Gastric acidity after pancreatoduodenectomy: influence of surgical
advertisement

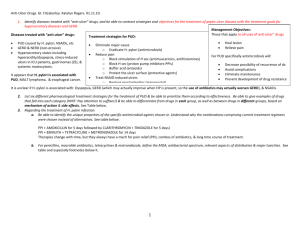
Gastric acidity after pancreatoduodenectomy: influence of surgical technique and peri-operative medical treatment. M.J.M. Morak1, T.C.K. Tran1, M.J. Bruno2, W.C.J. Hop3, G. Kazemier1, J. de Jonge1 and C.H.J. van Eijck1 1 Department of Surgery Erasmus Medical Center, Rotterdam, The Netherlands 2 Department of Gastroenterology and Hepatology Erasmus Medical Center, Rotterdam, The Netherlands 3 Department of Biostatistics Erasmus MC, Rotterdam, The Netherlands Background: Gastric acid at the anastomotic site after pancreaticoduodenectomy might cause peptic ulcers. This study was performed to compare gastric acidity after pylorus-preserving pancreatoduodenectomy (PPPD) and classical Whipple’s resection, in addition we assessed the effect of proton pump inhibitors (PPIs) and somatostatin analogues. Method: In a prospective cohort study, 50 (69%) patients underwent a PPPD and 22 a classical Whipple’s resection. Patient received intramuscular Sandostatin long acting release (LAR) (n=48; 67%) or subcutaneous octreotide (n=23; 32%). Esomeprazole was started following operation if not used pre-operatively. Gastrin levels were measured before and on day 2 after surgery together with gastric acidity. Results: Multivariate analysis showed that the type of somatostatin analogue and preoperative PPI were independent determinants of gastric acidity two days postoperatively. The type of resection or post-operatively started PPIs had no effect on gastric acidity. There was a positive relation between serum gastrin levels and gastric pH. The type of resection, type of somatostatin analogue or PPIs had no influence on serum gastrin. Conclusion: There is no difference between PPPD or classical Whipple’s resection on postoperative gastric acidity. Pre-operative use of PPIs and the administration of subcutaneous octreotide resulted in diminished gastric acidity on day 2 postoperatively, which may prevent anastomotic ulcers. Sandostatin LAR resulted in significantly higher gastric acidity.