Neuroscience 2a – Blood Supply to CNS
advertisement
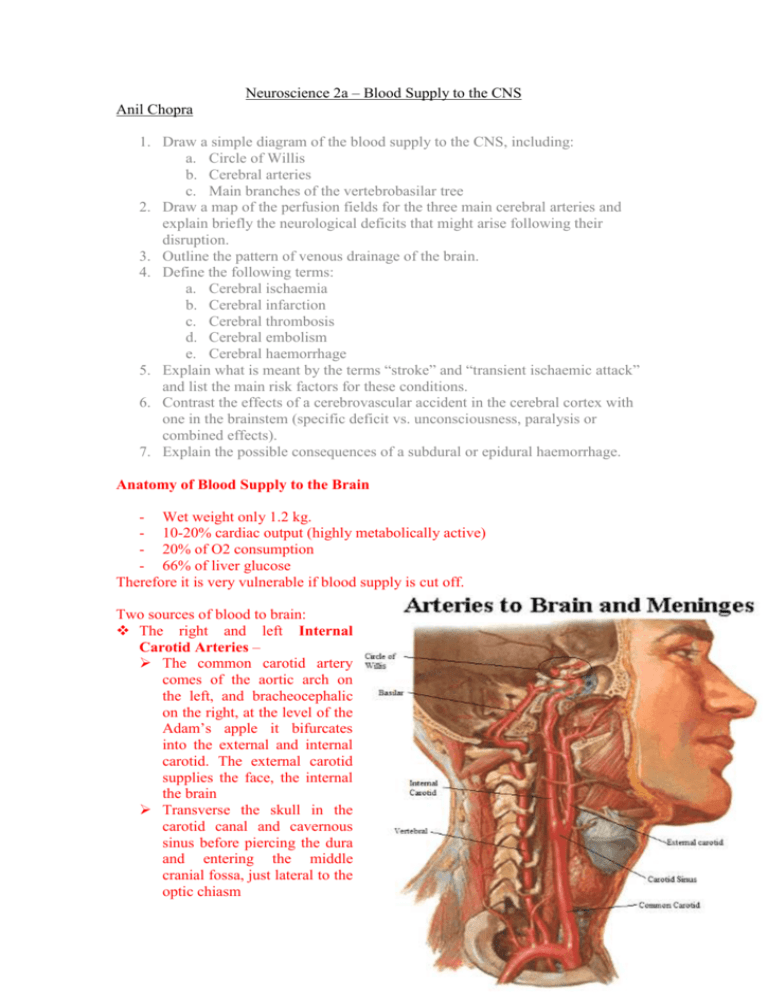
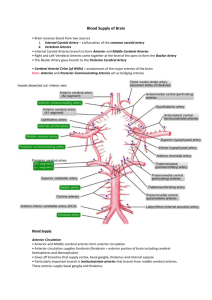
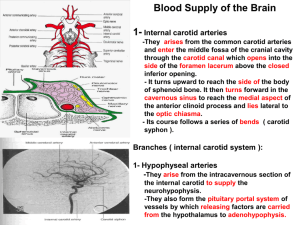
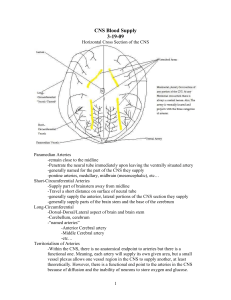
Neuroscience 2a – Blood Supply to the CNS Anil Chopra 1. Draw a simple diagram of the blood supply to the CNS, including: a. Circle of Willis b. Cerebral arteries c. Main branches of the vertebrobasilar tree 2. Draw a map of the perfusion fields for the three main cerebral arteries and explain briefly the neurological deficits that might arise following their disruption. 3. Outline the pattern of venous drainage of the brain. 4. Define the following terms: a. Cerebral ischaemia b. Cerebral infarction c. Cerebral thrombosis d. Cerebral embolism e. Cerebral haemorrhage 5. Explain what is meant by the terms “stroke” and “transient ischaemic attack” and list the main risk factors for these conditions. 6. Contrast the effects of a cerebrovascular accident in the cerebral cortex with one in the brainstem (specific deficit vs. unconsciousness, paralysis or combined effects). 7. Explain the possible consequences of a subdural or epidural haemorrhage. Anatomy of Blood Supply to the Brain - Wet weight only 1.2 kg. - 10-20% cardiac output (highly metabolically active) - 20% of O2 consumption - 66% of liver glucose Therefore it is very vulnerable if blood supply is cut off. Two sources of blood to brain: The right and left Internal Carotid Arteries – The common carotid artery comes of the aortic arch on the left, and bracheocephalic on the right, at the level of the Adam’s apple it bifurcates into the external and internal carotid. The external carotid supplies the face, the internal the brain Transverse the skull in the carotid canal and cavernous sinus before piercing the dura and entering the middle cranial fossa, just lateral to the optic chiasm Prior to bifurcation the ICA supplies branches of the pituitary (hypophyseal arteries), the eye (ophthalmic artry), parts of the basal ganglia (globus pallidus) and the limbic system (anterior choroidal artery). Divide and supply blood to the anterior and middle parts of the cerebral hemispheres (anterior and middle cerebral arteries) The right and left Vertebral Arteries – Come of the subclavian artery on both sides Ascend to the brainstem foramina in the transverse processes of the upper cervical vertebrae. Enter the skull through the foramen magnum Unite at the level of the lower part of the pons to supply blood to the brain stem via the basilar artery and the posterior parts of the cerebral hemisphere by dividing into the two posterior cerebral arteries at the superior border of the pons Before forming the basilar artery each vertebral artery has a number of branches including the posterior spinal artery and anterior spinal artery which supply the upper cervical cord and the posterior inferior cerebellar artery (PICA) which supplies the medulla and cerebellum This whole network makes up the posterior circulation Circle of Willis: In addition the posterior and anterior circulations anastomose at the base of the brain in the circle of Willis This anastomose circuit allows for compensatory flow if part is impaired via the posterior and anterior communicating arteries It is not patent in many people, and in many is not bi enough to compensate for impaired flow from a main artery such as the MCA Venous Drainage from the Brain » Venous drainage of the brainstem and cerebellum is directly into the dural venous sinuses » Drainage of the hemispheres is via internal and external cerebral veins » The external veins drain into the superior sagittal sinus → transverse sinus → lateral sinus → internal jugular vein » The internal veins drain to the deep structures of each hemisphere to the great vein of Galen → straight sinus → internal jugular » Venous sinuses are the main source of drainage which are formed from folds in the dura mater » Drainage to the jugular vein is through the jugular foramen Stroke Also known as Cerebrovascular accident (CVA) Definition of Stroke: A rapidly developing focal disturbance of brain function of presumed having a vascular origin and of more than 24 hours duration Infarction (blockage) (85%) or haemorrhage (burst blood vessel) (15%) Definition of Transient ischaemic attack: rapidly developing focal disturbance of brain function of presumed vascular origin that resolves completely within 24 hours. Infarction: Degenerative changes which occur in tissue following occlusion of an artery. Visible on a CT scan, Cerebral Ischaemia: Lack of sufficient BLOOD SUPPLY to nervous tissue resulting in permanent damage if blood flow is not restored quickly. Cerebral hypoxia refers to deprivation of oxygen supply to brain tissue and total deprivation of oxygen to the brain is called cerebral anoxia. Thrombosis: formation of a blood clot (thrombus). Embolism: when a small vessel is plugged by debris from a larger vessel. Can not only be thrombus but also air. E.g. thrombi from the heart; atherosclerotic debis from the internal carotid. Stroke Epidemiology 3rd commonest cause of death 100,000 deaths in UK per annum 50% of survivors are permanently disabled 70% show an obvious neurological deficit Risk factors o Age o Hypertension o Cardiac disease o Smoking o Diabetes mellitus o Others Anterior cerebral artery (Disinhibited frontal lobe) • Paralysis of contralateral leg > arm, face • Disturbance of intellect and judgment (abulia) • Loss of appropriate social behavior Middle cerebral artery • “Classic stroke” • Contralateral hemiplegia: this is when paralysis occurs on the opposite side of the body to which the lesion is. The arm is affected more than the legs. • Hemisensory deficits (no sensation on one side of the body) • Hemianopia (knock out half visual field) • Aphasia –inability to speak (Left sided lesion) Posterior cerebral artery • Visual deficits – homonymous hemianopia (blindness of half the visual field) – visual agnosia (Loss of the ability to interpret sensory stimuli, such as sounds or images) • Receptive aphasia – can speak by cannot understand what is being said due to defects in Wernicke’s area. Lacunar Infarcts • Lacune is a small cavity • They appear in deep structures as a result of small vessel occlusion. • Deficit is dependent on anatomical location • Normally occur as a result of hypertension. • Can be clinically silent Hemorrhagic Strokes • Extradural – build up of blood, usually from arteries, between the dura mater and the skull. Usually caused by trauma and has immediate effects due to the dramatic increase in raised intra-cranial pressure (must be treated immediately to avoid death). • Subdural – build up of blood between the dura and arachnoid membrane, normally from veins. It is also caused by trauma but has delayed effects as the drainage through veins is slow, the increase in intracranial pressure is also slow. • Subarachnoid – bleeding between arachnoid membrane and pia mater. Normally caused by spontaneous ruptured aneurysms – typical symptom is the thunderclap headache “worst headache ever”. • Intracerebral – spontaneous hyper-tensive occlusions of arteries or veins within the brain itself. Very severe as raise in intra-cranial pressure crushes brain tissue directly.