Renal Lab 2: Tubules, Interstitium and Vessels (March 25 or 26)
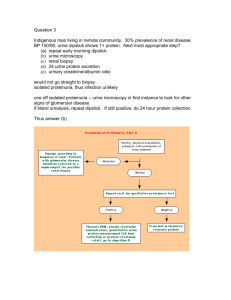
advertisement
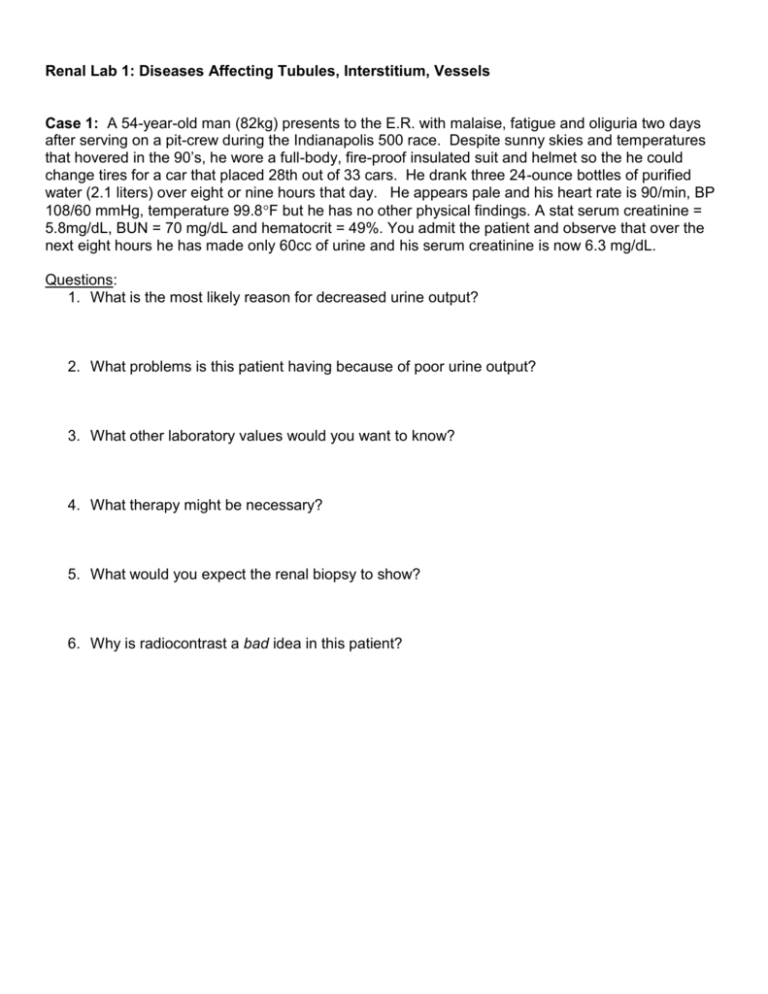
Renal Lab 1: Diseases Affecting Tubules, Interstitium, Vessels Case 1: A 54-year-old man (82kg) presents to the E.R. with malaise, fatigue and oliguria two days after serving on a pit-crew during the Indianapolis 500 race. Despite sunny skies and temperatures that hovered in the 90’s, he wore a full-body, fire-proof insulated suit and helmet so the he could change tires for a car that placed 28th out of 33 cars. He drank three 24-ounce bottles of purified water (2.1 liters) over eight or nine hours that day. He appears pale and his heart rate is 90/min, BP 108/60 mmHg, temperature 99.8F but he has no other physical findings. A stat serum creatinine = 5.8mg/dL, BUN = 70 mg/dL and hematocrit = 49%. You admit the patient and observe that over the next eight hours he has made only 60cc of urine and his serum creatinine is now 6.3 mg/dL. Questions: 1. What is the most likely reason for decreased urine output? 2. What problems is this patient having because of poor urine output? 3. What other laboratory values would you want to know? 4. What therapy might be necessary? 5. What would you expect the renal biopsy to show? 6. Why is radiocontrast a bad idea in this patient? Case 2: A 48-year-old postal worker (60 kg female) presents to you three months after receiving a living-related renal allograft for chronic kidney disease secondary to autosomal dominant polycystic kidney disease. The patient's last serum creatinine two weeks ago was 1.2 mg/dl. Laboratory results from this visit reveal a serum creatinine of 1.9 mg/dl and elevated blood levels of tacrolimus. On the exam the patient has a blood pressure of 160/95 mmHg and she is slightly tender over her graft sight. She started back to work this week. Questions: 1. What is the differential diagnosis associated with this acute clinical presentation? 2. How can you clinically distinguish between the categories of pre-renal, renal and post-renal? 3. If you suspect that tacrolimus is the cause of acute renal failure, how is the diagnosis made? How would you treat the patient? 4. When is it appropriate to biopsy the patient and what might the renal biopsy show? Case 3: An 18-year-old female presents with complaints of a diffuse rash. Ten days ago the patient was prescribed cephalexin for a lower extremity cellulitis that developed after scratching a mosquito bite. She states the cellulitis improved but yesterday when a rash appeared on her chest and legs she started taking ibuprofen. On exam the patient has a temperature of 101.5 F and a diffuse erythematous maculopapular rash. Her serum creatinine is 2.5 mg/dl and differential white blood cell count reveals 10% eosinophils (absolute count 1000). Questions: 1. What would you expect to see on urinalysis? 2. What other laboratory tests would you order? 3. How would you manage the patient? Is a renal biopsy necessary? 4. What would the renal biopsy show? Case 4: A 40-year-old man (70 kg) presents with complaints of headache that has increased in severity over the last several days and has been associated with blurred vision over the last 12 hours. On exam he has a blood pressure of 230/135 mmHg and an S4 gallop on auscultation of the heart. Urine dipstick detected blood and protein. Questions: 1. You refer the patient to the ER where your fellow intern sees this patient. What would be important signs to elicit on physical exam? 2. What laboratory tests would you order? 3. What treatment would you immediately begin? 4. The next morning, with excellent management, the BP is 156/92 mmHg and serum creatinine is 2.9 mg/dL. What would you do next? 5. When is a kidney biopsy indicated? What might the biopsy show? 6. The patient is scheduled for follow-up with his primary care physician in one week. What other studies would be appropriate as an outpatient?