PENATALAKSANAAN NYERI
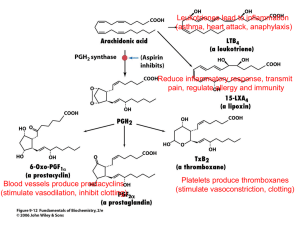
advertisement

Kuningan, 9 April 2010 Definisi Nyeri (Pain) dari IASP (International Association for the Study of Pain) Pain (Nyeri) adalah suatu pengalaman sensorik dan emosional yang berkaitan dengan kerusakan jaringan atau diduga ada kerusakan jaringan Nyeri adalah pengalaman sensorik yang berkaitan dengan aktivasi nociceptor dan lintasan nyeri Nyeri adalah suatu pengalaman emosional Kerusakan jaringan tidak mesti ada JENIS NYERI Neuropathic Pain Pain initiated or caused by a primary lesion or dysfunction in the nervous system (either peripheral or central nervous system)1 Examples Peripheral • Post herpetic neuralgia • Trigeminal neuralgia • Diabetic peripheral neuropathy • Postsurgical neuropathy • Posttraumatic neuropathy Central • Posts troke pain Common descriptors2 • Burning • Tingling • Hypersensitivity to touch or cold Mixed Pain Pain with neuropathic and nociceptive components Inflammatory Pain Pain caused by injury to body tissues (musculoskeletal, cutaneous or visceral)2 Examples Examples • Low back pain with radiculopathy • Cervical radiculopathy • Cancer pain • Carpal tunnel syndrome 1. International Association for the Study of Pain. IASP Pain Terminology. 2. Raja et al. in Wall PD, Melzack R (Eds). Textbook of pain. 4th Ed. 1999.;11-57 • • • • Pain due to inflammation Limb pain after a fracture Joint pain in osteoarthritis Postoperative visceral pain Common descriptors2 • Aching • Sharp • Throbbing Diagnosis Drug Treatment Acute and chronic pain NSAIDS (al Meloxicam/ Movi-cox), Opioids, Paracetamol Myofascial pain dysfunction Neuropathic pain, neuralgias Analgesics (Movi-cox), tricyclics, centrally-acting muscle relaxants, glucocorticoids Carbamazepine, phenytoin, baclofen, tricyclics, gabapentin, others? Ascending Pain Transmission Pathway The ascending neural pain pathway is only a 3 neuron relay The major convergence point is the ventral posterior lateral nucleus of the thalamus, which relays the signal to limbic and cortical areas Ascending Pain Pathway (Purves, 2001). Descending Pain Modulation Pathway The Descending Pain Pathway – The Periaqueductal Grey (PAG) is the major convergence point. Descending pain pathway (Purves, 2001). Targets of Pain Therapies Pharmacotherapy Non-opioid analgesics Opioid analgesics Nerve Blocks Adjuvant analgesics (neuropathic, musculoskeletal) Electrical Stimulation Acetaminofen Transcutaneous electrical nerve stimulation (TENS) Percutaneous electrical nerve stimulation (PENS) Alternative methods (NSAID) Gottschalk et al., 2001 Acupuncture Physical Therapy Chiropractics Surgery Thick, myelinated, fast conducting neurons Mediate the feeling of initial fast, sharp, highly localized pain. Rabaan Tekanan Very thin, unmyelinated, slowconducting Mediate slow, dull, more diffuse, often burning pain. Nerve Fibers Class Velocity Function A- A- Fast Fast Motor A- A- Intermediate Intermediate B C Small Small Touch, pressure Muscle tone Pain, temperature Motor Pain Chemical mediators are released from damaged tissue and inflammatory cells. Some inflammatory mediators directly activate nociceptors, while others act together to sensitize the pain pathway. Inflammation l l l biological response to injury or foreign substances acute and chronic inflammation components: cellular response biochemical mediators Mechanisms of Inflammation Cellular Mechanisms: Acute inflammation PMN Chronic inflammation lymphocytes monocytes Mechanisms of Inflammation Biochemical Mediators vasoactive amines plasma proteases (complement, kinins) arachidonic acid metabolites (PG, LT) lysosomal constituents oxygen derived free radicals cytokines growth factors Mediators of Inflammation Arachidonic Acid Metabolites Prostaglandins Leukotrienes Generation of Eicosonoids Phospholipids Phospholipase Arachidonic Acid 5-lipoxygenase cyclooxygenase 5-HPTE PGG2 peroxidase LTB4 LTC4 PGH2 TXA2 PGI2 PGE2 PGF2 PGD2 Biological Effects of Prostaglandins PGE2 Vasodilatation, pain sensitization, gastric cytoprotection PGF2 Bronchoconstriction, uterine contraction PGI2 Inhibit platelet aggregation, gastric cytoprotection TxA2 Platelet aggregation Roles of COX-1 and COX-2 Arachidonic acid COX-1 “Constitutive” COX-2 PGs PGs · GI cytoprotection · Platelet activity · Renal function Inducible · Inflammation · Pain · Fever Constitutive · Renal function Non-COX selective inhibitors of cyclooxygenase Selective COX-2 inhibitors Leukotriene inhibitors Non-COX Selective NSAIDs Carboxylic acids [salicylates, meclofenamate, diflunisal] Indoleacetic acids [indomethacin, sulindac] Propionic acids [ibuprofen, fenoprofen, ketoprofen, flurbiprofen] Naphthalene acetic acids [naproxen] Non-COX Selective NSAIDs [cont’d] l l l l l Diclofenac Etodolac Nabumetone Oxaprozin Ketorolac COX - 2 Inhibitors Celecoxib l Rofecoxib l Valdecoxib l Meloxicam (Movi-cox)* *[less COX-2 selective] l Golongan Coxib resiko kardiovaskuler + stroke Physicians prescribing celecoxib or valdecoxib should consider the emerging cautionary data "when weighing the benefits against risks for individual patients." The most appropriate candidates for coxib therapy are patients at a high risk of GI bleeding or who have a history of intolerance to "or are not doing well on" nonselective NSAIDs. "Individual patient risk for cardiovascular events and other risks commonly associated with NSAIDs should be taken into account for each prescribing situation." Consumers should use all over-the-counter analgesics, "including NSAIDs," strictly according to the label instructions and consult a physician if using them for longer than 10 days. Justification for the Development of COX-2 Selective Inhibitors COX-2: A New Anti-inflammatory Drug Target Arachidonic acid Glucocorticoids COX-2 (Inducible) COX-1 (Constitutive) (–) · · · · X (–) TARGET FOR A SPECIFIC COX-2 INHIBITOR NSAIDs Stomach Intestine Kidney Platelet Inflammatory site: · Macrophages · Synoviocytes · Endothelial cells COX-2 Selectivity: Molecular Basis NSAID Binding Clefts COX-1 COX-2 Chemical Structures of Oxicams and Coxibs OXICAMS COXIBS Linear, enolic acid Y-shaped, Tricyclic CH3 Meloxicam OH O S N H S O NH2 O Celecoxib S O N N N CF3 N CH3 O H3C O CH3 Piroxicam OH S O Rofecoxib O O O CH3 O S N N O N H COX-2 Selectivity DRUG Rofecoxib Celecoxib Meloxicam Diclofenac Indomethacin COX-2 IC50/COX-1 IC50 .013 .080 .200 .170 1.500 Efficacy as an emerging concern of NSAID used Potency (strong) Onset of action (rapid) Duration of action (long) •Efek samping minimal •Harga terjangkau Meloxicam (MOVI-COX) was approved recently by the FDA for use in osteoarthritis. The recommended dose for meloxicam is 7.5 to 15 mg once daily for osteoarthritis and 15 mg once daily for rheumatoid arthritis. Meloxicam demonstrates roughly tenfold COX-2 selectivity on average in ex vivo assays. However, this is quite variable, and a clinical advantage or hazard has yet to be established. There is significantly less gastric injury compared to piroxicam (20 mg/day) in subjects treated with 7.5 mg/day of meloxicam, but the advantage is lost with 15 mg/day (Goodman & Gilman, 2006) Potency of NSAID milligram basis of active compound for each formula potency NSAID strong Meloxicam Piroxicam Diclofenac moderate Celecoxib Nimesulide Ketorpofen weak Mefenamic acid Naproxen Nabumetone mg/formula 7.5, 15 10, 20 25, 50, 75 100, 200 100 100, 200 500 500 500 Onset of action of NSAID onset NSAID T-max (hr) Rapid Diclofenac 0.8 Nimesulide 1.2 – 2.7 Slow Celecoxib 2–4 Meloxicam 6 Duration of action of NSAID duration NSAID short Diclofenac Nimesulide moderate Celecoxib Naproxen long Meloxicam Piroxicam T-1/2 (hr) 1.1 1.8 – 4.7 11 14 20 57 TOXICITY OF NSAIDs Ototoxic Bronchospam Color blindness CHF Hepatotoxic UGIB Perdarahan GI Bleeding Nephrotoxic Allergy Tocolytic Mechanism of = Mechanism of therapeutic effects adverse effects Table IV. Incidence of gastrointestinal (GI) adverse events No. of patients Drug exposure (days) Patients/ byear No. of GI adverse events Percentage per 100 patients/year 736 56 113 0 0 Meloxicam 7.5mg 10158 33 918 3 0.3 Meloxicam 15mg 2960 179 1451 9 0.6 Meloxicam 22.5mg 910 241 600 6 1 Diclofenac 5464 35 524 9 Naproxen 243 117 78 1 1.7 1.3 Treatment Placebo Efficacy and Tolerability of Meloxicam, a COX-2 Preferential Nonsteroidal Anti-Inflammatory Drug [Clin Drug Invest 22(12):799-818, 2002. © 2002 Adis International Limited] Kombinasi OAINS Kombinasi 2 OAINS: Tidak dianjurkan Efek samping meningkat Tidak menambah efikasi Kombinasi OAINS dengan Pelindung Lambung: Kombinasi OAINS dan Analgetik: Masih dapat dipertanggungjawabkan Ditujukan untuk sedikit mengatasi masalah efek samping terhadap lambung. Dapat diberikan bersama golongan PPI, Misoprostol NSAID +Acetaminophen Greater analgesic effect than either alone Avoids adverse effects of opioids Similar half lives for many NSAIDS and acetaminophen Over-the-counter Each has analgesic ceiling. Pain: A conceptual approach to treatment (Biopsycosocial approach) Anti-depressants / psychotropics Cognitive therapies Functional restoration Pain Behaviors Suffering Opioid Relaxation Spiritual Pain Perception Adjuvants NSAIDs? Acetaminophene Neural augmentation Ablative surgery Local block Nociception NSAIDs (Movicox ®) Surgery Physical modalities 1. Looser JD, Cousins MJ. Med J aust 1990;216: 153-208; 2. van den Hout JH, et al. Clin J Pain. 2003;19:87-96.; 3. Mynors-Wallis L, et al. Br J Psychiatry. 1997;170:113-119.; 4. Morley S, et al. Pain. 1999;80:1-13. Anamnesa nyeri secara sistematik dan teratur Berprasangka baik (percaya) terhadap keluhan pasien atau keluarga Carilah metode kontrol nyeri yang nyaman untuk pasien dan keluarga Dilakukan intervensi yang tepat waktunya, logis dan terkoordinasi Edukasi pasien dan keluarga untuk mengatasi nyeri sekuat mungkin