AntiUlcerLOs
advertisement

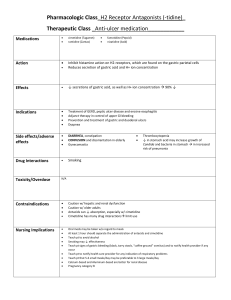
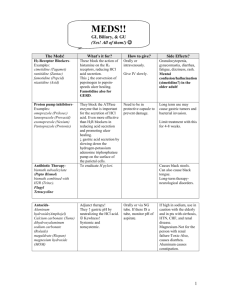
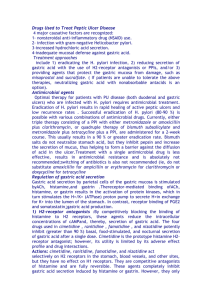
Anti-Ulcer Drugs. GI. Fitzakerley. Katelyn Rogers. 01.11.10. 1. Identify diseases treated with “anti-ulcer” drugs, and be able to contrast strategies and objectives for the treatment of peptic ulcer disease with the treatment goals for hypersecretory diseases and GERD. Management Objectives: Those that apply to all uses of anti-ulcer” drugs Diseases treated with “anti-ulcer” drugs: Treatment strategies for PUD: PUD caused by H. pylori, NSAIDs, etc GERD & NERD (non-erosive) Hypersecretory states including hyperacidity/dyspepsia, stress-induced ulcers in ICU patients, gastrinomas (ZE), & systemic mastocytosis. It appears that H. pylori is associated with PUD, MALT lymphoma, & esophageal cancer. Eliminate major cause o Eradicate H. pylori (antimicrobials) Reduce pain o Block stimulation of H sec (antimuscarinics, antihistamines) o Block H sec (proton pump inhibitors-PPIs) o Buffer acid (antacids) o Protect the ulcer surface (protective agents) Treat NSAID-induced ulcers o Replace prostaglandins (misoprostol) Heal lesion Relieve pain For PUD specifically antimicrobials will: Decrease possibility of recurrence of dx Avoid complications Eliminate maintenance Prevent development of drug resistance It is unclear if H. pylori is associated with: Dyspepsia, GERD (which may actually improve when HP is present, so the use of antibiotics may actually worsen GERD), & NSAIDs. 2. 3. List six different pharmacological treatment strategies for the treatment of PUD & be able to prioritize them according to effectiveness. Be able to give examples of drugs that fall into each category (HINT: Pay attention to suffixes!) & be able to differentiate from drugs in each group, as well as between drugs in different groups, based on mechanism of action & side effects. See Table below. Regarding the treatment of H. pylori infection: a. Be able to identify the unique properties of the specific antimicrobial agents chosen ie. Understand why the combinations comprising current treatment regimens were chosen instead of alternatives. See table below. PPI + AMOXICILLIN for 5 days followed by CLARITHROMYCIN + TINIDAZOLE for 5 days) PPI + BSIMUTH + TETRACYCLINE + METRONIDAZOLE for 14 days Therapies change with time, but they always have a mech for pain relief (PPI), combos of antibiotics, & long time course of treatment. b. For penicillins, macrolide antibiotics, tetracyclines & metronidazole, define the MOA, antibacterial spectrum, relevant aspects of distribution & major toxicities. See table and especially footnotes below it. 1 4. Compare and contrast the properties of different classes of drugs that are used to raise intragastric pH (proton pump inhibitors, H2 blockers & antacids). See Table below and footnotes. Treatment Strategies Eradicate H. pylori Block stimulation of H+ secretion Block acid secretion Buffer acid Protect the surface Replace prostaglandins Drug Groups/ Class Antimicrobials – must be broad spectrum since H. pylori is gram -. Antimuscarinics, Proton pump inhibitorsa Antacids Protective agents MISOPROSTOL Main Purpose Eliminate major cause Reduce pain Reduce pain Reduce pain Reduce pain Treat NSAID-induced ulcers Drug Names METRONIDAZOLE/TINIDAZOLE**** MISOPROSTOL (PGE1) Most effective at preventing & treating PUD! MOA CIDAL Unknown MOA. CIDAL Cell wall inhibitor (B-lactam) STATIC Prot synth inhib (50S) to prevent tanslocation STATIC Prot synth inhib (30S) prevent addition of aas Direct (but limited) antimicrobial activity Protects ulcer surface1 BISMUTH=active ingred. Difft fxns in large intestine2. ALUMINUM HYDROXIDE CALCIUM CARBONATE MAGNESIUM HYDROXIDE SODIUM BICARB OTC. Differ greatly b Good ones are not absorbed systemically, but has serious side eff Buffers acid. SUCRALAFATE BISMUTH SUBSALICYLATE Effectiveness ESOMEPRAZOLE/ OMEPRAZOLE, LANSOPRAZOLE, PANTOPRAZOLE, RABEPRAZOLE Most effective agents for reducing intragastric acidity MANY (Gi, CNS, disulfiramlike, teratogenic (?), inhib CYP2C9 Toxicity Hypersen s-itivity GI upset Drug interactions (bc both a substrate & inhib of CYP3A4) GI upset Photosensitivity Brown discoloration of growing teeth (contraindicate d in pregnancy) Blackening of stool (confuse with GI bleed) & tongue. Salycylate toxicity (vomiting, tinnitus, confusion, hyperthermia, resp alkalosis, metabolic acidosis) Side Effects AMOXICILLIN* CLARITHROMYCIN** TETRACYCLINE*** Anti-histamines BISMUTH SUBSALICYLATE ATROPINE PIRENZIPINE CIMETIDINE OTC Reduce intragastric acidityA Rarely used! Competitive inhibitors of ACh at M rec. ATROPINE is unselective. PIRENZIPINE is modtly selective for M1, but has GI effects (so acid sec can’t just be M3) OTC. Esp prevent nocturnal gastric acid secretion Primary: Highly selective, competitive inhibitors of parietal cell H2 recs. Secondary: Dec intracell cAMPdec in meal-stimulated acid secretion.C Irreversible inhibitors of ACTIVE (H/K ATPase) for 49+ h (only in parietal cell) SLOW GASTRIC EMPTYING & PROLONG EXPOSURE OF ULCER TO ACID (MORE SEVERE THAN H2 BLOCKERS) Few. Elderly have decd clearance & reduction in vol of distribution! Mental status changes (IV) Compete for renal tubular secretion w/ weak bases (MET). Inhibit gastric first-pass metab of ethanol (F), except FAMOTIDINE Unknown affects in pregnancy. RAPIDLY given bradycardia & hypoTD None significant. Rare drug interactions Post-therapy rebound acid hypersecretion upon cessatioin. 1-5% have the usual side effects. Long term use may inc risk of hip fx (dec vit B12, Fe, Ca, & Zn absorption), resp & enteric infections, & ECL cell hyperplasia bc of the decd gastric pHinc somatostatindec gastrin release, so more cells are made. 2 (Sometimes given with SIMETHICONEantifoaming agentdecs ST and pain) Al3+: Constipating Mg2-: Cathartic CaCO2 & NaHCO3 produce CO2 (add SIMETHICONE) gastric distention and bletchin. ALUMINUM & MAGNESIUM HYDROXIDE have a much lesser incidence of serious side effects. Drug interactions CAUSED by antacids: -Decd gastric pH (change absorption) -Binding of drug in intestine (dec abs) -Incd gastric emptying (dec abs) -Alkalinize urine (change elimination) INTERACTS WITH TETRACYCLINE. Treats ulcers induced by NSAIDs. -Sucrose sulfatealuminum hydroxide complex that attaches to the basement memb of the ulcer. -No acid-neutralizing properties, but may stimulate mucosal PG & HCO3, as well as bind GFs that facilitate repair. -Limted to stress-related gastritis since advent of PPIsc -Constipation from aluminum salt May bind to other meds & dec their absorption (see Q 6). Locally blocks actin of NSAIDs on the stomach lining, so they can act systemically at target. -Reduces histaminestimulate cAMP productiondecd H sec, stim of mucous & bicarb sec (raises gastric pH & protects surface) -Reduce incidence of NSAID-induced ulcers to <3% & complications by 50%d Abortifacient – stimulates uterine contractions. Dose related diarrhea, severe nausea, cramping abdominal pain (incd intestinal electrolyte and fluid sec) in 10-20% of patients. *Of the penicillins, AMOXICILLIN is the most effective because of its greater oral availability (compared to Carbenicillin, Piperacillin, & Ticarcillin) & its acid stability (compared to Ampicillin). **Of the macrolides, decreased dosing & GI side effects are found with CLARITHROMYCIN/Azithromycin compared to erythromycin. CLARITHROMYCIN is more acid stable than erythromycin too. Azithromycin has decreased drug interactions bc of no CYP450 interaction, than both CLARITHORMYCIN & erythromycin (this characteristic makes Azithromycin appear better), but the MIC50 and MIC90 for CLARITHROMYCIN are 0.03 and 0.06 respectively, while Azithromycin is 0.06 & 0.25 respectively. In other words, less CLARITHROMYCIN is needed to inhibit H. pylori; therefore CLARITHROMYCIN is the BEST of the macrolide drugs. ***Of the Tetracyclines, TETRACYCLINE HAS THE BEST ACTIVITY. Both TETRACYCLINE & Oxytetracycline are incompletely absorbed so give with food & don’t give with antacids because it chelates the antibiotic. ****TINIDAZOLE is a newer formulation that has a better dosing schedule & less resistance. In obligate anaerobes, METRONIDAZOLE acts as an electron sink; reduction liberates toxic intermediates, which damage DNA & other macromolecules. 35%-65% of H. pylori are resistant to METRONIDAZOLE. Two significant drug interactions are particularly relevant to ulcer treatment: METRONIDAZOLE potentiates the anticoagulant effect of WARFARIN; CIMETIDINE decreases the plasma clearance (potentiating the effects of METRONIDAZOLE). 1. BISMUTH disrupts cell wall, causing lysis; prevents adhesion; inhibits urease; coats ulcer, protets from acid & pepsin; stimulates prostaglandin, mucous & bicarb secretion. 2. In lower GI is antimicrobial agent (but limited) & binds enterotoxins. SALICYLATE also inhibits prostaglandin & chloride secretion. Used to treat traveller’s diarrhea. A. Incd gastric acid secretion results from release of ACh from the neurons of the enteric nervous sytem, which acts on M3 rec on parietal cells (directly incg H+ sec) and ECL cells (causing release of histamine, which acts on H2 recs to inc H+ sec). B. Glycopyrrolate may show up on boards but is never used. It is ~ ATROPINE, but less likely to cross BBB. C. CIMETIDINE net effect is inhibition of all forms of acid secretion: meal-stimulated (60-80%), basal & nocturnal (>90%). Vol of gastric sec & pepsin conc are also reduced. Other drugs in this class are FAMOTIDINE, NIZATIDINE, RANITIDINE, ROXATIDINE. It’s just that CIMETIDINE is the prototype drug in this class. T1/2=1-4 hours. Presc doses maintain > 50% acid inhibition for 10 hours, while OTC only 6 hours. Cleared by combination of hepatic metabolism, glom filt, & renal tubular secretion. NIZATIDINE undergoes little first-pass metab (100% bioavail), while others have ~50%. CIMETIDINE, FAMOTIDINE, & RANITIDINE are available IV for use in treatment of stress-related ulcers. CIMETIDINE is least potent and requires the largest dose, while FAMOTIDINE is the most potent so only a small dose is required. D. CIMETIDINE causes in <3% of patients: at high doses, inhibits binding of DHT to androgen rec, inhibits estradiol metab & incs serum prolactin levels; with long term use can cause gynectomastia & impotence in men & galactorrhea in women. More significant drug-drug interactions are that it inhibits hepatic microsomal drug-metabolizing enzymes CYP3A4, CYP1A2, CYP2C9, & CYP2D6 incs effects of other drugs. a. PPIs are useful in the treatment of Zollinger-Ellison syndrome & GERD (conds where H2 blockers are not completely satisfactory). PPIs have only modest efficacy in treating NERD; they have not been conclusively shown to be superior to either H2 antagonists or antacids in providing symptomatic relief of heartburn. PPIs are acid-labile prodrugs, so they are administered in acid-resistant formulations (either an enteric coating, or combined with sodium bicarb) that dissolve in the intestine where the drug is then absorbed & circ throughout the body. The prodrug diffuses preferentially into acidified compartments (ie parietal cell canaliculi), this is where it is converted to active form after protonation. In fact PPIS require an acid envt in the parietal cell. Short t1/2, however at least 18 hs are required for synth of new pump molecules significant acid inhibition which lasts ~24 h. ONLY ONCE DAY DOSING! Full acid inhibition is seen only after 3-4 d after daily meds. Undergo first pass metabolism (CYP2C19 & CYP3A4); with negligible renal clearance. ESOMEPRAZOLE, LANSOPRAZOLE & PANTOPRAZOLE are available IV for treatment of stress-induced ulcers. 3 b. ALUMINUM HYDROXIDE has a SLOW rate of dissolution slow onset, long duration action, while SODIUM BICARBONATE IS FAST Rapid onset, short duration of action DRUG SERIOUS (BUT RARE) SIDE EFFECTS ADVANTAGES DISADVANTAGES ALUMINUM HYDROXIDE 1. efficient 2. low systemic absorption 1. constipation 2. not very effective when given alone MAGNESIUM HYDROXIDE 1. efficient 2. low systemic absorption 1. osmotic diarrhea 1. renal insufficiency hypermagnesemia CNS and cardio- toxicity 1. belching, gastric distention 2. rebound acid secretion 1. mild systemic alkalosis 2. hypercalcemia in patients with impaired renal function if taken with dairy products (milk-alkali syndrome) CALCIUM CARBONATE 1. rapid onset of action 2. long duration 1. ↓ PO4 absorption (forms aluminum phosphate precipitates) → ↑ Ca2+ loss → osteomalacia c. SUCRALFATE requires acidic envt (just like PPI) to be activated into a viscous paste. Binds up to 6 hours selectively. d. MISOPROSTOL is rapidly absorbed & metabolized to active free acid, excreted in urine. 5. Based on an understanding of pharmacokinetics, explain why timing is critical in the administration of PPIs. First PPIS must be administered in the fasting state, when gastric motility is low. Bc bioavailability is decd approx 50% by food bc larger amplitude movts crush the protective coatings, exposing the prodrugs to the stomach acid & causing them to be inactivated. Second PPIs, only inhibit active pumps. Which in a fasting state, only 10% of pumps are active, therefore it makes sense to administer PPIs ~1 h before a meal. 1. severe metabolic alkalosis 2. hypercalcemia in patients with impaired renal function if taken with dairy products (milk-alkali 1. belching, gastric 1. extremely syndrome) SODIUM distension rapid onset of BICARBONATE 2. short duration of 3. alkalinizes urine action action 4. absorption of NaCl causes fluid retention in patients with heart 6. Explain how MISOPROSTOL facilitates ulcer healing, w/o interfering w/ NSAID failure, actions ofhypertension inflammation. or renal insufficiency First PGE1 is less involved in inflammation than other PGs & it has a shorter t1/2 (30-40 mins) than NSAIDS. In other words (from notes), the NSAID comes in and blocks PGE1 (leading to incd H+), but MISOPROSTOL can slip in and activate PGE1 again lowering the acidity! 7. Understand the reason for positive & negative interactions among anti-ulcer drugs, & be able to explain how specific OTC anti-ulcer drugs can alter the absorption &/or excretion of weak acids & bases. See side effects in Table too. Remember: SUCRALFATE and PPIS require acidic envt, so ANTACIDS & H2 REC ANTAGS dec efficacy. AND keep OTC meds in mind! Also: PPIS, H2 BLOCKERS, ANTACIDS all affect luminal pHabsorbance changesurine pH changesexcretion is effected. ANTACIDS chelate TETRACYCLINE. Gastric Absorption Excretion pH<2 (Normal) pH>4 (high) PPIs pH<8 (Normal) pH>8 (Antacids) Weak acids More DECREASE Less INCREASE Weka bases Less INCREASE More DECREASE 4