Incidence of Contrast-induced Nephropathy in Patients Undergoing
advertisement

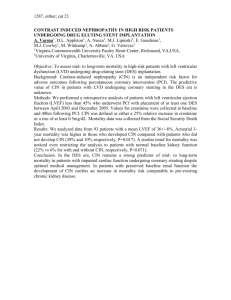
P109 (RA6443) Incidence of Contrast-induced Nephropathy in Patients Undergoing Noncoronary Angiography MR Clatworthy1, MR Todd1, E Jolly1, D Appleton2 and AN Chaudhry1 1 Division of Renal Medicine Department of Medicine, University of Cambridge, Box 118, Addenbrooke's Hospital, Hills Road, Cambridge, CB2 2QQ, United Kingdom and 2Department of Radiology, University of Cambridge, Box 188, Addenbrooke's Hospital, Hills Road, Cambridge, CB2 2QQ, United Kingdom Radiographic contrast-induced nephropathy (CIN) is a significant cause of hospitalacquired acute renal failure and has been associated with increased in-hospital mortality and length of stay. CIN is normally defined as an increase in creatinine of 25% or more from baseline1. Risk factors associated with the development of CIN include high doses of contrast media, volume depletion, pre-existing renal disease, and administration of nephrotoxins. A number of prevention strategies have been suggested such as pre-hydration, N-acetyl cysteine, and more recently sodium bicarbonate. We wished to ascertain the incidence of CIN in patients undergoing non-coronary angiography in Addenbrookes Hospital. We retrospectively reviewed the hospital biochemistry database on patients undergoing non-coronary angiography in an annual period between April 1st 2004 and March 31st 2005. Age, baseline creatinine and creatinine at 12-48 hours, and contrast dose were documented. 676 non-coronary angiographic procedures (aortofemoral, renal, and upper limb angiograms, arch aortograms, and anterograde pyelograms) were undertaken within the studied time period. Of these, 30 (4.5%) were excluded because procedures were duplicate entries on the procedure list, or patients were already receiving renal replacement therapy. Baseline and post-procedure creatinine values were available on 160 patients (23.5% of total procedures). These were divided into two groups according to previous studies1, Group 1 (baseline creatinine <97μmol/l, low risk of CIN, n=72), and Group 2 (baseline creatinine >97μmol/l, high risk of CIN, n=88). Group 1, 2 patients (28%) had a >25% fall in creatinine post-procedure, compared with 9 (10.2%) in Group 2. 11 patients (15.3%) in Group 1, and 12 (13.6%) of patients in Group 2 developed a >25% rise in creatinine following angiography. No patient with worsening renal function required renal replacement therapy. In summary, in the so-called high risk group of patients (Group 2), 13.6% developed CIN, this was similar to previously reported incidence but also to that seen in the lowrisk group (Group 1). Given current accepted criteria, the actual clinical impact of radiographic contrast on renal function seems to be relatively mild. References 1. Merten GJ,et al. Prevention of contrast-induced nephropathy with sodium bicarbonate: a randomised controlled trial. JAMA. 2004; 291:2328-2334