NSAIDs
advertisement
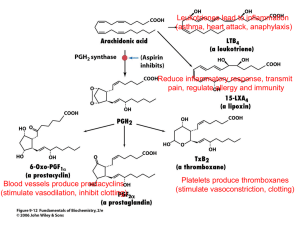
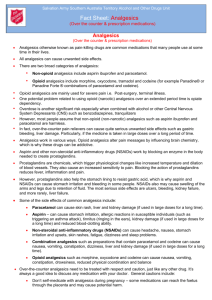
Pharmacotherapy of pain Types of pain 1 Acute pain preventive function localised has vegetative sympthomatology and doesn´t cause severe psychological changes clearly defined beginning and ending analgesics are usually effective in treatment Chronic pain without preventive function lasts 3-6 months often associated with severe psychological changes without clearly defined beginning malignant (caused by cancer)or non-malignant Types of pain 2 Nociceptive somatic • superficial • deep visceral (diffuse) Neuropatic central • deafferentational peripherial • neuropaties Idiopatic Psychogenic Therapy of pain Analgesics and co-analgesics Non-opioid analgesics • Analgesics/antipyretics • Non-steroidal anti-inflammatory drugs (NSAIDs) Opioid analgesics • Natural (morphine, dihydrocodeine) • Synthetic (fentanyl, buprenorphine) Co-analgesics (Antidepressants, Anxiolytics, Myorelaxants, Anticonvulsives, Neuroleptics, Glucocorticoids, Anesthetics, 2 sympaticomimetics, H1 antihistamines) Non-opioid analgesics Analgesics/antipyretics aspirin (acetylsalicylic acid- ASA) paracetamol (USA- acetaminophen) metamizole (textbooks from the US say it´s an NSAID) Non-steroidal anti-inflammatory drugs (NSAIDs) Non-selective inhibitors of COX-1 and COX-2 (ibuprofen, diclofenac, ASA) Preferential inhibitors of COX-2 (nimesulide, meloxicam) Selective inhibitors of COX-2 (celecoxib, rofecoxib (dereg.)) Analgesics/antipyretics Paracetamol Derivate of anilin Mechanism of action – unknown, possibly inhibition of COX-3 (variant of COX-1) in CNS Good absorption from GIT Biological half life - 1,5-3 h Only a small percentage of the drug binds on plasma proteins (10%) Elimination – through the kidnies in the form of glukuronides and sulfates In doses over 5 g/day can cause hepatal damage In the world, approximately 200 different preparates containing paracetamol are being used. Metamizole Derivate of pyrazolone Synonyms Noramidopyrín, Dipyrón has spasmolytic properties. Serious adverse effect is depression of bone marrow leading to agranulocytosis. Good absorption in the case of both peroral and rectal administration. More than 50 % binds onto plasmatic proteins Plasmatic halflife is short (i.v. metamizole - 14 min) Elimination- mostly through kidnies. Non-steroidal anti-inflammatory drugs (NSAIDs) Properties Cyklooxygenase 1 Cyklooxygenase 2 Localisation cytoplasmatic in ER perinuclear Regulation constitutional inducable / constitutional Presence in tissues GIT mucosa, renal parenchyma, endothelium, Tr Mf, Mo, CNS, kidneys, uterus, seminiferous Predicted function Integrity of stomach mucosa, kidney perfusion, Tr function Patogenesis of inflammation and genesis of pain Non-steroidal anti-inflammatory drugs Division according to COX selectivity: Selective inhibitors of COX-1: Acetylsalicylic acid (ASA)- in a dose of 30- 300 mg/day Non-selective inhibitors of COX: Acetylsalicylic acid- in a dose of 500 mg/day or more, ibuprofen, diclofenac, ketoprofen, tiaprofen, indomethacin and many more Preferential inhibitors of COX-2: nimesulide, meloxicam etc. Selective inhibitors of COX-2: celecoxib, rofecoxib, etoricoxib, valdecoxib etc. Effects of NSAIDs 1. Analgesic effect 2. Antipyretic effect 3. Antiflogistic effect (mainly higher doses) 4. Antiaggregatory effect (not every NSAID, most important is ASA because of irreversible blocade of COX-1- be careful with combination of ASA for anti-aggregation and other NSAIDs- mostly ibuprofen) 5. Other effects- for example reduced incidence of some tumors (for example colorectal carcinoma), NSAIDs – one of the most widely used drug groups→ their ADRs represent a serious medical / public health / economical problem there are big differences between various NSAIDs in the level risk of particular possible ADRs Adverse effects of NSAIDs GIT- erosions and ulcers of the gastric mucosa (also in other localisations in the GIT), nausea, vomitus, meteorism, diarrhoea, constipation... (mainly inhibition of COX-1) kidney- reduction of glomerular filtration, retention of Na and fluids, edema, hyperkaliemia, kidney failure, interstitial nephrits... (inhibition of COX-1 and 2) CVS- thrombotic events, increase of blood pressure, heart failure... (mainly COX-2 (mostly in thrombotic events)) CNS- cephalea, weakness, sleap disorders, dizziness, epileptic seizures... other- hepatotoxicity, bleeding, provocation of asthmatic attack, Ray´s syndrom, prolonged childbirth, urticaria, decreased number of white blood cells... Gastrointestinal ADRs most serious – ↓ production of prostaglandins in the gastric mucosa → peptic ulcer (most often in the stomach and duodenum; the mucosa can get damaged by NSAIDs also in other places in the GIT) roughly 25 % of chronic NSAID users might develop erosions and ulcers, in 2-4 % perforation or bleeding can occure Kidney ADRs Decreased production of prostanoids → negative effect on the perfusion of the kidneys, glomerular filtration, excretion of sodium and water and on production of renin → circulation overload, oedemas, hypertension ; hyperkalemia ; in severe cases symptoms of acute kidney failure serious complication– interstitial nephritis (immunological reasons) Incidence of kidney ADRs is poughly 18%, Cardiovascular ADRs Increased blood pressure- mostly in hypertensive patients treated with antihypertensives (mainly ACEIs, ARBs, beta blockers), there are big differences between various NSAIDs Development/worsening of heart failure- the risk is highest during the first weeks of treatment, mainly in patients with preexisting congestive heart failure; possibly 19% of all cases of congestive heart failure could be caused (at least partially) by NSAID therapy Thrombotic events- acute myocardial infarction, stroke, thromboembolic disease Opioid analgesics Dampen strong somatic and visceral pain – strongest analgesics, without roof effect, can cause addiction Dampen algognostic (perception and localisation) and algotymick(psychical and emotional) part of pain Strong agonists: morphine, fentanyl Weak agonists: tramadol, codeine Partial agonists: buprenorphine Agonists/antagonists: butorfanol, pentazocine Antagonists: naloxone, naltrexone Pharmacological effects Depressory Analgesia Depression of breathing Antitussive effect Decreased secretion and motility in the GIT – constipation Sedation Stimulatory Vomiting Miosis Increased tonus of smooth muscles, sphincters Induction of histamine release Euphoria Adverse effects of opioids Neuropsychiatric Sedation, clouded consciousness, euphoria, sleep disorders Cardiopulmonal Depression of breathing, Bronchoconstriction (high doses) Orthostatic hypotension, Bradycardia (high doses) Gastrointestinal Nausea, vomiting, constipation, gastrointestinal or gallbladder colics Urinary system Retention of urine Endocrine Decreased levels of testosterone, problems with menstrual cycle Allergic and immunologic Pruritus, immunosupression Morphine Prototypical opioid Isolated from sap from unriped skulls of poppy (1803) Fast resorption after p.o. application, bioavailability is only 30% (significant first pass effect) Most common adverse effects- nausea, vomiting, constipation, gallbladder and uretral spasms Depression of breathing is the most common cause of death in case of intoxication. Most common signs of intoxication – unconstiousness, bradypnoea a miosis Fentanyl Synthetic derivate of phenylpiperidine Strong agonist of receptors 80-100 times more potent than morphine Lipophilic character – rapid onset of action, but the effect lasts only for a short time Contraindicated in pregnancy Derivates of fentanyl- sufentanyl and alfentanyl are used in anesteziológii Big advantage – availability of fentanyl in the form of transdermal patches – „Durogesic“ The second most widely used opioid Tramadol Atypical opioid Intermediate analgesic effect High bioavailability is an advantage. In therapeutic doses lacks most of the adverse effects of opioids. The most common adverse effects are sweating, nausea and dry mouth. Suitable for treatment of mild to severe pain in adults and children. Available in different drug forms. It is cheap. In case of long term treatment, analgesics should be administered regularly, not only when the patient feels pain.