Adapted with permission from Transplantation of the liver. Second edition. Edited by Busuttil R, Klintmalm G. Philadelphia: WB Saunders Image 2: Roux-en-Y Hepaticojejunostomy (RYHJ) Image 3: Cholecystoduodenostomy (CD) reconstruction of two right sided bile ducts during LDLT. Questions: 1) Blood supply to the bile duct anastomosis after liver transplant is mainly derived from: a. Gastroduodenal artery b. Left hepatic artery c. Right hepatic artery d. Common hepatic artery e. Right gastric artery Answer: C 2) The most common complication of bile duct reconstruction after liver transplant is: a. Anastomotic stricture b. Cholangitis c. Hemo-bilia d. Bile leak e. Choldocholithiasis Answer: D 3) Most of the bile duct reconstructions after standard liver transplants are: a. Duct to duct choledocho-choledochostomy b. Roux-en-Y hepaticojejunostomy c. Choledochojejunostomy d. Side to side choledocho-choledochostomy Answer: A 4) This method of bile duct reconstruction preserves the natural anti-reflux mechanism of the sphincter of Oddi a. Duct to duct choledocho-choledochostomy b. Roux-en-Y hepaticojejunostomy c. Choledochoduodenostomy Answer: A 5) A 40 year old male undergoes a successful deceased donor liver transplant. He is taken back to the operating room on post operative day 1 for bleeding. During the surgery small amount of bile is seen leaking from the anastomosis. The most likely cause of this bile leak is: a. Bile duct ischemia b. Post operative bleed c. Acute cellular rejection d. Technical error at time of initial bile duct anastomosis e. CMV infection Answer: D 6) A 30 year old woman undergoes liver transplant for primary sclerosing cholangitis. Bile duct is reconstructed using a Roux-en-Y hepaticojejunostomy. Post operatively an anastomotic stricture is suspected. What is the best way to reach the diagnosis in this patient? a. Endoscopic retrograde cholangiography (ERC) b. Percutaneous transhepatic cholangiography (PTC) c. Computed tomography (CT) scan of the liver d. Duplex sonography of the transplanted liver Answer: B 7) The best reconstruction option during right living donor liver transplant for two bile duct orifices 1 cm apart is: a. Duct to duct choledocho-choledochostomy b. Side to side choledocho-choledochostomy c. Roux-en-Y hepaticojejunostomy d. Choledochoduodenostomy Answer: C 8) Living donor liver transplants (LDLT) are associated with a higher rate of biliary complications than deceased donor liver transplants (DDLT) a. True b. False Answer: True 9) Duct-to-duct anastomosis should never be performed in living donor liver transplants a. True b. False Answer: False 10) Most of the transplant centers in the US routinely use T-tubes as part of bile duct reconstruction a. True b. False Answer: False