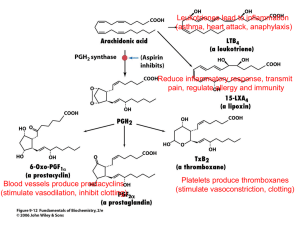
Clinical Guidelines for the use of NSAIDs and COX
advertisement

Yorkshire Palliative Medicine Guidelines Group GUIDELINES ON THE USE OF NON-STEROIDAL ANTI-INFLAMMATORY DRUGS (NSAIDs) AND SELECTIVE CYCLO-OXYGENASE-2 (COX-2) INHIBITORS IN PALLIATIVE CARE April 2010 Authors: Dr Julia Barnes, Dr Rachel Sorley and Dr Milind Arolker on behalf of the Yorkshire Palliative Medicine Clinical Guidelines Group. Overall Objective: Using a ‘Frequently Asked Questions’ format we present evidence and recommendations relating to the use, and with particular emphasis on reducing some risks, of using NSAIDs and selective COX-2 inhibitors. Search strategy: Evidence was examined and summarised from systematic reviews, meta-analyses and national guidelines and Medline/Embase databases were searched if the above provided insufficient information. A hierarchy of information sources was agreed within the group: 1. Cochrane/ Database of Abstracts of Reviews of Effectiveness (DARE) 2. SIGN/NICE 3. Clinical Knowledge Summaries (CKS) 4. Bandolier 5. Palliative Care Formulary, third edition 6. Medline/Embase via Search 2.0: search drug & adverse effect (with thesaurus mapping) Searches were limited to papers published in English. See appendix 1 for the Cochrane/Medline/Embase search strategy. Level of evidence: Evidence has been graded according to criteria described by Keeley (2003) – see appendix 2. Review date: August 2013 Competing interests: None declared Disclaimer: These guidelines are the property of the Yorkshire Palliative Medicine Guidelines Group. It is intended that they be used by qualified, specialist palliative medicine professionals as an information resource. They should be used in the clinical context of each individual patient’s needs and reference to appropriate prescribing literature should also be made. The Yorkshire Palliative Medicine Guidelines Group takes no responsibility for any consequences of any actions taken as a result of using these guidelines. Contact details: Dr Lynne Russon, Consultant in Palliative Medicine, Leeds Teaching Hospitals NHS Trust/Sue Ryder Care Wheatfields Hospice, Grove Road, Headingley, Leeds LS6 2AE E-mail: Lynne.Russon@suerydercare.org 2 CONTENTS Introduction 4 Summary of conclusions/recommendations 7 NSAIDs/selective COX-2 inhibitors and: Gastro-intestinal bleeding References 11 15 Concomitant use of corticosteroids References 21 23 Concomitant use of aspirin References 27 28 Concomitant use of anti-coagulants References 31 33 Bronchospasm/asthma References 38 40 Heart failure References 42 44 Thrombotic events References 47 50 Renal impairment References 56 58 Cancer-induced bone pain References 63 66 Subcutaneous ketorolac References 69 71 Appendices: 1. 2. 3. 4. Search strategies Grading of evidence Glossary of italicised terms Acknowledgements and authors 3 74 75 76 78 INTRODUCTION NSAIDs/selective COX-2 inhibitors are commonly used classes of drugs with around one-third of people over the age of 65 in developed countries thought to be using an NSAID on a daily basis.1 Patients in the palliative care population often have multiple co-morbidities and polypharmacy which compound their risks of experiencing adverse drug effects. These sideeffects can adversely affect their quality of life and symptom control. NSAIDs are anti-inflammatory, anti-pyretic and analgesic drugs and work by inhibiting cyclo-oxygenase. This enzyme converts arachidonic acid to thromboxanes and prostaglandins (See figure 12). There are 2 types of COX enzymes: COX-1 is ‘constitutive’ and present in most tissues of the body at constant levels. It catalyses the initial step in the formation of thromboxane A2 and prostaglandins involved in the regulatory and cytoprotective functions in platelets, renal cells and gastrointestinal mucosa. COX-2 is ‘inducible’ by inflammation and produces prostaglandins that mediate pain and inflammation. Prostaglandin synthesis in tissues and the CNS is reduced by NSAIDs which results in analgesia. NSAIDs vary in how selective they are for COX-1 and COX-2 pathways. This selectivity can vary according to dose. The degree of selectivity for COX-1 relative to COX-2 can be used to classify NSAIDs 2: Non-selective e.g. ibuprofen, naproxen, aspirin Preferential COX-1 inhibitors e.g. indomethacin, ketorolac Preferential COX-2 inhibitors e.g. diclofenac, etodolac, meloxicam The above 3 classes are regarded as ‘NSAIDs’ for the purposes of this guideline. Selective COX-2 inhibitors(coxibs) 4 Figure 1: Non-Steroidal Anti-Inflammatory Drugs 2 What adverse effects of NSAIDs/selective COX-2 inhibitors should we be concerned about? Adverse effects include: Upper gastrointestinal complications: Dyspepsia Ulcer Perforation Obstruction Bleeding Cardiovascular and renal complications: Myocardial infarction Stroke Cardiac failure Hypertension Renal impairment Platelet inhibition: Prolonged bleeding Hepatotoxicity 5 These guidelines focus on the evidence relating to the use and/or side effects of NSAIDs/selective COX-2 inhibitors with respect to gastrointestinal bleeding, co-administration with corticosteroids, aspirin, anti-coagulants, bronchospasm/asthma, heart and renal failure and thrombotic events. We also include reviews of the evidence relating to cancer-induced bone pain and subcutaneous ketorolac. References 1. Mamdani M et al. Observational study of upper gastrointestinal haemorrhage in elderly patients given selective cyclo-oxygenase-2 inhibitors or conventional non-steroidal anti-inflammatory drugs. British Medical Journal 2002; 325: pp. 624-629 2. Neal MJ (ed). Medical Pharmacology at a Glance, fifth edition. Oxford: Blackwell Publishing, 2005 3. Twycross R and Wilcock W (eds). Palliative Care Formulary third edition. Nottingham: Palliativedrugs.com Ltd, 2007. 6 SUMMARY NSAIDs/selective COX-2 inhibitors and Gastro-Intestinal (GI) bleeding 1. Ibuprofen is probably the ‘safest’ NSAID. 4,5,6,7 2. Selective COX-2 inhibitors increase the risk of developing upper GI bleeding complications less than NSAIDs. The absolute risk reduction is 0.4%. 8 3. Individuals at a particularly high risk of upper GI bleeding or perforation have most to gain (in terms of risk reduction) from receiving a selective COX-2 inhibitor compared to a traditional NSAID. 4. No particular selective COX-2 inhibitor has any superiority over another 8 when it comes to reducing the risk of GI bleeding. 5. Celecoxib poses less of a GI risk than ibuprofen 2400 mg/day 8 but the evidence for this superiority is less robust with ibuprofen doses up to 2400 mg/day. 5 6. Ketorolac has the highest risk of causing GI bleeding and so unless this is not a relevant issue e.g. in the case of an imminently dying patient, it should only be used when other NSAIDs are ineffective (see subcutaneous ketorolac section page 69). 7. Gastroprotection with a proton pump inhibitor (PPI) should be considered unless the patient is under 45 with no other risk factors and is likely to be using an NSAID for short-term use e.g. less than 1 month. 8. Any NSAID or selective COX-2 inhibitor should be used at the lowest effective dose and for the shortest duration. 11 9. Avoid modified release (M/R) preparations if possible. NSAIDs/selective COX-2 inhibitors and corticosteroids 1. If at all possible avoid co-prescribing steroids and NSAIDs especially if other risk factors are present, as risks appear to be cumulative. 6,9,10 2. If we take the baseline incidence of upper GI complications (UGIC) necessitating hospitalisation in the general population as one per thousand persons per year 10, according to this study: o In those receiving steroid alone, relative risk is increased to ≈2 events o In those receiving NSAIDs alone, relative risk is increased to ≈4 events o In those receiving both steroids and NSAIDs, relative risk is increased to ≈8 events o The cumulative risk of UGIC events in patients receiving steroids, NSAIDs, aspirin and full dose paracetamol is ≈18 events per thousand persons per year 3. If needing to co-prescribe, ensure steroid dose is as low as possible for the shortest length of time. 4. Steroid use may mask clinical signs and symptoms of serious gastrointestinal complications such as gastro-intestinal perforation. Tachycardia may be the predominant clinical sign and pain/peritonism may be absent. 7 7 5. No specific evidence exists for which NSAID or type of gastroprotection to use when co-prescribing with steroids so the prescriber should prescribe an appropriate NSAID tailored to that individual’s circumstances together with a PPI. NSAIDs/selective COX-2 inhibitors and aspirin 1. If a patient requires both aspirin and a NSAID, ibuprofen and celecoxib are the agents found to place the patient under the lowest level of additional GI bleeding risk. 4,5 2. Clinical Knowledge Summaries recommend adding in a proton pump inhibitor rather than switching to clopidogrel for patients who are on aspirin and NSAIDs. 6,7. NSAIDs/COX-2 inhibitors and warfarin/Low Molecular Weight Heparin (LMWH) 1. NSAIDs and selective COX-2 inhibitors have the potential to interact with warfarin resulting in an increased bleeding time as measured by the INR. 1,13,14 2. There is less robust evidence of the increased risk of interaction with warfarin in the case of the older NSAIDs, in particular nabumetone. 1 3. There is no evidence to suggest that patients anti-coagulated on LMWH are less at risk of alteration in the bleeding time compared to patients on warfarin if they are commenced on NSAIDs. 4. For patients on anticoagulant therapy NSAIDs/COX-2 inhibitors should be introduced with caution and the INR (for patients on warfarin) monitored after the initiation of the drug or alteration of the dose. NSAIDs/selective COX-2 inhibitors and bronchospasm/asthma 1. Anyone with a history of an asthmatic reaction to aspirin or another NSAID or if they have high risk features (severe asthma, nasal polyps, urticaria or chronic rhinitis) should avoid all products containing aspirin or NSAIDs. 1 2. If an NSAID is absolutely necessary, use of a selective COX-2 inhibitor should be preferentially considered which should be given under medical supervision. 4 3. NSAID-naïve asthmatic patients can take an NSAID but they need to be aware of potential risks and advised if a respiratory reaction occurs they must stop treatment and seek medical help. As aspirin-induced asthma can develop in asthmatics > 40 years old, it has been suggested that this group avoid NSAIDs, be warned of the risks and that if NSAIDs are absolutely necessary that the first dose be taken under medical supervision. 1 8 NSAIDS/selective COX-2 inhibitors and heart failure 1. They should not be used in patients with severe heart failure and should be used with caution in those with a history of cardiovascular disease or risk factors for cardiovascular disease as they are at higher risk of developing heart failure. 3 2. They should be used with caution in the elderly [>65] even in the absence of other risk factors, as there is a greater risk of developing heart failure. 3. There is little evidence to show that any one drug has lower risk factors for cardiac failure than any other, but celecoxib seems to pose a similar degree of risk as traditional NSAIDs. 2,4,5,6 4. NSAIDs with a longer half-life (such as naproxen) and controlled release preparations may have an increased risk of causing heart failure. 3 These should be avoided in high-risk patients. NSAIDs/selective COX-2 inhibitors and thrombotic events 1. As NSAIDs and selective COX-2 inhibitors excluding naproxen are associated with an increased risk of cardiovascular thrombotic events 1,2,3,4,5 their use for palliative care patients depends on a balance of risks and benefits. 2. Naproxen appears to carry the lowest risk of increasing cardiovascular events 1,5 and may be the most suitable for patients at higher risk of cardiovascular disease. 3. A second option would be ibuprofen up to 1200mg daily. 4. Avoid diclofenac. 5. Use celecoxib at doses of 200 mg/day or less. NSAIDs/selective COX-2 inhibitors and renal impairment 1. Avoid NSAIDs or COX-2 inhibitors if possible in patients with renal impairment. 2. Celecoxib is overall the safest agent to use. 1,5,6,7 3. Ibuprofen seems to be the safest traditional NSAID. 1,5,6,7 4. Changes in renal function are higher with cumulative dose 1,2, but changes in renal function can be seen up to and beyond 6 months of initiating therapy. 3,4 5. Particular care is needed when prescribing for patients with low circulating volumes [congestive cardiac failure/diuretic therapy]. 3,4 9 The use of NSAIDs/selective COX-2 inhibitors for Cancer-Induced Bone Pain (CIBP) 1. There is some evidence that using an NSAID for bone pain secondary to metastatic cancer can have an analgesic effect and reduce the opioid requirement. 3 2. There is conflicting evidence as to whether NSAIDs/selective COX-2 inhibitors have a clinically meaningful adverse effect on bone healing. 9 Subcutaneous ketorolac 1. S/c ketorolac may improve pain even when oral NSAIDs haven’t. 2. Despite ketorolac being used for up to 6 months without any adverse effects 7, elderly people, patients with GI cancer and patients receiving other drugs which increase the risk of bleeding/renal failure are particularly at risk. 1,2,6,7 If appropriate, renal function should be monitored and ketorolac used at the lowest effective dose and for the shortest duration possible. 3. Gastroprotection (a PPI) should be co-administered if appropriate. 10 NSAIDs/selective COX-2 inhibitors and Gastro-Intestinal (GI) bleeding Q.1 How do these drugs cause GI bleeding? They damage the GI mucosa by topical and systemic actions: Absorption across the gastric mucosa causes direct injury to the epithelium. Systemic effects occur through the inhibition of COX-1. In the gastroduodenal mucosa COX-1 produces prostaglandins which protect the mucosal lining from injury by the luminal acid pepsin.1 Factors contributing to GI risks Many studies looking at GI side-effects specifically exclude people with conditions such as coagulopathies, cancer, chronic liver disease or a history of alcoholism. Where the patient has additional risk factors for GI bleeding their risk may therefore be higher than that found in the study population. Comorbid conditions such as cardiovascular disease, diabetes and renal impairment also increase the risk of GI bleeding. Many other drugs also increase the risk of GI bleeding including aspirin, anticoagulants, corticosteroids and selective serotonin reuptake inhibitors (SSRIs). Treatment should be individualised as the benefit/burden of commencing a NSAID will vary according to each patient’s circumstances. - Age Non-users of NSAIDs are thought to have an estimated rate of 1 occurrence of serious gastrointestinal ulcer complication (perforation or bleeding) per 1,000 persons/year. 2 This increases with age with one study finding a rate of 2.2 upper GI haemorrhages per 1000 persons/year in people aged 66 or over. 3 11 Compared to non-users of NSAIDs, the relative risk of upper GI bleeding, perforation or other serious upper GI tract events resulting in hospitalisation is increased across all age groups and rises with age 4: Graph from Bandolier - Past history A past history of a bleeding/perforated peptic ulcer significantly increases the risk of the above events in the order of 15-fold. 4 A past history of an ulcer also increases the risk, but by a lesser extent. 4 - Dose The risk of developing an upper GI bleeding event increases with increased daily dose of the NSAID (see below). Q.2 Short-acting and long-acting agents – is there any difference in risk? Yes. Slow-release formulations and those drugs with longer half-lives are associated with a higher risk of bleeding due to a more sustained inhibition of cyclo-oxygenase. 5 Drugs with longer half-lives include naproxen, sulindac and meloxicam. 5 Q.3 What about duration of use and its effect on risk? There are differences in opinion between epidemiological studies and some authors think this is probably due to methodological problems such as uncontrolled confounding. Because of ‘self-selection’ (only patients who can tolerate NSAIDs will remain on treatment) or measures taken to reduce gastrotoxicity, patients on long-term NSAIDs probably have lower risks than those recently starting treatment. One study has tried to clarify this – but found the same phenomenon. 6 12 Q.4 Are any NSAIDs less risky than others? Yes and broadly speaking similar hierarchies have been demonstrated although levels of risk vary 4,5,6,7 (see reference section). Q.5 Are selective COX-2 inhibitors any safer? Taking a selective COX-2 inhibitor increases the risk of developing upper GI bleeding complications by a lower amount than traditional NSAIDs 8 and this is also dose-dependent. Broadly speaking: compared with non-use, NSAIDs increase risk 3-4 times, selective COX-2 inhibitors 2-3 and the risk reduction increase may be even greater in high-risk patients. 5 Q.6 Which NSAID is the most gastrotoxic? Ketorolac. 4,9 Q.7 Gastroprotection – what and who for? People younger than 45 and at low risk of GI adverse events (e.g no history of GI bleeding or Helicobacter Pylori infection and not on aspirin, warfarin or corticosteroids may not need a gastroprotective drug.10 A proton pump inhibitor (PPI) is the preferred choice of gastroprotective drug. 10 PPIs reduce ulcer recurrence and prevent ulcer development in previously ulcer-free at-risk patients on chronic NSAIDs. 1 Conclusions and recommendations 1. Ibuprofen seems to be the ‘safest’ traditional NSAID. 4,5,6,7 2. The dose of the intended NSAID may affect the risk profile and if we take the Richy study 6 as the strongest evidence, meloxicam may be slightly less toxic than diclofenac/naproxen, although overall the differences are small between all the commonly used NSAIDs. 3. Selective COX-2 inhibitors increase the risk of developing upper GI bleeding complications by a lower amount than NSAIDs . The absolute risk reduction is 0.4%. 8 4. Individuals at a particularly high risk of upper GI bleeding or perforation have most to gain (in terms of risk reduction) from receiving a selective COX-2 inhibitor compared to a traditional NSAID. 5. No particular selective COX-2 inhibitor has any superiority over another when it comes to reducing the risk of GI bleeding. 8 13 6. Celecoxib poses less of a GI risk than ibuprofen 2400 mg/day 8 but the evidence for this superiority is less robust with respect to ibuprofen doses up to 2400 mg/day. 5 7. Ketorolac has the highest risk of causing GI bleeding and so unless this is not a relevant issue e.g. in the case of an imminently dying patient, it should only be used when other NSAIDs are ineffective (see subcutaneous ketorolac section page 69). 8. Gastroprotection with a PPI should be considered unless the patient is under 45 with no other risk factors and is likely to be using an NSAID for short-term use 10 e.g less than 1 month. 9. Any NSAID/selective COX-2 inhibitor should be used at the lowest dose and for the shortest duration. 11 10. Avoid M/R preparations if possible. 5 14 References Cross-sectional and retrospective analyses are more likely to over-estimate risks compared with RCTs and longitudinal cohort studies because RCTs can more accurately control for confounding factors and bias. Smaller studies (e.g. with < 1000 participants) can produce relative risks that demonstrate variability when these studies are compared to each other. Q.1 How do NSAIDs cause GI bleeding? 1. Schlansky B & Hwang J. Prevention of nonsteroidal anti-inflammatory drug-induced gastropathy. Journal of Gastroenterology 2009; 44 (S19) pp. 44-52 Review 2. Hernandez-Diaz S & Garcia Rodriguez L. Incidence of serious upper gastrointestinal bleeding/perforation in the general population: Review of epidemiologic studies. Journal of Clinical Epidemiology 2002; 55: pp. 157163 Review 3. Mamdani M et al. Observational study of upper gastrointestinal haemorrhage in elderly patients given selective cyclo-oxygenase-2 inhibitors or conventional non-steroidal anti-inflammatory drugs. British Medical Journal 2002; 325: pp. 624-629 Level of evidence: 2++ Population based retrospective cohort study with subjects aged ≥ 66 years Controls numbered 100,000 Study duration was 1 year Unable to control for smoking and alcohol consumption 4. Hernandez-Diaz S & Garcia Rodriguez L. Association between Nonsteroidal Anti-inflammatory Drugs and Upper Gastrointestinal Tract Bleeding/Perforation. Archives of Internal Medicine 2000; 160: pp. 20932099 Level of evidence: 2++ Pooled meta-analysis of 18 case-control/cohort studies on non-aspirin NSAID use and severe upper GI bleeding events 15 Analysed to compare NSAID use with non-use and to generate RR Didn’t include patients on COX-2 inhibitors. All but 2 studies attempted to control for potential confounders such as age It found variable risks associated with individual NSAIDS (different studies used different doses to define low/medium/high doses) – see graph below Ibuprofen being least harmful at doses below 2400 mg/day (RR 2.1, 95% CI 1.6-2.7) Low-medium dose diclofenac ( ≤ 100 mg or ≤ 75 mg) had a slightly lower RR (3.1, 95% CI 2.0-4.7) than low-medium dose naproxen (≤ 1000mg or ≤ 750 mg) which had a RR of 3.5 (95% CI 2.8-4.3) High dose diclofenac had a lower RR than both high dose ibuprofen and naproxen: o High dose diclofenac: RR 3.6 (95% CI 2.3-5.6) o High dose naproxen: RR 5.1 (95% CI 3.8-6.9) o High dose ibuprofen: RR 5.5 (95% CI 3.0-10.00) Low-medium doses of the NSAIDs were associated with relative risks of 2-4. Graph from Bandolier Q.2 Short-acting and long-acting agents – is there any difference in risk? 5. Garcia Rodriguez L and Tolosa L. Risk of Upper Gastrointestinal Complications Among Users of Traditional NSAIDs and COXIBs in the General Population. Gastroenterology 2007; 132: pp. 498-506 Level of evidence: 2++ Retrospective population based cohort study with a nested casecontrol analysis Cohort derived from UK patients on a GP database Aged 40-85 – excluded cancer, coagulopathies, liver and alcohol disorders 1561 cases and 10,000 controls Estimates of RR adjusted for peptic ulcer disease, smoking, alcohol, steroids, aspirin, warfarin Calculated RR of upper GI bleeding/perforation of traditional NSAIDs and COXIBs compared to non-use 16 The RR for each drug was not specified but was represented graphically. This has made accurate interpretation of the results difficult 95% CI for the RRs weren’t specified but were diagrammatically illustrated in the paper. Etoricoxib had extremely wide confidence intervals at both dose ranges. Low/medium doses: o Ibuprofen had the lowest RR (approx 2) o Meloxicam and indomethacin next lowest (wider CI for indomethacin) o Then celecoxib and diclofenac - comparable RRs o Then naproxen (around 4) o Etoricoxib had the highest RR of approx 10 High doses: Ibuprofen lowest RR Then Celecoxib Then Diclofenac Then Naproxen Then Indomethacin Then Etoricoxib Q.3 What about duration of use and its effect on risk? 6. Richy F et al. Time dependent risk of gastrointestinal complications induced by non-steroidal anti-inflammatory drug use: a WHO consensus statement using a meta-analytic approach. Annals of Rheumatic Diseases 2004; 63: pp. 759-766 Level of evidence: 1+ RCTs and controlled cohort studies were identified between 1985 and 2003 Oral preparations and had to be given for at least 5 days Didn’t include patients on selective COX-2 inhibitors Eventually 32 RCTs and 13 major cohort studies were identified with duration of treatment ranging from 5-1825 days In the RCTs patients had to be matched at inclusion for age, sex and history of GI events and most of the cohort studies matched for age and sex Median daily doses were: ibuprofen 1200 mg, naproxen 875 mg, diclofenac 150 mg, etodolac 800 mg, indomethacin 75 mg, meloxicam 15 mg, piroxicam 20 mg 17 Meta-regression analysis shows that the maximum level of risk appears at 50 days of treatment for non-indomethacin NSAIDs, then begins to decrease Seven NSAIDs were investigated more than others in RCTs (see above for median doses) and this meta-analysis showed that compared to placebo or non-exposed group: o o o o o o Ibuprofen had the lowest RR =1.19 (95% CI 0.93-1.54) Meloxicam RR=1.24 (95% CI 0.98-1.56) Piroxicam RR=1.66 (95% CI 1.14-2.44) Diclofenac RR=1.73 (95% CI 1.21-2.46) Naproxen RR=1.83 (95% CI 1.25-2.68) Indomethacin RR=2.25 (95% CI 1.10-5.07) Q.4 Are any NSAIDS less risky than others? See also references 2 and 4. 7. Lewis S et al. Dose-response relationships between individual nonaspirin nonsteroidal anti-inflammatory drugs and serious upper gastrointestinal bleeding: a meta-analysis based on individual patient data. British Journal of Clinical Pharmacology 2002; 54: pp. 320-326 Level of evidence: 2++ Pooled results from 3 case-control studies All studies included patients experiencing acute upper GI haemorrhage All patients matched for age and sex All studies excluded patients with gastric carcinoma. Didn’t include patients on selective COX-2 inhibitors Doses of NSAIDs were coded as low, medium or high based on dose ranges recommended in the BNF. It also found dose-response relationships (expressed as odds ratios), summarised as: Low doses: o o o o o ibuprofen (<1200 mg) OR 1.1 (95% CI 0.6-2.0) diclofenac (<75 mg) OR 2.2 (95% CI 0.8-5.8) indomethacin (≤50 mg) OR 3.2 (95% CI 1.1-9.5) naproxen (< 500 mg) OR 4.8 (95% CI 1.3-18.1) piroxicam (≤ 10 mg) OR 9.0 (95% CI 2.1-39.2) Medium doses: o ibuprofen (1200-1799 mg) OR 1.8 (95% CI 0.8-3.7) 18 o o o o diclofenac (75-149 mg) OR 3.2 (95% CI 1.9-5.5) naproxen (500-999 mg) OR 5.4 (95% CI 2.9-9.9) indomethacin (51-149 mg) OR 6.8 (95% CI 3.6-12.9) piroxicam (11-20 mg) OR 12 (95% CI 6.5-22.1) High doses: o o o o o ibuprofen (≥ 1800 mg) OR 4.6 (95% CI 0.9-22.3) diclofenac (≥ 150 mg) OR 12.2 (95% CI 5.6-26.7) naproxen (≥ 1000 mg) OR 15.6 (95% CI 8.1-30.2) indomethacin (≥ 150 mg) OR 20.4 (95% CI 4.2-99.7) piroxicam (≥ 21 mg) OR 79 (95% CI 9.9-631.8) Q.5 Are COX-2 inhibitors any safer? See also reference 3. 8. Rostom A et al. Gastrointestinal Safety of Cyclo-Oxygenase-2 Inhibitors: A Cochrane Collaboration Systematic Review. Clinical Gastroenterology and Hepatology 2007; 5: pp. 818-828 Level of evidence: 1++ Systematic review of RCTs assessing the upper GI harms of greater than 4 weeks use of COX-2s (celecoxib, etoricoxib, valdecoxib, lumiracoxib) compared with non-selective NSAIDs and placebo in arthritis sufferers For ulcer perforation, obstruction or bleeding, an absolute risk reduction of ≈ 0.4% resulted from using COX-2s compared with non-selective NSAIDs Selective COX-2s were statistically superior to naproxen and ibuprofen for the above endpoints. All included studies used ibuprofen 2400 mg/day Celecoxib showed a non-significant trend towards less frequently occurring perforation, obstruction or bleeding episodes compared to diclofenac Authors concluded that COX-2 inhibitors provide better GI safety and found similar results across all types of selective COX-2s Q.6 Which NSAID is the most gastrotoxic? See also reference 2. 9. Garcia Rodriguez L et al. Risk of Hospitalisation for Upper Gastrointestinal Tract Bleeding Associated with Ketorolac, Other Nonsteroidal Anti-inflammatory Drugs, Calcium Antagonists and Other Antihypertensive drugs. Archives of Internal Medicine 1998; 158: pp. 3339 19 Level of evidence: 2++ Prospective case-control cohort study of 1505 patients; patients followed up until they were hospitalised for an upper GI bleed/perforation Ketorolac was either oral or IM; IM was associated with a higher risk than oral Q.7 Gastroprotection – what and who for? See also reference 1. 10. Clinical Knowledge Summaries. NSAIDs – prescribing issues. [Online]. Available from: http://cks.library.nhs.uk [Accessed 31 August 2009]. Included in recommendations 11. Medicines and Healthcare Products Regulatory Agency. Drug Safety Update. 2007; Volume 1 Issue 3 [Online]. Available from: http://www.mhra.gov.uk/Publications/Safetyguidance/DrugSafetyUpdate [Accessed 31 August 2009}. 20 NSAIDs and steroids Steroids and gastrointestinal complications Corticosteroids are specific COX-2 inhibitors 1 and may contribute to the delayed healing of gastric erosions caused by NSAIDs 2 Evidence suggests that there is a low incidence of major gastrointestinal complications associated with corticosteroid monotherapy and there is conflicting evidence with regard to any dosedependent increased risk of ulceration in steroid-treated patients 2,3,4,5,6 Q.1 What are the risk factors for gastrointestinal complications with steroids? Drawing definite conclusions regarding risk factors associated with corticosteroids and peptic ulcers from limited studies is very difficult. The paucity of work in some areas provides too little data for meaningful interpretation and comparison of studies is difficult due to lack of uniform diagnostic criteria and varying exclusion criteria. 2 Total dose of steroid: o Increasing dose of steroid may be associated with an increased risk of perforations/peptic ulcers and different studies quote different steroid doses at which there is an association 3,4,5,6,7 (Note that 5mg prednisolone ≡ 0.75mg dexamethasone). Previous history of peptic ulcer: o Increases the risk of peptic ulceration 3 Advanced malignancy: o May increase the risk of developing a peptic ulcer 8 Concurrent prescribing of NSAIDs: o Evidence suggests that the incidence of peptic ulcers/haemorrhages is higher in people who are taking both NSAIDs and steroids 6,9,10 Length of time on steroids and NSAID: o Possibly an increased risk if on both for longer than 90 days but few papers address this directly. 21 9 Conclusions and recommendations 1. If at all possible avoid co-prescribing steroids and NSAIDs especially if other risk factors are present, as risks appear to be cumulative. 6,9,10 2. If we take the baseline incidence of upper GI complications (UGIC) necessitating hospitalisation in the general population as one per thousand persons per year 10, according to this study: In those receiving steroid alone, relative risk is increased to ≈2 events In those receiving NSAIDs alone, relative risk is increased to ≈4 events In those receiving both steroids and NSAIDs, relative risk is increased to ≈8 events The cumulative risk of UGIC events in patients receiving steroids, NSAIDs, aspirin and full dose paracetamol is ≈18 events per thousand persons per year 3. If needing to co-prescribe, ensure steroid dose is as low as possible for the shortest length of time. 4. Steroid use may mask clinical signs and symptoms of serious gastrointestinal complications such as gastro-intestinal perforation. Tachycardia may be the predominant clinical sign and pain/peritonism may be absent. 7 5. No specific evidence exists for which NSAID or type of gastroprotection to use when co-prescribing with steroids. 6. See also the guidance in the Gastrointestinal Bleeding section (page 11). 22 References Steroids and gastrointestinal complications 1. Dickman A & Ellershaw J. NSAIDS: gastroprotection or selective COX2 inhibitor. Palliative Medicine 2004; 18: pp. 275-286. 2. Ellershaw JE & Kelly MJ. Corticosteroids and peptic ulceration. Palliative Medicine 1994; 8: pp. 313-319. Review articles 3. Conn HO & Blitzer BL. Medical progress: non association of adrenocorticosteroid therapy and peptic ulcer. New England Journal of Medicine 1976; 294: pp. 473-479. Level of evidence: 1 Analysis of 26 prospective RCTs (3558 cases) and 16 prospective controlled non double-blinded investigations (1773 cases). Study design has been criticised by other researchers Frequency of peptic ulcer was slightly higher in steroid group but not statistically significant. Neither haemorrhage nor perforation from ulcer occurred significantly more often in the steroid group compared to the placebo group. . Patients with a previous history of peptic ulcer had a significantly higher risk of peptic ulcer perforation if on steroids 0.1% vs 4.8%, (p<0.001). While greater than 20 mg prednisolone/day was not associated with a significantly higher risk of developing a peptic ulcer, a total dose of more than 1000 mg prednisolone was 4. Messer J et al. Association of adrenocorticosteroid therapy and pepticulcer disease. New England Journal of Medicine 1983; 309: pp. 21-24. Level of evidence: 1 Meta-analysis of pooled data from 71 controlled trials (not all were double-blind) Studies were excluded if patients received antacids Study design has been criticised by other researchers The overall incidence of diagnosed ulcers was 1.8 % in the steroidtreated patients and 0.8% in the controls (p<0.001), RR 2.3 (CI 1.4-3.7) 23 There was a higher rate of haemorrhage from ulcers in the steroid group, although this did not reach statistical significance The incidence of ulcers was significantly increased even if patients received steroids for less than 1 month and in those receiving a total dose of less than 1000 mg prednisolone 5. Conn HO & Poynard T. Corticosteroids and peptic ulcer: meta-analysis of adverse events during steroid therapy. Journal of Internal Medicine 1994; 236: pp. 619-632. Level of evidence: 1+ Meta-analysis of 93 double-blind RCTs Patients received a mean dose of 35 mg (or equivalent) of prednisolone for a mean duration of 64 days Of 3267 patients in the control (non-exposed) group, 0.3% developed ulcers and in the study group 13 out of 3335 (0.4%) did. This was not statistically significant. There were no statistically significant differences in the rates of perforation/haemorrhage Although the incidence of peptic ulcer increased with increasing duration of therapy, the differences did not become statistically significant ‘Symptoms of peptic ulcer’ (undefined by authors) did occur more frequently in the steroid group which was statistically significant. 6. Rodríguez L & Hernández-Díaz S. The risk of upper gastrointestinal complications associated with nonsteroidal anti-inflammatory drugs, glucocorticoids, acetaminophen, and combinations of these agents. Arthritis Research 2001; 3: pp. 98–101. Review article examining a nested case control study involving 958,000 patients age 40-79 years Study population excluded those with cancer Study didn’t look at COX-2 inhibitors 852 patients meeting criteria matched to 6768 controls Estimates of RR adjusted for age, smoking and concomitant medications including omeprazole and anticoagulants The risk of upper GI complications (bleeding or perforation) (UGIC) was 2.1 (95% CI 1.4–3.0) times higher for current users of steroids than for non-users (expressed as RR) Addition of corticosteroid increased the RR of peptic ulcer or ulcer complication from 3.6 (95% CI 2.9 - 4.3) in those receiving NSAID monotherapy to 8.5 (95% CI 3.9 - 18.9) in those on NSAID and steroid 24 So if we take the baseline incidence of UGIC events necessitating hospitalisation in the general population as one per thousand persons per year10 , according to this study: o In those receiving steroid alone, relative risk is increased to ≈2 events o In those receiving NSAIDs alone, relative risk is increased to ≈4 events o In those receiving both steroids and NSAIDs, relative risk is increased to ≈8 events o The cumulative risk of UGIC events in patients receiving steroids, NSAIDs, aspirin and full dose paracetamol is ≈18 events per thousand persons per year Q.1 What are the risk factors for gastrointestinal complications with steroids? See also references 2,3,4,5,6. 7. Dayton MT, Kleckner SC, Brown DK et al. Peptic ulcer perforation associated with steroid review. Archives of Surgery 1987; 122: pp. 376380. Level of evidence: 3 10-year retrospective chart review of hospital patients who had had steroid treatment within 1 week of peptic ulcer perforation 17% of peptic ulcer perforations during this period were associated with steroid use (25 patients), mean age 45 years Only 36% of patients with steroid-associated perforations were receiving antacid prophylaxis Mean dose of corticosteroid at time of perforation was 14mg dexamethasone (or equivalent) 8. Schell HW. Adrenal corticosteroid therapy in far advanced cancer. Geriatrics 1972; 27: pp. 131-141 Level of evidence: 3 Post-mortem case series showing that a higher proportion of peptic ulcers were present in patients dying of cancer who received steroids (for at least 2 weeks) compared to those who did not (10% in steroid group compared to 3% in no-steroid group). This study did not mention NSAID prescribing. 5% of group who had received steroids had a complicated peptic ulcer contributing to death compared to 1% in the group not receiving steroids. 9. Piper J, Ray W, Daugherty J, Griffin M. Corticosteroid Use and Peptic Ulcer Disease: Role of Nonsteroidal Anti-inflammatory Drugs. Annals of Internal Medicine 1991; 114: pp. 735-740. 25 Level of evidence: 2++ Retrospective case-control study of 1415 patients over the age of 65 who were hospitalised with a confirmed gastric or duodenal ulcer or an episode of gastrointestinal haemorrhage. Analysis compared the risk of developing peptic ulcer disease in patients taking both NSAIDS and steroids with those on neither drug and calculated an estimated RR of 14.6 (CI 6.7 - 32.0) Increasing duration of NSAID use (more than 90 days) was associated with a higher RR of peptic ulcer disease, compared to non-use 10. Hernandez-Diaz S & Garcia Rodriguez L. Incidence of serious upper gastrointestinal bleeding/perforation in the general population: Review of epidemiologic studies. Journal of Clinical Epidemiology 2002; 55: pp. 157-163 26 NSAIDs/selective COX-2 inhibitors and aspirin This section looks at which NSAID is best to prescribe for a patient on aspirin with respect to the risk of causing gastrointestinal (GI) bleeding. Q.1 How is aspirin different to NSAIDs? Aspirin is a salicylate and suppresses the production of prostaglandins and thromboxane A2 due to its irreversible inactivation of the COX-1 enzyme 1 (see Figure 1 page 5). This is different from other NSAIDs, such as diclofenac and ibuprofen, which are reversible inhibitors. Low-dose, long-term aspirin use irreversibly blocks the formation of thromboxane A2 in platelets, producing an inhibitory effect on platelet aggregation. This makes aspirin useful for reducing the incidence of heart attacks but also makes patients more prone to bleeding. 1,2,3 Enteric coated formulations/ modified release formulations of aspirin do not modify the effect on GI bleeding. 3 Q.2 Which NSAID should I prescribe for a patient taking aspirin? Evidence suggests that ibuprofen is the NSAID with the lowest associated risk of GI bleeding; celecoxib is slightly higher. 4,5 Risk varies with different NSAIDs 4 (see table 1, page 29). Q.3 Should I switch aspirin to clopidogrel when adding in NSAIDs? There is no evidence to guide practice when adding in NSAIDs to patients taking aspirin. There is evidence showing that the risk of GI bleeding is significantly lower when aspirin is used with a proton pump inhibitor (PPI) rather than switching to clopidogrel. 6,7 Recommendations 1. If a patient requires both aspirin and a NSAID, ibuprofen and celecoxib are the agents found to place the patient under the lowest level of additional GI bleeding risk. 4,5 2. Clinical Knowledge Summaries recommend adding in a PPI rather than switching to clopidogrel for patients who are on aspirin and NSAIDs. 6,7 27 References Q.1 How is Aspirin different to NSAIDs? 1. Neal MJ (ed). Medical Pharmacology at a Glance, fifth edition. Oxford, Blackwell Publishing, 2005 2. Loeb S, Klusek H & Blake G (eds). Nursing students guide to drugs, first edition. Springhouse, Pennsylvania, Springhouse Corporation, 1993. 3. Derry S & Loke Y. Risk of gastrointestinal haemorrhage with long term use of aspirin: meta-analysis. British Medical Journal 2000; 321: pp. 11831187 Level of evidence: 1++ Meta Analysis 24 RCTs with ≈ 66,000 patients Included a sub-analysis of ≈ 50,000 patients taking doses of aspirin ranging from 50-162.5 mg/day for a mean duration of 28 months GI haemorrhage occurred in 2.3% of patients taking aspirin compared with 1.45% taking placebo (pooled OR 1.59, 95% CI 1.4-1.8, p<0.0001) NNH/year = 248 for doses 50-1500 mg/day Q.2 Which NSAID should I prescribe for a patient taking aspirin? 4. Rahme E, Nedjar H, Bizzi A & Morin S. Hospitalization for gastrointestinal adverse events attributable to the use of low-dose aspirin among patients 50 years or older also using non-steroidal anti-inflammatory drugs: a retrospective cohort study. Alimentary Pharmacology and Therapeutics 2007; 26 (10): pp. 1387-1398 Level of evidence: 2++ Retrospective cohort study Over 1.5 million people on combinations of NSAIDs and aspirin Median daily dose of ibuprofen was 1600 mg, naproxen 750 mg and celecoxib 200 mg Only 29% were taking aspirin ≤ 81 mg/day There were much lower numbers of prescriptions for piroxicam and ibuprofen issued during the study period which may have biased the results Adjusted data to take account of patients already on a proton pump inhibitor Factors associated with a higher rate of bleeding included previous ulcers, heart and renal failure 28 Table 1: Association between COX-2 inhibitors, Non selective-NSAIDs and acetaminophen and hospitalization for upper GI events Hazard ratios and 95% CI for upper GI bleeding when compared to people on paracetamol (acetaminophen) - the overlapping confidence intervals for naproxen, piroxicam and ibuprofen suggest that coincident use of aspirin does not change the bleeding risk with these agents. However, bleeding risks with diclofenac and celecoxib are approximately doubled when aspirin is used concomitantly. Drug No aspirin With aspirin Naproxen 2.5 (2.1-3.0) 2.2 (1.6-3.0) Piroxicam 1.8 (0.8-2.8) 2.0 (0.8-5.4) Diclofenac 1.5 (1.2-1.7) 2.8 (2.2-3.5) Ibuprofen 0.9 (0.6-1.4) 1.4 (0.8-2.7) Celecoxib 0.7 (0.6-0.8) 1.8 (1.5-2.1) 5. Rahme E, Bardou M, Dasgupta K et al. Hospitalization for gastrointestinal bleeding associated with non-steroidal anti-inflammatory drugs among elderly patients using low-dose aspirin: a retrospective cohort study. Rheumatology 2007; 46: pp. 265-272 Level of evidence: 2Retrospective cohort study of ≈ 332,000 patients ≥ 66 years Compared patients on celecoxib and aspirin with those on nonselective NSAIDs and aspirin Naproxen accounted for 24% of all non-selective NSAIDs Median aspirin dose was 325 mg/day with 23% using 80 mg/day Celecoxib and aspirin was associated with a lower rate of admission for gastrointestinal bleeding compared to nonselective NSAIDs and aspirin (hazard ratio 1 compared to 1.6) 29 Q.3 Should I switch aspirin to clopidogrel when adding in NSAIDs? 6. Chan FKL, Ching JYL, Hung LCT et al. Clopidogrel versus aspirin and esomeprazole to prevent recurrent ulcer bleeding. New England Journal of Medicine 2005; 352(3): pp. 238-244 Level of evidence: 1+ Double-blind prospective RCT 320 high-risk patients, average age 72 years, with proven past history of aspirin-induced ulcer bleeding Fully healed ulcers at time of inclusion Randomised to receive either clopidogrel 75 mg plus esomeprazole placebo or aspirin 80 mg/day plus esomeprazole 20 mg bd Followed for 12 months Clopidogrel group: 8.6% had recurrent bleeds Aspirin plus esomeprazole group: 0.7% had recurrent bleeds (p=0.001) 7. Lai KC, Hui WM, Wong BC et al. Esomeprazole with Aspirin Versus Clopidogrel for Prevention of Recurrent Gastrointestinal Ulcer Complications. Clinical Gastroenterology and Hepatology 2006; 4(7): pp. 860-865 Level of evidence: 1+ Double-blind prospective RCT 170 high-risk patients, average age 75 years with proven past history of aspirin-induced ulcer bleeding Fully healed ulcers at time of inclusion Randomised to receive either clopidogrel 75 mg/day or aspirin 100 mg and esomeprazole 20 mg od Followed for a median time of 52 weeks Clopidogrel group: 13.6% incidence of recurrent bleeds Aspirin plus esomeprazole group: 0% (p=0.0019) 30 NSAIDs/selective COX-2 inhibitors and Warfarin/Low Molecular Weight Heparin (LMWH) NSAIDs and platelet function NSAIDs work by reversibly inhibiting cyclo-oxygenase which catalyses the formation of prostaglandins and thromboxanes from arachidonic acid (AA) – see table 1 page 5. Thromboxane A2 is the major product of the AA metabolism in platelets and stimulates vasoconstriction and platelet aggregation. A reduction in thromboxane A2 can cause impaired platelet aggregation. Although NSAIDs inhibit platelet function, bleeding time has been shown to be prolonged by only about 33% in both volunteer and clinical studies and is not associated with haemorrhagic complications. This is because many other agonists including thrombin and collagen can promote platelet activation in the presence of a cyclo-oxygenase inhibitor. Such a modest increase in bleeding time prolongation is unlikely to be of major clinical significance in normal subjects. Nabumetone is thought to have less of an inhibitory effect on platelet aggregation than other NSAIDs. 1 Q.1 Anticoagulants and NSAIDs – does the risk of bleeding increase? Theoretically, several NSAIDs have the potential to displace warfarin from its binding sites on proteins and increase the plasma level of its more pharmacologically active free fraction. 1 Most of the trial evidence does not demonstrate an interaction between NSAIDs and warfarin but these studies used healthy volunteers. 2,3,4,5 Most evidence suggests that nabumetone does not affect the INR of patients on warfarin 1 although a case report to the contrary has been found. 6 Three studies have examined the possible interaction of LMWH and NSAIDs: - Two were in post operative patients 7,8 and concluded that there was no clinically significant increased risk of bleeding postoperatively but caution was advised because of theoretical risk. - One study used healthy volunteers 9 and here ketorolac significantly increased the bleeding time which was then further increased by the addition of dalteparin. Dalteparin alone had no effect on the bleeding time. Case reports of prolonged bleeding times in patients taking both NSAIDs (indomethicin, ketoprofen, piroxicam and sulindac) and anticoagulants have been published. 1 31 Q.2 Is it safer to prescribe a NSAID to a patient being anticoagulated on LMWH than warfarin? There is no evidence to support this. There are no trials comparing the safety of NSAID use in patients on warfarin vs LMWH therapy. Q.3 Is there any difference between traditional NSAIDs and COX-2 inhibitors in their effect on the bleeding time of anticoagulated patients? There is conflicting evidence with regards to the potential of COX-2 inhibitors to interact with warfarin resulting in an increased INR. Trials in healthy volunteers show either no effect or a ‘clinically insignificant effect’ when warfarin is combined with celecoxib 10,11 and etoricoxib 12 One small study in which patients on warfarin were commenced on celecoxib 200 mg/day showed an increase in the INR of > 15 % 13 A case has been reported of an increased INR following the commencement of celecoxib 14 The recommendations from this trial and also from the other trials where a ‘clinically insignificant effect’ direct effect on the INR was noted was that because of potential interactions, bleeding risk and the variability of the non-study healthy volunteer patient, the INR should be monitored when COX-2 inhibitors are initiated or changed. Conclusions 1. Traditional NSAIDs and selective COX-2 inhibitors have the potential to interact with warfarin resulting in an increased bleeding time as measured by the INR. 1,13,14 2. There is less robust evidence of the increased risk of interaction with warfarin in the case of the older NSAIDs, in particular nabumetone. 1 3. There is no evidence to suggest that patients anti-coagulated on LMWH are less at risk of alteration in the bleeding time compared to patients on warfarin if they are commenced on NSAIDs. Recommendation 1. For patients on anticoagulant therapy NSAIDs/selective COX-2 inhibitors should be introduced with caution and INR (for patients on warfarin) monitored after the initiation of the drug or alteration of the dose. 32 References Q.1 Anticoagulants and NSAIDs – does the risk of bleeding increase? 1. Hilleman DE, Mohiuddin SM, Lucas BD. Nonsteroidal Anti-inflammatory Drug Use in Patients Receiving Warfarin; Emphasis on Nabumetone. American Journal of Medicine 1993; 95: (S 2A) Review article and case series Level of evidence: 3 a) Evaluated the addition of nabumetone 1000 mg or 2000 mg/day taken ‘as needed’ b) 58 patients, already stabilised on chronic warfarin c) None had previously taken nabumetone d) No significant differences in INR found after 6 weeks of nabumetone 2. Vesell ES, Passananti TG, Johnson AO. Failure of Indomethacin and Warfarin to Interact in Normal Volunteers. Journal of Clinical Pharmacology 1975; 15: pp. 486-495 Level of evidence: 1+ 2 double-blind, randomised placebo-controlled trials: a) 16 healthy people age 19-28 received warfarin that prolonged their PT to 1.5-2.5 control Administration of indomethacin or placebo failed to alter the PT b) 19 healthy people age 22-27 given loading dose warfarin and PT monitored 20 days later started on either indomethacin or placebo and 11 days later another warfarin dose given and PT monitored No significant differences between indomethacin and placebo with respect to their effects on warfarin induced hypoprothrombinaemia and plasma warfarin half-life 3. Eichler HG, Jung M, Kyrle PA, Rotter M, Korn A. Absence of interaction between tenoxicam and warfarin. European Journal of Clinical Pharmacology 1992; 42: pp. 227-229 Level of evidence: 1Open randomized, cross-over design a) Single dose study 33 8 volunteers given single dose warfarin on 2 separate occasions 4 weeks apart One dose given without tenoxicam, the other following 14 days of it Tenoxicam continued for 1 week after warfarin No significant difference in PT between treatment cycles b) Steady state study 8 people given tenoxicam for 2 weeks and clotting tests done 3 week wash-out period Given warfarin, dose stabilised then given tenoxicam for another 2 weeks Tenoxicam then stopped and warfarin continued for another 4 weeks No changes in clotting results 4. Mieszczak C & Winther K. Lack of interaction of ketoprofen with warfarin. European Journal of Clinical Pharmacology 1993; 44: pp. 205-206 Level of evidence: 1Double-blind, randomised placebo-controlled trial 13 healthy male volunteers, mean age 34, acting as their own controls Ketoprofen given for 7 days after stabilisation on warfarin Ketoprofen did not affect the PT and no clinical evidence of bleeding 5. Fitzgerald D. Nabumetone, a novel anti-inflammatory. Royal Society of Medicine 1985; (Vol 69): pp. 47-52 Level of evidence: 2Double blind, placebo-controlled multi-dose trial 12 volunteers stabilized on warfarin. Placebo or nabumetone for 2 weeks No significant differences in INR, thrombin time or bleeding time 6. Dennis VC, Thomas BK, Hanlon JE. Potentiation of Oral Anticoagulation and Hemarthrosis Associated with Nabumetone. Pharmacotherapy 2000; 20(2): pp. 234-239 Level of evidence: 3 Case report Haemarthrosis in a patient on stable dose warfarin who commenced nabumatone one week earlier and whose INR had increased from 2.1 to 3.7 34 7. Kristensen SS et al. Combined treatment with Indomethacin and Low Dose Heparin After Total Hip Replacement. Journal of Bone and Joint Surgery 1990; 72-B: pp.447-449 Level of evidence: 1Double blind, randomised placebo-controlled trial 235 patients undergoing total hip replacement on prophylactic LMWH from day of surgery Randomised to indomethacin or placebo from day 1 post-op for 6 weeks More post-op bleeding occurred in the indomethacin group but it wasn’t statistically significant The period of heparin treatment was considerably lower in the indomethacin group because of earlier mobilisation 8. Weale AE, Durant N, Warwick DJ, Prothero D. Is there a clinical interaction between low molecular weight heparin and non-steroidal analgesics after total hip replacement? Annals of the Royal College of Surgeons of England 1995; 77: pp. 35-37 Level of evidence: 1Prospective randomised controlled trial 60 patients undergoing total hip replacement - all on enoxaparin postop Any previous NSAID was stopped 4 weeks prior to admission 26 patients given I/M ketorolac pre-op and for 4 days post-op; others randomised to opioid and paracetamol No clinically detectable GI haemorrhage in either group and no differences in wound oozing 9. Greer IA et al. Effect of ketorolac and low-molecular weight heparin individually and in combination on haemostasis. Blood Coagulation and Fibrinolysis 1999; 10: pp. 367-373 Level of evidence: 1 Double blind, randomized, placebo-controlled crossover study 24 healthy male volunteers age 18-48 who avoided aspirin and other NSAIDs for 2 weeks before and during the study Ketorolac with dalteparin studied Minimal interval between treatments 1 week There was no interaction between ketorolac and dalteparin with regards to platelet aggregation, anti-factor Xa activity or activated partial thromboplastin time 35 Ketorolac administration significantly prolonged skin bleeding time and addition of dalteparin enhanced the bleeding time further Authors state that skin bleeding time is not a predictor of surgical bleeding Therefore no evidence to suggest a clinically significant increased risk of bleeding postoperatively with combination of LMWH and NSAIDs but caution advised because of theoretical risk. Q3. Is there any difference between traditional NSAIDs and COX-2 inhibitors in their effect on the bleeding time of anticoagulated patients? 10. Karim A et al. Celecoxib Does Not Significantly Alter the Pharmacokinetic or Hypoprothrombinemic Effect of Warfarin in Healthy Subjects. Journal of Clinical Pharmacology 2000; 40: pp. 655-663 Level of evidence: 1Open label, multiple dose, randomized, placebo-controlled, parallel-group study 24 healthy volunteers age 19-50 given warfarin for 8 days Then randomised to celecoxib 200mg bd or placebo for 7 days while continuing warfarin Prothrombin times (PT) were monitored and did not differ significantly between the 2 groups Celecoxib did not significantly alter the steady-state pharmacokinetics of warfarin There were no adverse bleeding events Authors comment that all participants were ‘normal’ metabolisers of the hepatic enzyme P450 CYP2C9. Genetic variations of this enzyme could result in ‘poor’ metabolisers and hence potential alterations in PT 11. Dentali F et al. Does Celecoxib Potentiate the Anti coagulant Effect of Warfarin? A Randomised, Double-Blind, Controlled Trial. Annals of Pharmacotherapy 2006; 40: pp. 1241-1247 Level of evidence: 1Randomised, double-blind, controlled, crossover trial 15 patients on long-term warfarin, mean age 70 Phase 1: celecoxib 200mg/day or codeine phosphate 3-4 times/day for 5 weeks Phase 2: Swap over, no drug free interval Weekly INR for 10 weeks Celecoxib did not significantly affect the INR although one patient in the celecoxib group was withdrawn from the study when the INR increased from a baseline of 3.6 to 4.9. 36 12. Schwartz JI et al. The Effect of Etoricoxib on the Pharmacodynamics and Pharmacokinetics of Warfarin. Journal of Clinical Pharmacology 2007; 47: pp. 620-627 Level of evidence: 1Double-blind, placebo-controlled, randomized, crossover trial 18 healthy volunteers age 19-44 were given warfarin during a 28-day run-in period Then randomised to take either etoricoxib 120mg/day or placebo for 21 days while continuing warfarin Crossed over for another 21 days 14 subjects eventually analysed Etoricoxib increased the mean INR by 13% which the authors classed as of ‘uncertain clinical significance’ 13. Schaefer MG, Plowman BK, Morreale AP, Egan M. Interaction of rofecoxib and celecoxib with warfarin. American Journal of HealthcareSystem Pharmacy 2003; 60: pp. 1319-1323 Level of evidence: 1Prospective, open-label, randomised cross over study 16 patients on stable warfarin therapy and all on a COX-2 comparator agent eg traditional NSAID prior to enrolment Randomly received celecoxib 200mg/day or rofecoxib 25mg/day for 3 weeks After one week washout period they were switched to treatment with the opposite COX-2 inhibitor (they could take their pre-study analgesic during this period). 8 in both groups had a >15% increase in their INR. Only 4 had a rise with both COX-2 inhibitors therefore it appears unpredictable whether patients will have elevated INRs with different COX-2 inhibitors. 14. Brown A et al. An interaction between warfarin and COX-2 inhibitors: Two case studies. The Pharmaceutical Journal 2003; 271: p. 782 Level of evidence: 3 Case report Woman age 65 with previously stable INR averaging 2.5 found the INR increased to 5.8 after taking celecoxib 200 mg od for 3 weeks 37 NSAIDs/selective COX-2 inhibitors and bronchospasm/asthma Mechanism Some patients, with or without an atopic asthma history, experience aspirin or NSAID induced asthma. Studies suggest a prevalence in the general adult population of about 20%. 1 People with aspirin-induced asthma possibly depend more on the bronchodilating activity of Prostaglandin E2. Aspirin and other NSAIDs inhibit the production of PGE2 (see Figure 1 page 5) so more arachidonic acid is available for leukotriene production. Leukotrienes C4 and D4 are potent bronchoconstrictors and mucous secretagogues. 1 Q.1 Can asthmatics who are NSAID-naïve have an NSAID? Yes, but see recommendations. Q.2 Can asthmatics who have wheezed with aspirin have an NSAID? They should avoid NSAIDs. 1 Q.3 Are any of the traditional NSAIDS less prone to induce wheeze? No evidence found so answer unknown. Q.4 Are selective COX-2 inhibitors safer? Evidence suggests that celecoxib 2,3 is safer although a case report illustrates that the risk is not completely removed. 4 Q.5 Are topical NSAIDs safe to use in asthmatics sensitive to oral NSAIDs? Probably yes but unwanted side effects such as asthma have been reported rarely with topical NSAIDs. Studies of long term unwanted effects of topical NSAIDs are lacking. Recommendations 1. Anyone with a history of an asthmatic reaction to aspirin or another NSAID or if they have high risk features (severe asthma, nasal polyps, urticaria or chronic rhinitis) should avoid all products containing aspirin or NSAIDs. 1 2. If an NSAID is absolutely necessary, use of a selective COX-2 inhibitor should be preferentially considered which should be given under medical supervision. 4 38 3. NSAID-naïve asthmatic patients can take an NSAID but they need to be aware of potential risks and advised if a respiratory reaction occurs they must stop treatment and seek medical help. As aspirin-induced asthma can develop in asthmatics > 40 years old, it has been suggested that this group avoid NSAIDs, be warned of the risks and that if NSAIDs are absolutely necessary that the first dose be taken under medical supervision. 1 39 References Mechanism and Q.2 Can asthmatics who have wheezed with aspirin have an NSAID? 1. Twycross R and Wilcock W (eds). Palliative Care Formulary third edition. Nottingham: Palliativedrugs.com Ltd, 2007. Q.4 Are COX-2 inhibitors safer? 2. Dicpinigaitis P. Effect of the cyclooxygenase-2 inhibitor celecoxib on bronchial responsiveness and cough reflex sensitivity in asthmatics. Pulmonary Pharmacology and Therapeutics 2001; 14: pp. 93-97 Level of evidence: 1Randomised double blind cross over study 8 patients One week of therapy with celecoxib did not appear to significantly affect basal airway tone or the airway receptors controlling bronchoconstriction and cough. Results of this trial cannot be extrapolated to patients with severe asthma, or those suffering an asthmatic exacerbation. Authors stated that: ‘In such conditions of enhanced inflammatory response, the role of selective cox-2 inhibition remains to be elucidated’ 3. Gyllfors P et al. Biochemical and clinical evidence that aspirinintolerant asthmatic patients tolerate the cyclooxygenase 2-selective analgesic drug celecoxib. Journal of Allergy and Clinical Immunology 2003; 111 (5): pp. 1116-1121 Level of evidence: 1+ Double-blind, randomised cross-over trial 33 patients with proven aspirin sensitivity Increasing dose challenge with placebo or celecoxib on 2 occasions 7 days apart Then all subjected to 2 doses of celecoxib 200mg 2 hours apart Lung function, clinical symptoms and urinary excretion of LTE4 measured No changes in the above including at the highest recommended daily dose of celecoxib 40 4. Baldassarre S et al. Asthma attacks induced by low doses of celecoxib, aspirin and acetaminophen. Journal of Allergy and Clinical Immunology 2006; 117 (1): pp. 215-217 Level of evidence: 3 Case report of a single-blind, placebo controlled challenge 45-year old woman with proven aspirin-induced asthma developed severe bronchospasm after 15mg celecoxib Authors conclude that even though such reactions to COX-2 inhibitors are rare, first doses should be given under medical supervision. 41 NSAIDS/selective COX-2 inhibitors and heart failure How can NSAIDs/selective COX-2 inhibitors increase the risk developing heart failure? Experimental studies have shown that giving NSAIDs to susceptible people can increase systemic vascular resistance and reduce renal blood flow, glomerular filtration rate (GFR) and sodium excretion. The combination of these mechanisms increases the risk of developing heart failure. This is thought to occur because of the effects of NSAIDs on prostaglandins: Prostaglandins have both vasoconstriction and vasodilatation actions. Patients with impaired ventricular function produce more vasodilatory prostaglandins to reduce peripheral resistance. Prostaglandin production is inhibited by NSAIDs so this compensatory mechanism is switched off when NSAIDs are given to a patient with impaired ventricular function. This results in raised peripheral resistance and reduced renal perfusion. Q.1 What is the risk of developing heart failure? The general population seems to be at slightly higher risk of developing heart failure if taking NSAIDs. 1,2 Q.2 Who is at risk? The greatest risk appears to be for those with a history of heart failure or risk factors for cardiovascular disease. 3 Consistent with the proposed mechanism of effect, there is also a higher risk of heart failure in patients on diuretics, ACE-inhibitors and beta-blockers at start of use of an NSAID. 1,2,3 Q.3 Are traditional NSAIDs safer than selective COX-2 inhibitors? The risk of taking selective COX-2 inhibitors and NSAIDs appears to be similar. 2,4,5,6 Q.4 Does the risk of taking NSAIDs vary with different preparations? There is some evidence that the risks are slightly increased for NSAIDs with a long plasma half-life and slow-release formulations. 3 In this study drugs were placed in the following half-life categories: ≤ 4 hours (diclofenac, ibuprofen, ketoprofen, mefanamic acid), 4-12 hours (indomethacin, sulindac, ketoprofen S/R) and ≥ 12 hours (naproxen, piroxicam, tenoxicam). 42 Recommendations 1. NSAIDS and selective COX-2 inhibitors should not be used in patients with severe heart failure. 2. NSAIDS and selective COX-2 inhibitors should be used with caution in those with a history of cardiovascular disease or risk factors for cardiovascular disease as they are at higher risk of developing heart failure. 3 3. NSAIDS and selective COX-2 inhibitors should be used with caution in the elderly [>65] even in the absence of other risk factors, as there is a greater risk of developing heart failure. 4. There is little evidence to show that any one drug has lower risk factors for cardiac failure than any other, but celecoxib seems to pose a similar degree of risk as traditional NSAIDs. 2,4,5,6 5. NSAIDs with a longer half-life (such as naproxen) and controlled release preparations have been associated with an increased risk of causing heart failure. 3 These should be avoided in high-risk patients. 43 References Q.1 What is the risk of developing heart failure? 1. Huerta et al. Non-steroidal anti-inflammatory drugs and risk of first hospital admission for heart failure in the general population Heart 2006; 92: pp.1610-1615. Level of evidence 2+ Case-controlled study based on the UK General Practice Research Database Cases were 1396 people with a first hospital admission for non-fatal heart failure; controls were a random sample of 5000 people. The study did not include people prescribed COX-2 inhibitors. The incidence rate of first admission for heart failure was 2.7 per 1000 person-years. Results: o 14% of cases and 10% of controls were current users of NSAID. o Risk of hospitalisation (adjusted for confounding factors) for NSAID users versus non-NSAID users: All NSAIDs: RR 1.3 (95% CI 1.1 to 1.6). Diclofenac: RR 1.1 (95% CI 0.8 to 1.5). Ibuprofen: RR 1.4 (95% CI 1.0 to 2.0). Indometacin: RR 3.4 (95% CI 1.5 to 7.7). No clear effects of dose and duration were found. Risks were slightly increased for NSAIDs with a long plasma half-life and for NSAIDs in slow-release formulations. Higher risk of heart failure in patients on diuretics, ACE-I and betablockers at start of use of NSAID. 2. Scott PA et al. Non-steroidal anti-inflammatory drugs and cardiac failure: meta-analyses of observational studies and randomised controlled trials. European Journal of Heart Failure 2008; 10: pp.11021107 Level of evidence 1+ Meta-analysis of observational studies and RCTs Five case-control studies showed a non-significant association between NSAIDs and cardiac failure. Two cohort studies showed a significant risk of cardiac failure with NSAIDs. Six placebo controlled trials in non-rheumatoid disease showed more cardiac failure with NSAIDs. 44 Six RCTs comparing coxibs with NSAIDs in arthritis showed no difference in cardiac failure risk. There are no trials comparing coxibs and NSAIDs in non-rheumatic disease. They were unable to break down results for individual NSAIDs because of heterogeneity of studies and low numbers of cases for individual drugs. Conclusion: All NSAIDs cause heart failure in susceptible individuals. The risk of COX-2 inhibitors and NSAIDs is similar. Patients with a history of heart failure are at greatest risk. Q.2 Who is at risk? 3. Page et al. Consumption of NSAIDs and the development of congestive heart failure in elderly patients. Archives of Internal Medicine 2000; 160: pp.777-784. Level of evidence 2+ Case-control study of the relationship between recent NSAID use and hospitalisation with congestive cardiac failure (CCF). Cases were 365 patients admitted with primary diagnosis of CCF Controls were 658 patients admitted to the same hospital without CCF NSAID use gave OR of 2.1 (95% CI 1.2-3.3) for admission with CCF Risk slightly greater with long acting and slow release preparations. Q.3 Are traditional NSAIDs safer than COX-2 inhibitors? See also reference 2. 4. Mamdani et al. Cyclo-oxygenase-2 inhibitors versus non-selective nonsteroidal anti-inflammatory drugs and congestive heart failure outcomes in elderly patients: a population based cohort study. The Lancet 2004; 363: pp.1751-1756 Level of evidence 2++ Canadian population-based cohort study in people older than 66 years Information obtained from drug database to identify new users of rofecoxib (14 583), celecoxib (18 908), NSAID (11 606) and age and sex matched controls (100 000). Primary end point: admission with congestive cardiac failure. Results given as RR: celecoxib 1.0, NSAID 1.4. 5. Whelton et al. Cardiorenal effects of celecoxib as compared with the NSAID diclofenac and ibuprofen. Kidney International 2006; 70: pp.1495-1502 45 Level of evidence 1+ Osteo and rheumatoid arthritis patients. Observational study of patients on Celecoxib Long-term Arthritis Safety Study (CLASS) database (randomised, double blind parallel group study.) Celecoxib 400mg bd (n=3986) vs. diclofenac 75mg bd (n=1996) vs. ibuprofen 800mg tds (n=1985). 6.1% of ibuprofen patients developed oedema compared to 4.1% of diclofenac and celecoxib patients (p<0.05). No significant difference in congestive cardiac failure between groups. 6. Farkouh et al. Cardiovascular outcomes in high-risk patients with OA treated with ibuprofen, naproxen or lumiracoxib. Annals of Rheumatological Disease 2007; 66: pp.764-770 Level of evidence 1+ Data used from TARGET trial, o 18 325 patients with osteoarthritis (OA), 2 parallel sub studies comparing lumiracoxib with either ibuprofen or naproxen. o Patients stratified into high and low cardiac risk. o High-risk group divided into aspirin users and non-aspirin users. o Primary end point all cardiovascular mortality, heart attack and stroke at 1yr. o Secondary end point congestive cardiac failure (CCF). Overall CCF developed in 1.28% of ibuprofen patients compared to 0.14% of lumiracoxib patients (p=0.031). No differences were found in CCF rates in the naproxen sub study. Q.4 Does the risk of taking NSAIDs vary with different preparations? See reference 3. 46 NSAIDs/selective COX-2 inhibitors and thrombotic events Q.1 Do NSAIDs/COX-2 inhibitors increase the risk of thrombotic cardiac events? The exact mechanism by which NSAIDs are prothrombotic is unknown. Theoretically selective COX-2 inhibitors could be prothrombotic: They allow COX-1 mediated enzyme activity to continue, which includes stimulation of platelet aggregation and vasoconstriction. This effect is exacerbated, since inhibiting COX-2 mediated enzyme activity causes blocking of vasodilation and removal of inhibition of platelet aggregation COX-2 inhibitors may impair ischaemic preconditioning.This is the phenomenon whereby an initial period of sub-critical myocardial ischaemia appears to offer both initial and more sustained protection against subsequent ischaemia. An increased risk of cardiac events could also be indirect via NSAIDs’ effect on the cardiorenal mechanism. This can result in salt and water retention together with loss of vasodilator prostaglandins, which cause a raised blood pressure and an increased risk of congestive cardiac failure. Q.2 What are the risks? The data shows increased risk for cardiac thrombotic events for NSAIDs and selective COX-2 inhibitors excluding naproxen. 1,2,3,4,5 There does not appear to be an increased risk of cerebrovascular thrombotic events. The thrombotic risk as summarised on Clinical Knowledge Summaries is shown below: COX-2 inhibitors: o Coxibs (including celecoxib at doses in excess of 200mg/day and etoricoxib) increase the risk for atherothrombosis by about 3 events per 1000 people per year (compared with placebo). Standard NSAIDs: o Naproxen 1000 mg daily has a lower thrombotic risk than COX-2 inhibitors. Overall, epidemiological data do not suggest an increased risk of myocardial infarction. o Ibuprofen may have a small thrombotic risk at high doses (e.g. 2400 mg daily), but at lower doses (e.g.1200 mg daily or less), epidemiological data do not suggest an increased risk of myocardial infarction. 47 o o Diclofenac, meloxicam, and indomethacin were associated with a increased risk of cardiovascular thrombotic events (compared with non-use). Other NSAIDs have less evidence on thrombotic risks, but they may all be associated with a small risk of thrombotic events. COX-2 inhibitors and standard NSAIDs: o People with risk factors for cardiovascular (cv) events are at higher risk of thrombotic adverse events than those without such risks. Their relative risk of thrombotic events with antiinflammatory drugs, compared with non-users, is the same as that of people without cv risks, but because the baseline risk of events in people with cv risk factors exceeds that of people with no cv risk factors, the excess risk to such individuals posed by anti-inflammatory drugs is considerable. Adverse effects may manifest early, and the risk may persist throughout and beyond treatment. Table 1. (From CKS) Risk of serious cardiovascular events associated with nonsteroidal anti-inflammatory drugs (NSAIDs) compared with placebo. NSAID Relative risk (NSAID versus placebo) 95% confidence interval Number of studies Diclofenac† Rofecoxib† Indometacin† Meloxicam† Piroxicam† Ibuprofen† Celecoxib† Celecoxib — pooled data‡ 400 mg QD‡ 200 mg BID‡ 400 mg BID‡ Naproxen† 1.40 1.36 1.36 1.24 1.16 1.09 1.06 1.6 1.19 to 1.65* 1.18 to 1.58* 1.15 to 1.61* 1.06 to 1.45* 0.86 to 1.56 0.99 to 1.20 0.92 to 1.22 1.1 to 2.3* 1.1 1.8 3.1 0.99 0.6 to 2.0 1.1 to 3.1* 1.5 to 6.1* 0.89 to 1.09 10 12 7 4 5 17 12 6 (7950 participants) — — — 16 * Increased relative risk statistically significant. Data from: [McGettigan and Henry, 2006†; Solomon et al, 2008‡] 48 Q.3 What is the risk of cerebrovascular accidents? There is some evidence that NSAIDs or COX-2 inhibitors increase the risk of cerebrovascular accidents - Andersohn et al Stroke 2006, Lee et al AJM 2007, Roumie et al Stroke 2007 – to mention a few. It is beyond the scope of this review to answer this question with certainty. Q. 4 Who is at risk? The risk applies to the general population but those with risk factors for cardiovascular disease may be of higher risk. 7 Q.5 Are traditional NSAIDs safer than COX-2 inhibitors? 2,4,7 No Diclofenac, rofecoxib,meloxicam, and indomethacin were associated with an increased risk of cardiovascular thrombotic events (compared with non-use) The risk of cardiovascular thrombotic events with diclofenac was similar to that associated with rofecoxib The risk with indomethacin was similar to that with diclofenac and rofecoxib Naproxen was not associated with an increased risk of thrombotic events . Ibuprofen was not associated with increased risk. Celecoxib at doses of 200mg/day was not associated with increased risk. Q.6 Does the risk increase with higher doses? One study looking at celecoxib suggests that it does. 7 Recommendations 1. As NSAIDs and COX-2 inhibitors excluding naproxen are associated with an increased risk of cardiovascular thrombotic events 1,2,3,4,5 their use for palliative care patients depends on a balance of risks and benefits. 2. Naproxen appears to carry the lowest risk of increasing cardiovascular events 1,5 and may be the most suitable for patients at higher risk of cardiovascular disease. 3. A second option would be ibuprofen up to 1200mg daily. 4. Avoid diclofenac 5. Use celecoxib at doses of 200mg/day or less. 49 References Q.2 What are the risks of NSAIDs/selective COX-2 inhibitors causing thrombotic events? 1. McGettigan P, Henry D. Cardiovascular risk and inhibition of cyclooxygenase: a systematic review of the observational studies of selective and nonselective inhibitors of cyclo-oxygenase-2. Journal Of The American Medical Association 2006; 296 (13): pp. 1633-1644 Level of evidence: 2 ++ Trials between 1985 and 2006 17 case controlled studies and 6 cohort studies There was no significant increase in the RR of a cardiovascular event with celecoxib or meloxicam. There was an increased RR for diclofenac There was no significant increase in cardiovascular risks with naproxen, ibuprofen or piroxicam, 2. Kearney P M et al. Do selective cyclo-oxygenase-2 inhibitors and traditional non-steroidal anti-inflammatory drugs increase the risk of atherothrombosis: meta-analysis of randomised trials. British Medical Journal 2006; 332 (7553): pp. 1302-1308. Level of evidence: 1 Included studies that compared a selective COX-2 inhibitor with a placebo or traditional NSAID for at least 4 weeks COX-2 inhibitors were associated with a moderately increased incidence of serious vascular events (RR 1.42, 95% CI 1.13-1.78) There was no statistically significant difference in the rate of a serious vascular event between those receiving COX-2 inhibitors and any NSAID (RR 1.16, 95% CI 0.97-1.38) When compared with naproxen,COX-2 inhibitors were associated with an increased incidence of serious vascular events (RR 1.57, 95% CI 1.21-2.03) 3. Caldwell B et al. Risk of cardiovascular events and celecoxib: a systematic review and meta-analysis. Journal of the Royal Society of Medicine 2006; 99 (3): pp. 132-140. Level of evidence: 1 6 RCTs with a total of 12,780 patients 50 None of the studies were either adequately powered or specifically designed to assess the risk of cardiovascular thromboembolic events with celecoxib treatment Celecoxib was administered for at least 6 weeks Studies comparing celecoxib with any other treatment showed the risk of myocardial infarct was significantly higher in the celecoxib groups (OR 1.88, 95% CI 1.15-3.08) No difference in deaths from cardiovascular events between those taking celecoxib and those taking placebo. 4. Chen LC & Ashcroft DM. Risk of myocardial infarction associated with selective COX-2 inhibitors: meta-analysis of randomised trials. Pharmacoepidemiology Drug Safety 2007; 7: pp. 762-772. Level of evidence: 1 Included 55 RCTs COX-2 inhibitors were associated with a significantly increased risk of heart attack compared with placebo / NSAIDs (OR 1.46, 95% CI 1.02-2.09) or NSAIDs (OR 1.45, 95% CI 1.09-1.93) 5. Singh G, Wu O, Langhorne P, Madhok R. Risk of acute myocardial infarction with non-selective non-steroidal anti-inflammatory drugs: a meta-analysis. Arthritis Research Therapeutics 2006; 8 (5): R153 Level of evidence: 2 ++ Studies of non-selective NSAIDs where acute myocardial infarct (MI) was objectively confirmed Included 14 observational studies Non-selective NSAIDs were associated with a statistically significant increase in the occurrence of MI when compared with non-use (RR 1.19, 95%CI 1.08-1.31) Diclofenac was associated with a statistically significant increase in the occurrence of MI when compared with non-use (RR 1.38, 95% CI 1.221.57) Ibuprofen was associated with a statistically significant increase in the occurrence of MI when compared with non-use (RR 1.11, 95% CI 1.061.17) Naproxen was not associated with a statistically significant increase in the occurrence of MI when compared with non-use 51 Q.3 What is the risk of cerebrovascular accidents? See also reference 2. 3. Caldwell B et al. Risk of cardiovascular events and celecoxib: a systematic review and meta-analysis. Journal of the Royal Society of Medicine 2006; 99 (3): pp. 132-140. Level of evidence: 1 Four studies (n=4,422) compared celecoxib with placebo and assessed cerebrovascular events Six studies (n=12,780) compared celecoxib with any other treatment and assessed cerebrovascular events There was no difference in the occurrence of cerebrovascular events between the groups 6. Chen L C & Ashcroft D M. Do selective COX-2 inhibitors increase the risk of cerebrovascular events: a meta-analysis of randomised controlled trials. Journal Of Clinical Pharmacology Therapy 2006; 31(6): pp. 565-576 Level of evidence: 1 Included 40 RCTs comparing any individual COX-2 inhibitor used for at least 4 weeks, against placebo or other active treatment Reported the proportion of patients experiencing cerebrovascular events Concluded that there is no evidence of a significantly increased risk of cerebrovascular events associated with selective cyclooxygenase-2 inhibitors compared with placebo or active treatment such as nonsteroidal anti-inflammatory drugs. Q.4 Who Is at risk? 7. Scott D & Solomon. Cardiovascular risk of celecoxib in 6 randomised placebo controlled trials. Circulation 2008; 117: pp. 2104-2113 Level of evidence: 1 This study assessed the cardiovascular risk associated with celecoxib in 3 dose regimens and the relationship between baseline cardiovascular risk and the effect of celecoxib on cardiovascular events Graph showing risk of cardiovascular events: 52 Higher dose is associated with increased risk in groups with higher cardiovascular risk Patients at highest baseline risk have an increased relative risk for celecoxib-related adverse cardiovascular events Q.5 Are traditional NSAIDs safer than COX-2 inhibitors? Naproxen appears to be the safest NSAID (see Table 1): 53 Table 1 (from CKS). Risk of serious cardiovascular events associated with nonsteroidal anti-inflammatory drugs (NSAIDs) compared with placebo. NSAID Relative risk (NSAID versus placebo) 95% confidence interval Number of studies Diclofenac† Rofecoxib† Indometacin† Meloxicam† Piroxicam† Ibuprofen† Celecoxib† Celecoxib — pooled data‡ 400 mg QD‡ 200 mg BID‡ 400 mg BID‡ Naproxen† 1.40 1.36 1.36 1.24 1.16 1.09 1.06 1.6 1.19 to 1.65* 1.18 to 1.58* 1.15 to 1.61* 1.06 to 1.45* 0.86 to 1.56 0.99 to 1.20 0.92 to 1.22 1.1 to 2.3* 1.1 1.8 3.1 0.99 0.6 to 2.0 1.1 to 3.1* 1.5 to 6.1* 0.89 to 1.09 10 12 7 4 5 17 12 6 (7950 participants) — — — 16 * Increased relative risk statistically significant. Data from: [McGettigan and Henry, 2006†; Solomon et al, 2008‡] See references 2, 4, 5 and 7. 8. Jones S C. Relative thromboembolic risks associated with COX-2 inhibitors. Annals of Pharmacotherapy 2005; 39 (7-8): pp. 1249-1259. Level of evidence: 1 RCTs, retrospective and prospective cohort studies and case-control studies were eligible for inclusion High-dose celecoxib (400 mg twice daily) was associated with a significant increase in cardiovascular events compared with placebo (RR 3.4, 95% CI 1.4-7.8) There was no significant difference between low-dose celecoxib (200 mg twice daily) and placebo. Based on existing data, celecoxib was the safest COX-2 inhibitor when given in the lowest possible dose for the shortest time in the ideal target population. 54 Q.6 Does the risk increase with higher doses? See reference 7: Increased celecoxib dose is associated with increased risk of cardiovascular events: 55 NSAIDs/selective COX-2 inhibitors and renal impairment Q.1 How do NSAIDs/selective COX-2 inhibitors cause renal impairment? There are 3 main sites and mechanisms of injury to the renal system: The first and most common mechanism is by blocking the prostaglandins’ vasodilatory action on the afferent arterioles of the glomeruli. This causes reduced glomerular perfusion, which results in reduced glomerular filtration rate. The second mechanism is an allergic type reaction resulting in interstitial nephritis and this can occur days to weeks after starting NSAIDs/COX-2 inhibitors. The third mechanism is immune-mediated resulting in membranous glomerulonephritis which can cause nephrotic syndrome. Q.2 What is the risk of renal toxicity? Traditional NSAIDs and COX-2 inhibitors can induce renal impairment and many studies suggest that cumulative dose contributes to the risk 1,2. Q.3 Who is at risk? 3,4 The risk applies to the general population but those with risk factors for cardiovascular disease may be at higher risk, especially those taking diuretics. There is also some evidence that elderly and cachectic patients are at greater risk. Changes in renal function can be seen up to and beyond 6 months from initiating therapy. Q.4 Are traditional NSAIDs safer than COX-2 inhibitors? 1,5,6,7 The greatest risk comes from using NSAIDs such as indomethacin. The safest NSAID is ibuprofen, closely followed by diclofenac. Amongst the COX-2 inhibitors, celecoxib is associated with a lower risk of renal dysfunction and hypertension – even compared to diclofenac and ibuprofen. Recommendations There is limited evidence to support these findings in relation to those with moderate renal impairment – most studies involve those with normal renal function or very mild renal impairment. Caution must therefore be used in extrapolation. 1. Avoid NSAIDs or COX-2 inhibitors if possible in patients with renal impairment. 56 2. Celecoxib is overall the safest agent to use. 1,5,6,7 3. Ibuprofen seems to be the safest traditional NSAID. 1,5,6,7 4. Changes in renal function are higher with cumulative dose 1,2, but changes in renal function can be seen up to and beyond 6 months of initiating therapy. 3.4 5. Particular care is needed when prescribing for patients with low circulating volumes [congestive cardiac failure/diuretic therapy]. 3,4 57 References Q.2 What is the risk of renal toxicity? 1. Swan S et al. Effect of Cyclooxygenase-2 Inhibition on Renal Function in Elderly Persons Receiving a Low-Salt Diet. Annals of Internal Medicine 2000; 133: pp. 1-9. Level of evidence: 1+ RCT comparing rofecoxib with indomethacin in healthy subjects aged 60-80. Used low-salt diet to increase the dependence on prostaglandins for maintaining renal function. 2 separate studies. o Single dose study – 15/16 Patients with Creatinine Clearance (Cr Cl) >40ml/min. Randomly assigned to single dose of rofecoxib 250mg, indomethacin 75mg, or placebo. Glomerular Filtration Rate (GFR) was calculated before and after administration. GFR was significantly reduced in both treatment arms compared to placebo, but no significant differences were found between the treatment arms. o Multiple dose study – 60/71 Patients with Cr Cl 30-80ml/min. Randomly assigned to rofecoxib 12.5mg od, rofecoxib 25mg od, indomethacin 50mg tds, or placebo for 5 days. Calculated baseline GFR and day 6. Lowest GFR result at 3 consecutive intervals was recorded. No significant differences found between the treatment arms. In patients with low effective circulating volume (congestive cardiac failure, diuretic use, cirrhosis) NSAID-induced alterations can result in clinically significant renal insufficiency. Decreases in GFR are similar regardless of whether COX-2 inhibitors or non-selective inhibitors are used. 2. Evidence as quoted on Clinical Knowledge Summaries: Level of evidence: 1 Their evidence for renal and renovascular risks associated with COX-2 inhibitors and standard NSAIDs comes from three systematic reviews: a) Morrison A et al. Systematic review of trials of the effect of continued use of oral non-selective NSAIDs on blood pressure and hypertension. Current Medical Research & Opinion 2007; 23 (10): pp. 2395-2404. There was a small increase in the risk of hypertension with ibuprofen. 58 b) Zhang J, Ding E & Song Y.et al. Adverse effects of cyclooxygenase 2 inhibitors on renal and arrhythmia events: meta-analysis of randomized trials. Journal of the American Medical Association 2006; 296 (13): pp. 1619-32. A systematic review of 114 RCTs assessed the risks of renal adverse events (renal dysfunction, hypertension, and peripheral oedema) associated with COX-2 inhibitors (rofecoxib, celecoxib, valdecoxib, parecoxib, etoricoxib, and lumiracoxib) There was no evidence of a class effect for COX-2 inhibitors on renal adverse events Celecoxib: o Peripheral oedema: RR 1.09 (95% CI 0.91 - 1.31). o Hypertension: RR 0.83 (95% CI 0.71 - 0.97). o Renal dysfunction: RR 0.61 (95% CI 0.40 - 0.94). Etoricoxib: o Peripheral oedema: RR 0.95 (95% CI 0.68 - 1.32). o Hypertension: RR 1.07 (95% CI 0.72 - 1.58). A total of 35 people needed to be treated for one person to develop hypertension within about 12 weeks (NNH 35, 95% CI 27 to 47). o Renal dysfunction: RR 0.59 (95% CI 0.10 to 3.32). Other COX-2 inhibitors were not significantly associated with risk c) Aw T et al. Meta-analysis of cyclooxygenase-2 inhibitors and their effects on blood pressure. Archives of Internal Medicine 2005; 165 (5): pp. 490-496. Incidence of hypertension: the risk for COX-2 inhibitors was increased compared with placebo and with standard NSAIDs. These studies found increased risks of hypertension and elevated blood pressure (particularly systolic blood pressure): The results are not entirely consistent among the studies. The risks for hypertension vary among drugs (indicating that this risk may not be a class effect); they may be greatest for ibuprofen and naproxen and least for celecoxib and diclofenac. The risks of renal and cardiorenal adverse effects from COX-2 inhibitors and standard NSAIDs may be greater in people with existing renal or cardiorenal compromise (e.g. cardiac failure). The systematic reviews and case-controlled study did not report absolute risk increases or numbers needed to treat. 59 Q.3 Who is at risk? 3. Jerkic M et al. The mechanism of increased renal susceptibility to toxic substances in the elderly. International Urology and Nephrology 2001; 32: pp. 539-547 Review article Reduced body fat increases the concentration of water soluble agents in non-fat compartments Reduced albumin levels increase the plasma levels of bound drugs Ageing reduces the activity of renin-angiotensin aldosterone system The elderly are more susceptible to the inhibitory effects of vasodilatory prostaglandins 4. Toto R et al. Effects of acute and chronic dosing of NSAIDs in patients with renal insufficiency. Kidney International 1986; 30: pp. 760-768 Level of evidence: 2 Study of 8 normal subjects and 12 patients with chronic renal insufficiency of various etiology (Creatinine Clearance 19-83ml/min). Looked at effects of acute (0-4 days) and chronic (5 days) dosing of indomethacin 50mg tds compared to ketoprofen 50mg qds. Acute dosing of both agents resulted in significant decreases of Glomerular Filtration Rate in those with renal impairment. With chronic dosing, each dose of NSAID caused transient, reversible decreases in renal haemodynamics that may ‘dampen with time’. Caution must be exercised in extrapolation of these findings to other settings. Modified release preparations ‘might cause sufficiently prolonged effects to prevent recovery between doses and cause an overall adverse effect’. The authors noted that their findings were in ‘apparent conflict’ with those of Ciabattoni et al and suggested a difference in renal pathology as a cause for this (Effects of sulindac and ibuprofen in patients with chronic glomerular disease. Evidence for dependence of renal function on prostacyclin. New England Journal of Medicine 1984; 310: pp. 279283). This was a small study, unmatched and not blinded. There was no evidence of randomisation to treatment arms. Q.4 Are traditional NSAIDs safer than COX-2 inhibitors? See reference 1. 60 5. Strand V. Are Cox-2 inhibitors preferable to non-selective non-steroidal anti-inflammatory drugs in patients with risk of cardiovascular events taking low-dose aspirin? The Lancet 2007; 370 (9605): pp. 2138-2151 Review Large clinical review looking into cardiovascular and gastrointestinal effects of NSAIDs/COX-2 inhibitors, in particular for patients taking aspirin. Several studies suggest that celecoxib is associated with fewer adverse renal effects than other non-selective NSAIDs, and could be protective against aspirin-induced changes in renal function 6. Whelton, Lefkowith, West and Verburg. Cardiorenal effects of celecoxib as compared with nonsteroidal anti-inflammatory drugs diclofenac and ibuprofen. Kidney International 2006; 70: pp. 1495-1502. Level of evidence: 1 Paper reporting on large database accumulated on cardiorenal safety during the CLASS trial (Celecoxib Longterm Arthritis Safety Study). This compared the upper GI safety of celecoxib 400mg bd with normal full therapeutic doses of diclofenac (75mg bd) and ibuprofen (800mg tds) in rheumatology outpatients. o 8059 patients enrolled, with 7968 given medication on an intention to treat basis (3987 given celecoxib, 3981 given ibuprofen or diclofenac). o Followed up for 9 months. o Mean age of population was 60 yrs. o All had normal baseline BP and renal function. Significant reductions in renal function were seen with diclofenac compared to celecoxib. Non-significant reductions were seen with ibuprofen compared to celecoxib. A substantial proportion of patients exhibited changes 6 months or longer after initiating treatment. In patients with mild renal impairment (normal creatinine, Urea>20), the incidence of clinically important changes in renal function was 2 fold lower in celecoxib compared with diclofenac or ibuprofen. o This cohort were more likely to withdraw from the study owing to renal adverse events. o Withdrawal rate was lower in the celecoxib arm (1.5%), diclofenac (3.7%), ibuprofen (4.2%). 7. Winkelmayer, Waiker, Mogun and Solomon. Nonselective and Cyclooxygenase-2-selective NSAIDs and Acute Kidney Injury. American Journal of Medicine 2008; 121: p. 12 Level of evidence: 3 61 Subjects were selected as those enrolled to Medicare and a pharmaceutical assistance programme between 1999-2004 Patients were excluded with any history of renal problems. Co-morbidities were determined from other medications prescribed for those individuals Gathered information for those patients prescribed a new NSAID/COX2 inhibitor that they had not received in the previous 6 months. Followed up for 45 days and assessors searched for any incidence of acute kidney injury, either as an outpatient or requiring inpatient stay. 962 patients had an event Celecoxib was taken as the reference group, as it was the most frequently prescribed anti-inflammatory agent. They concluded that compared to celecoxib, ibuprofen and indomethacin had a greater risk of acute kidney injury. 62 The use of NSAIDs/selective COX-2 inhibitors for Cancer-Induced Bone Pain (CIBP) Background to CIBP Up to 85% patients with bone metastases will suffer pain, often associated with anxiety and depression, reduced performance status and a poor quality of life 1 It is considered a complex pain syndrome with a triad of characteristics1: o Background element – typically opioid responsive, dull quality o Spontaneous breakthrough element o Incident pain – harder to treat with opioids Radiotherapy is considered the gold-standard treatment 1 Bone metastases are painful because tumours invading and growing within the medullary space of the bone can activate primary afferent nerve fibres which transmit noxious stimuli to the dorsal horn of the spinal cord 2 Cancer cells can secrete prostaglandins which activate the primary afferents 2 Invading tumours can also encourage the production of an inflammatory infiltrate and alter the balance between osteoblasts and osteoclasts 2 Suggested paradigm for management: see schematic 11 63 New Bone Pain Analgesics & request imaging where appropriate Pathologic fracture or high risk criteria on x-ray (e.g. osteopaenia, osteoporotic fracture) Surgery (if appropriate) yes no Exclude non-malignant bone pain (e.g. Pagets, OA, osteoporotic collapse, etc) or confirm the primary malignancy Diffuse Pain Hormone sensitive cancer hormone therapy Chemo-sensitive cancer Chemo therapy +/bisphosphonates isotopes (strontium) radiotherapy Schematic from reference 1 64 Localisable Pain Radiotherapy Q.1 What is already known about NSAIDs/selective COX-2 inhibitors and CIBP? There is a lack of robust, clinical evidence. There are no recorded outcomes for incident pain and no studies have addressed the use of COX-2 inhibitors. A Cochrane Systematic Review 3 of cancer pain has incorporated randomised control trials looking at NSAID vs placebo, opioid vs NSAID+opioid 4,5 , NSAID vs opioid 6,7 , NSAID vs NSAID 8 and NSAID vs NSAID+opioid The heterogeneity of study designs, type of pain and baseline pain severity limited the scope for meta-analysis Data related to CIBP has been extracted from this review, where the authors provide some evidence that this type of pain was investigated. These studies give us mixed results (see table 1 page 65) There is insufficient information for a systematic review on the efficacy of NSAIDs for CIBP Q.2 Do NSAIDs/selective COX-2 inhibitors inhibit bone healing? There is a lack of high quality evidence. There is none from randomised controlled trials, nor evidence from large good quality observational studies. 9 Theoretically, because osteoblasts produce prostaglandins, NSAIDs could inhibit bone healing. Some studies looking at rates of healing from non-pathological fractures have suggested an association between NSAIDs and poor healing. However, evidence has been conflicting and it must be remembered that the study may not have controlled for confounding variables such as smoking, which is known to significantly inhibit bone healing. 9 Conclusions There is some evidence that using an NSAID for bone pain secondary to metastatic cancer can have an analgesic effect and reduce the opioid requirement. 3 There is conflicting evidence as to whether NSAIDs/COX-2 inhibitors have a clinically meaningful adverse effect on bone healing. 9 65 References Background 1. Delaney B, Fleetwood-Walker SM, Colvin LA, Fallon M. Translational Medicine: Cancer pain mechanisms and management. British Journal of Anaesthesia 2008; doi: 10.1093/bja/aen100 Review 2. Urch C. The pathophysiology of cancer-induced bone pain: current understanding. Palliative Medicine 2004; 18: pp. 267-274 Review Q.1 What is already known about NSAIDs/selective COX-2 inhibitors and CancerInduced Bone Pain? 3. McNicol ED, Strassels S, Goudas L, Lau J, Carr DB. NSAIDS or paracetamol, alone or combined with opioids, for cancer pain. Cochrane Database of Systematic Reviews 2005; Issue 2. Art. No.: CD005180. DOI: 10.1002/14651858.CD005180. Level of evidence: 1++ Qualitative systematic review due to heterogeneity of sample, patient populations and outcomes See table 1 for references 4-8 4. Weingart WA, Sorkness C, Earhart R. Analgesia with oral narcotics and added ibuprofen in cancer patients. Clinical Pharmacy 1985; 4(1): pp. 53-58. 5. Lomen PL et al. Flurbiprofen for the Treatment of Bone Pain in Patients with Metastatic Breast Cancer. American Journal of Medicine 1986; 80(3A): pp. 83-87. 6. Tonachella R, Gallo Curcio C, Grossi E. Diclofenac sodium in cancer pain: A double-blind within-patients comparison with pentazocine. Current Therapeutic Research 1985; 37(6): pp. 1130-1133. 7. Stambaugh JE Jr, Drew J. The combination of ibuprofen and oxycodone/acetominophen in the management of chronic cancer pain. Clinical Pharmacology & Therapeutics 1988; 44(6): pp. 665-669 66 8. Levick S et al. Naproxen sodium in treatment of bone pain due to metastatic cancer. Pain 1988; 35(3): pp. 253-258 Q.2 Do NSAIDs/selective COX-2 inhibitors inhibit bone healing? 9. http://www.medicine.ox.ac.uk/bandolier/booth/painpag/wisdom/NSAIbo ne.html [Accessed February 1 2009] Table 1: Summary of evidence from Cochrane review (page 68) 67 Author and grade of evidence Type of comparison n Age Weingart WA et al 1985 4 Level of evidence: 1+ Lomen PL et al. 1986 5 Level of evidence: 1Tonachella R et al. 1985 6 Level of evidence: 1Stambaugh JE Jr, Drew J. 1988 7 Level of evidence: 1Levick S et al. 1988 8 Level of evidence: 1+ Opioid vs NSAID+opioid Opioid vs NSAID+opioid NSAID vs Opioid 10 17 16 NSAID/Opioid combination compared with NSAID/Opioid combination 30 Low dose NSAID vs. supramaximal dose NSAID 100 39-67 35-79 mean 60 Cancer type 2 breast, 2 colo-rectal, 3 gynae, 1 lung, 1 bladder, 1 melanoma All had metastatic disease, 6 with bony involvement stable metastatic breast cancer not stated 18-80 not stated 19-81 Mean 62 not stated Type of pain stated? not clear Bone pain bone pain in 20% of group receiving opioid then NSAID, & in 50% in group receiving NSAID then opioid Bone pain due to metastatic cancer Bone pain due to metastatic cancer Chronicity of pain Comparators Study duration Outcomes 4 months 20 years (mean 55.3 months) Ibuprofen 400mg qds or placebo on top of existing constant opioid 9 days, crossover at day 4 and day 7 Pain relief by VAS NSAID superior to placebo. 8/10 improved pain score by mean 39% (3-76%) Not stated; cannot extrapolate from disease duration Flurbiprofen orally, dose not stated, or placebo in addition to usual therapeutic regimen. Opioid doses allowed to vary. 3 weeks then crossover Pain score on 04 scale Overall NSAID superior to placebo. Results not statistically significant. 8 days not stated Diclofenac im 75mg bd or Pentazocine im 30mg bd. Cross over after 3 day period + 1 day placebo washout Daily pain score on 0-12 scale “chronic” not stated Ibuprofen 60mg qds (15) or placebo (15) in addition to stable as-needed doses of oxycodone (5mg)/paracetamol (325mg) Naproxen 1650 mg/ day vs. Naproxen 825 mg/ day 7 days 3 days Pain relief by global rating of patient and investigator (scales poorly described) 2hrly patient and investigator Pain intensity scores (VAS) Results/Conclusions Each drug significantly reduced pain intensity (p<0.01), Diclofenac provided a greater reduction when given compared to pentazocine (p<0.047) Ibuprofen reduced the need for oxycodone/paracetamol. 5 days required for maximal dose reduction effect. Baseline pain: 2 moderate, and 13 severe in the ibuprofen group. 6 moderate, and 9 severe in placebo group Pain intensity decreased by one-third in both high dose (n=51) and low dose (n=49) groups. Responders gave better pain scores if on higher dose (but not statistically significant) Subcutaneous ketorolac Q.1 What is it? Ketorolac is a cyclic proprionate compound structurally related to indomethacin. The analgesic effect is much greater than its anti-inflammatory effect. It comes in tablets/liquid form and is licensed for use IV/IM for the short-term management of moderate to severe acute post-operative pain. Evidence surrounding its safety and efficacy is largely based on short-term studies looking at acute pain. It is renally excreted with a dose-dependent effect on the risk of GI bleeding (see page 12). Manufacturer’s recommendations: Start with an initial dose of 10 mg and use a total daily dose of 90 mg for ‘non-elderly’ and 60 mg for elderly, renally impaired and patients weighing less than 50 kg with a maximum duration of treatment of 2 days. Reduce dose for patients weighing less than 50kg Contra-indications include people already on aspirin, severe heart failure and serum creatinine greater than 160 mmol Q.2 What are the side effects/risks in the general population? A study looking at post-operative use showed a dose-response relationship between daily dose and GI bleeding with a higher risk of GI bleeding if therapy lasted more than 5 days. 1 Another study of patients who had received parenteral ketorolac showed a possibly higher risk of acute renal failure after more than 5 days of therapy. 2 Ketorolac and the palliative care patient Subcutaneous ketorolac can be used for its analgesic effect when oral NSAIDs are unable to be administered. As repeated injections can be painful, it is recommended that it is used in a syringe driver. 3 Q.3 What are the reasons for using it? The use of ketorolac in palliative care is for the management of bone pain, visceral pain, neuropathic pain or pain of mixed aetiology. Here are examples of clinical situations in the literature where it has been used: 1. When opioid related side effects may limit titration of the opioid and hence adequate analgesia 2. Where there is poor analgesia despite opioid and oral NSAID 3. Where there is good analgesia but severe opioid related sideeffects It can have a significant opioid-sparing effect. Q.4 What side-effects have been noted in palliative care patients? Evidence takes the form of case series/reports. 4,5,6,7,8,9 GI bleeding has occurred, especially in patients with GI malignancies or taking steroids (see table 1 page 73). Q.5 What about the toxicities of other subcutaneous (s/c) NSAIDs ? There is no comparative evidence in the literature with regards to s/c ketorolac vs diclofenac vs naproxen. For subcutaneous naproxen, a case study did not report any specific reactions. 10 For subcutaneous diclofenac, a retrospective case series noted 1 site reaction.11 Conclusions 1. S/c ketorolac may improve pain even when oral NSAIDs haven’t. 2. There are more examples of the use of s/c ketorolac in the palliative care literature compared to s/c naproxen or diclofenac with regards to efficacy and side-effects, although this evidence is low-grade. Recommendations 1. Despite ketorolac being used for up to 6 months without any adverse effects 7, elderly people, patients with GI cancer and patients receiving other drugs which increase the risk of bleeding/renal failure are particularly at risk. 1,2,6,7 If appropriate, renal function should be monitored and ketorolac used at the lowest effective dose and for the shortest duration possible. 2. Gastroprotection (a PPI) should be co-administered if appropriate. 70 References 1. Strom, B et al. Parenteral ketorolac and risk of gastrointestinal and operative site bleeding. A postmarketing surveillance study. Journal of the American Medical Association 1996; 275 (5): pp. 376-382 Level of evidence: 2+ surveillance study showed a dose-response relationship between daily dose and GI bleeding with a higher risk of GI bleeding if therapy lasted more than 5 days 2. Feldman, H et al. Parenteral Ketorolac: The Risk for Acute Renal Failure. Annals of Internal Medicine 1997; 126 (3): pp. 193-199 Level of evidence: 2+ Cohort study of 9850 patients who had received parenteral ketorolac Showed a possibly higher risk of acute renal failure after more than 5 days of therapy and an increased risk if there was concomitant cancer, renal impairment, hypertension, cirrhosis or use of aminoglycoside antibiotics. 3. Twycross R and Wilcock W (eds). Palliative Care Formulary third edition. Nottingham: Palliativedrugs.com Ltd, 2007. For further details of references 4-9 see table1 below. 4. Blackwell N et al. Subcutaneous ketorolac – a new development in pain control. Palliative Medicine 1993; 7: pp. 63-65 5. Duncan A, Hardy J & Davis C. Subcutaneous ketorolac. Palliative Medicine 1995; 9: pp. 77-78 6. Myers K & Trotman I. Use of ketorolac by continuous subcutaneous infusion for the control of cancer-related pain. Postgrad Medical Journal 1994; 70: pp. 359-362 7. Hughes A, Wilcock A & Corcoran R. Ketorolac: Continuous Subcutaneous Infusion for Cancer Pain. Journal of Pain and Symptom Management 1997; 13 (6): pp. 315-316 71 8. De Conno F et al. Tolerability of Ketorolac Administered via Continuous Subcutaneous Infusion for Cancer Pain: A Preliminary Report. Journal of Pain and Symptom Management 1994; 9 (2): pp. 119-121 9. Ripamonti C et al. Continuous Subcutaneous Infusion of Ketorolac in Cancer Neuropathic Pain unresponsive to Opioid and Adjuvant Drugs: A Case Report Tumori 1996; 82: pp. 413-415 10. Toscani F et al. Sodium Naproxen: continuous subcutaneous infusion in neoplastic pain control. Palliative Medicine 1989; 3: pp. 207-211 Level of evidence: 3 Case series of 14 patients age 46-68 with cancer pain and switched from oral naproxen to CSCI at same doses Pain types included bone, visceral, neuropathic and nociceptive All patients given ranitidine Average duration of treatment was 21 days (7-112) No ‘generalised reactions’ noted 11. Hall E. Subcutaneous diclofenac: an attractive alternative? Palliative Medicine 1993; 7: pp. 339-340 Level of evidence: 3 Retrospective study of 27 patients 15 patients had 150mg, 4 patients 225 mg and 8 patients 300 mg Duration of administration ranged from 7 hours – 14 days, median 48 hours 1 patient developed a severe site reaction Table 1: Summary of Palliative Care literature discussing subcutaneous ketorolac (page 73) 72 Author and evidence grading No. of patients Age Dose range (mg) Duration of treatment (days) Gastroprotection Toxicity/nature Blackwell4 1993 Grade 3 7 30-90 8-31 Misoprostol None 50-150 3-22 No comment No comment 36 Majority 60 3-115 Misoprostol 4 patients developed GI bleeding: Age 19-79 Range 60-120 Median 15 Age 52-81 Duncan5 1995 Grade 3 Myers & Trotman6 1994 Grade 3 10 Age 29-36 1 patient bled when high dose dexamethasone was added 2 patients had upper GI cancer 1 patient had ? radiation proctitis 1 patient had a colonic perforation Hughes7 1997 Grade 3 25 with 30 episodes of use 60-90 3-185 Majority misoprostol, others omeprazole Malaena in patient age 81 after 22 days of 75mg PR bleeding in patient age 67 after 27 days of 90 mg Mean 20 Age 43-83 Bleeding resolved on stopping drug De Conno8 1994 Grade 3 10 90-120 Fixed at 7 days No comment No comment except with regards to site 120 75 Misoprostol None 40-73 Mean 56 Ripamonti9 1996 Grade 3 1 Age 48 APPENDIX 1 Cochrane Library search strategy (December 2008) ID Search #1 Meloxicam #2 Nabumetone #3 Indometacin #4 Indomethacin #5 Dexibuprofen #6 Fenbufen #7 Dexketoprofen #8 Tiaprofenic acid #9 Azapropazone #10 Aceclofenac acid #11 Tenoxicam #12 MeSH descriptor Anti-Inflammatory Agents, Non-Steroidal explode all trees #13 Ketorolac #14 Ketorolac trometamol #15 Aspirin #16 Mefenamic acid #17 Flurbiprofen #18 Ibuprofen #19 Naproxen #20 Salicylate* #21 Diclofenac #22 Etodolac #23 MeSH descriptor Cyclooxygenase 2 Inhibitors, this term only #24 Celecoxib #25 Etoricoxib #26 Rofecoxib #27 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26) #28 (#23 OR #24 OR #25 OR #26) #29 (#27 OR #28) A list of the same NSAIDs and COX-2 selective drugs was used in similar searches of the literature in Medline and Embase. APPENDIX 2 Levels of Evidence______________________ ________________ 1++ High-quality meta-analyses, systematic reviews of randomised controlled trials (RCTs), or RCTs with very low risk of bias 1+ Well-conducted meta-analyses, systematic reviews of RCTs, or RCTs with a low risk of bias 1Meta-analyses, systematic reviews of RCTs, or RCTs with a high risk of bias 2++ High-quality systematic reviews of case-control or cohort studies or high-quality case-control or cohort studies with a very low risk of confounding, bias, or chance and a high probability that the relationship is causal 2+ Well-conducted case-control or cohort studies with a low risk of confounding, bias, or chance and a moderate probability that the relationship is causal 2Case-control or cohort studies with a high risk of confounding, bias, or chance and a significant risk that the relationship is not causal 3 Non-analytic studies, e.g., case reports, case series 4 Expert opinion Keeley PW. Clinical Guidelines. Palliative Medicine 2003; 17: pp. 368-374 75 APPENDIX 3 Glossary of terms Absolute risk reduction (ARR)1 The proportion by which an intervention reduces the risk of an event. Bleeding time A test of the time taken for blood to clot – assessed by making a cut on the arm/earlobe and is usually 3-8 minutes. Case-control study1 A retrospective study which looks at the relationship between a risk factor and one or more outcomes. Patients are selected who already have the condition or outcome (cases) and are matched to patients who do not (controls). The effect of the risk factor is then compared between the 2 groups. Cohort study1 A prospective, observational study that follows a cohort over a period of time and investigates the effect of a treatment or risk factor. Confidence Interval (CI)1 Statisticians can calculate a range (interval) in which we can be fairly sure (confident) that the true population value lies. A 95% CI is commonly given which implies that we can be 95% confident that the true population value lies within that range. Note that the size of the CI is related to the sample size in the study – larger studies usually have a narrower CI because the bigger the study population, the closer we are to getting the true population’s value. Hazard Ratio (HR)1 This is the ratio of the hazard (i.e chance of a harmful event happening) in one group of observations divided by the hazard of the event in another group. A HR of 2 implies twice the risk. The HR should be stated with its CI. International Normalised Ratio (INR) A standardised measure of Prothrombin Time (PT) based on the World Health Organisation’s reference thromboplastin, where INR = 1 is normal Meta-analysis 2 This is a way of collating results from a number of similar studies to give one overall estimate of effect e.g relative risk. It can be considered a particular type of systematic review that concentrates on the numerical results. 76 Number Needed to Harm (NNH)1 We can calculate the amount by which a treatment increases the risk of an adverse event. The reciprocal of the difference in risk i.e 1 divided by the additional amount of risk gives us the NNH. This is the number of patients that need to be treated for 1 to be harmed by the treatment. The larger the NNH the better. Odds Ratio (OR)1 The odds of an event are obtained by dividing the number of people with an event by the number who did not have the event. The odds ratio therefore is worked out by dividing the odds of an outcome in one group by the odds of the same outcome in a different group. Prothrombin Time (PT) 3 The time taken for blood clotting to occur in a sample of blood to which calcium and thromboplastin have been added. A prolonged PT indicates a deficiency of coagulation factors. See also INR. Relative Risk (RR) In randomised controlled trials, this is the chance of an outcome while on a specific treatment compared with the chance while on an alternative/no treatment. It is worked out by dividing the rate of the event in one group of study patients by the rate in another comparative group and is usually given as a fraction or proportion. Risk This describes the likelihood of an event happening compared with the total number of possible events e.g if 5 people out of 100 die the risk of death is 5%. Systematic Reviews 2 These form an integral part of evidence-based medicine. They are a formalised and stringent process of combining information from relevant studies. The Cochrane Library contains a database of such reviews. References 1. Harris M & Taylor G (eds). Medical Statistics Made Easy first edition. London: Martin Dunitz, 2004 2. Petrie A & Sabin C (eds). Medical Statistics at a Glance second edition. Oxford: Blackwell Publishing Ltd, 2005 3. Martin E (ed). Concise Colour Medical Dictionary. Oxford: Oxford University Press, 1996 77 APPENDIX 4 Acknowledgements The clinical guidelines group would like to thank Dr Patricia McGettigan, Senior Lecturer in Medical Education and Medicine at Hull York Medical School for her advice during the development of this document. The group is also grateful to those who provided advice and comments during the local peer-review process. List of authors Consultants in Palliative Medicine Dr Katherine Lambert Dr Lynne Russon Advanced Pharmacist in Palliative Care and Pain Sue Ayers Specialist Registrars in Palliative Medicine Dr Milind Arolker Dr Julia Barnes Dr Lucy Close Dr Amy Gadoud Dr Adam Hurlow Dr Lucy Nicholson Dr Clare Rayment Dr Carina Saxby Dr Jenny Smith Dr Rachel Sorley 78 79