outline23943
advertisement

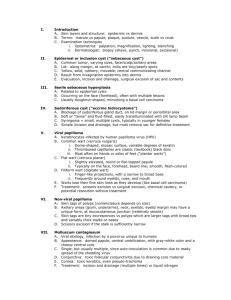
I. Introduction a. Marked increases in skin cancer, both non-melanoma skin cancer and malignant melanoma b. Many factors are contributing, including an increasingly elderly population, increased sun exposures, changes in recreational time, and clothing styles c. Optometrists, by virtue of the area that we examine, are in a primary position to detect skin cancer, the great bulk of which occurs on the head and neck II. Basal cell carcinoma (BCC) a. Epidemiology i. Non-melanoma skin cancer (NMSC) consists (classically) of basal cell carcinomas plus squamous cell carcinomas ii. Numbers continue to increase in the US – estimates for 2007 are just estimates; NMSC entities are not reported to tumor registries iii. Numbers continue to increase due to increased UV exposure, an increasingly elderly patient population, increases in outdoor activities, changes in clothing styles, changes in ozone iv. Total of NMSC is greater than all other types of cancer combined per year (this suggests, based on a projected 1.44 million new cases of all other cancer, that NMSC would reach 1.5 million new cases in 2007) v. Greater risks for BCC in patients who are white, have light colored eyes and hair, and tan poorly. vi. Highest incidence rates are in Australia (mix of susceptible phenotypes with high UV exposure) b. Risks associated with basal cell carcinoma i. Phenotypic characteristics: skin, hair, eyes ii. UV exposure patterns: much less related to cumulative/occupational exposure than to intense, intermittent exposure (in early years) iii. Use of tanning beds increases relative risk (RR) by 1.5 x iv. Smoking confers no additional risk for BCC v. Subsequent BCC after an initial BCC has a 3-yr cumulative risk of 44% vi. The relationship between UV exposure and BCC risk is complex and poorly understand, vs. that seen with squamous cell carcinoma c. Tissue characteristics i. Involvement with p53 – this is a tumor suppressor gene that may mutate, due to UV-B exposure. Locally, the tumor suppression aspect is absent or impaired, so basal cells can run amok. ii. Involvement with the signaling pathway (aka "hedgehog signaling pathway") – the 'patched gene' (or PTCH1 gene) undergoes mutations, which may result in pathway regulation and the formation of BCC (in perhaps all cases). The relationship between the HH signaling pathway and UV exposure is unknown at this time. d. Clinical characteristics i. There is no precursor to a basal cell carcinoma ii. Nodular subtype: translucent, waxy papule, pink/flesh colored, telangiectasias haphazard on surface, loss of fine skin lines with development, hard/rolled/pearly borders iii. Initially smooth surface umbilicates and ulcerates, leading to noduloulcerative subtype (poor surface protection, weak structure) iv. Superficial subtype mimics eczema, usually on trunk/back v. Sclerosing (morpheaform) subtype is flat, hard, waxy, yellow/ivory, mimicking scar tissue, with vague borders; infiltrates into collagen, periosteum, cartilage – much more dangerous than nodular subtype vi. Greatest risk of recurrence is the BCC located on eyelids (lower lid), nose, and ears (thin skin, closer to underlying structures); less risk of recurrence when located on trunk or neck III. Squamous cell carcinoma (SCC) a. Epidemiology b. c. d. IV. i. Since SCC is included in non-melanoma skin cancer, it is increasing in incidence every year. Data indicates greater increases in SCC incidence compared to BCC incidence (200% for SCC vs. 80% for BCC) ii. Traditionally, the ratio of non-ocular BCC to SCC is 4 to 1 iii. The ratio of BCC to SCC reverses in immunocompromised patients to 1 to 2 (data is mainly from studies of transplant recipients) Risks associated with squamous cell carcinoma i. Cumulative UV-B exposure is the primary risk factor but intermittent and intense exposures are involved (recent vs. childhood exposures??) ii. UV-B exposure is riskiest when long-term and chronic, not intermittent (difference between SCC and BCC) iii. UV-A radiation increases the risk but the interaction between UV-A and UV-B is not clear in promotion of SCC iv. Risk of further SCC after initial SCC is an 18% 3-year cumulative risk v. Smoking confers an increased relative risk of 2x Tissue characteristics i. Mutations in the p53 tumor suppressor gene appear to be the major factor in carcinogenesis. The mutations are widespread in sundamaged skin, occurring long before SCC ultimately appears ii. UV-B exposure causes mutations in nucleotides in which one pyridimine base is adjacent to another; the mutation is a shift from cytosine to thymine. Most are single substitutions, less are double substitutions. iii. A single substitution in a keratinocyte results in apoptosis, but double substitution mutations in cells result in clonal expansion, not apoptosis, leading to actinic keratosis. iv. Uncontrolled proliferation of abnormal cells leads to SCC in situ (Bowen's disease), then invasive SCC. Clinical characteristics i. Begins as down-growth of abnormal keratinocytes into the dermis ii. Begins as a small, firm, erythematous nodule or as a flat, red, scaly patch – neither of which are specific for SCC iii. Early SCC in the epidermis only is Bowen's disease (SCC-in-situ) iv. Lesion enlarges, with variable surface scale (heavy when arising from an actinic keratosis, less scaly when arising on sun-damaged skin) v. SCC grows faster than BCC, and ulcerates, bleeds, and scabs more quickly as well vi. Risks of metastasis vary widely: low (< 6%) if associated with actinic keratosis, ranging to 40+% if arising from scar tissue, stasis ulcers, genital areas, etc. Malignant melanoma (MM) a. Epidemiology i. Increases in incidence and increases (to a lesser degree) in mortality. Incidences increasing at faster rates than for any other neoplasm, with the exception of lung cancer in women. ii. Half the incidence of MM is between 35-65 years of age, with approximately 80% of cases occurring between 20 and 74 years. iii. Estimated 59,000 new cases of cutaneous melanoma in the US in 2006 with over 8000 fatalities iv. Age-adjusted incidence of melanoma in US is 18.3 per 100,000 persons per year v. Queensland, Australia has a cumulative incidence in the over-50 population of 1 in 19 for men and 1 in 25 for women. b. Risks associated with malignant melanoma i. Familial factors: family h/o melanoma, dysplastic nevus syndrome ii. Host factors: previous MM, number of nevi, presence of dysplastic nevi, presence of large congenital nevi, immunosuppression, and phenotypic factors (eye color, hair color, inability to tan) c. d. V. iii. Environmental factors: sunlight exposure (intense and intermittent in childhood and teen years more so than in adult years). Farmers have higher risks of SCC but not of malignant melanoma. iv. Geographical factors: living nearer the equator (particularly in early years versus later years) Tissue characteristics i. Dendritic melanocytes undergo a process of abnormal differentiation ii. Abnormal cells initially go through a radial growth phase, evolving in a step-wise fashion. These tumors are generally not associated with metastasis. Following radial growth, a vertical phase of growth begins, with increased risk of metastasis. iii. Dendritic melanocytes synthesize melanin, transferring it to keratinocytes as a protective strategy when exposed to chronic or lowgrade UV– this is protection against DNA damage. Intermittent, intense exposures cause genetic damage, resulting in cellular atypia, either in benign nevi (uncommon), dysplastic nevi (uncommon), or de novo (most common). Cells proliferate into epidermis (intraepidermal growth or radial growth), then into the dermis (vertical growth) Clinical characteristics i. Superficial spreading melanoma 1. Most common type in US (70% or more of all cases) 2. About 20-25% result from a benign nevus 3. Often on backs of legs (women) or back (men 4. Irregular borders, odd shape, odd colors ii. Nodular melanoma 1. Rare in US (5% of all cases) 2. Dangerous for vertical growth pattern and easy misdiagnosis 3. Dome-shaped, one or more colors, potentially amelanotic iii. Lentigo maligna melanoma 1. Rare in US (about 5-15% of all cases) 2. Virtually all derive from precursor (Hutchinson freckle) 3. Usually slowly progressive, malignant with nodule development iv. Acral lentiginous melanoma 1. Rare in US (5% of cases among white people) 2. Most common melanoma among blacks, Asian, Hispanics 3. Palms, soles of feet, fingers, toes Two rare types of skin cancer presenting frequently on the face a. Sebaceous carcinoma (sebaceous gland carcinoma, SGC) i. Meibomian glands (rarely in glands of Zeis or caruncle-associated sebaceous glands) ii. Uncommon compared to BCC (SGC is < 7% of lid malignancies, vs. BCC comprising 80+% of lid malignancies) iii. Older individuals, female > male, upper lid > lower lid iv. Easily misdiagnosed as chalazion, chronic blepharitis/conjunctivitis v. Typically is a firm, painless nodule; may migrate into conjunctiva via pagetoid spread b. Merkel cell cancer (MCC) i. Very rare tumor (1500 per year), involving cells that act as 'slowacting mechanoreceptors' ii. Located on head/neck 43%, eyelids 9%, elsewhere 48% iii. Most common in elderly patients, frequently appearing in areas of sun exposure. Incidence has tripled over the past 20 years. iv. Variably sized cutaneous nodule; classically violaceous, but also red or pink; painless v. Over 50% of cases have local lymph node metastasis vi. Recent (2008) discovery of Merkel cell polyoma virus; DNA located in 80% of cancers VI. Management a. Multiple modalities exist for basal cell and squamous cell: surgical excision, cryotherapy, electrodesiccation/curettage, chemotherapy, Mohs surgery b. Fewer modalities exist for melanoma, Merkel cell and sebaceous gland carcinomas: due to the potential for metastasis and lethality, surgical excision with wide margins or Mohs are recommended. VII. Prevention strategies a. Early detection i. Watch for odd behavior of the lesion (out of synch with patient's age or demographics) ii. Suspect with other malignancies (self, family, immunosuppression) iii. Older patient or anyone with heavy UV exposure iv. Changes in lesion: unresponsive to therapy, growth spurt, eroded or bleeding surface, eyelid changes (madarosis, chronic hyperemia) v. Signs of sun damage (wrinkles, telangiectasias, dermatoheliosis) b. Primary prevention vs. secondary prevention i. Primary: sunscreen use on a daily basis (mainly for SCC prevention) ii. Primary: avoid intermittent/intense exposures with clothing, avoidance, sunscreen use (mainly for BCC and MM) iii. Secondary: early detection of MM at a thin stage in which survival is considerably better iv. Secondary: regular skin examinations (self, significant other or family members, dermatologist)