Airgas template - Morgan Community College
advertisement

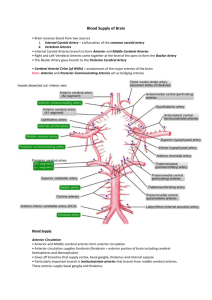
Essentials of Pathophysiology CHAPTER 37 DISORDERS OF BRAIN FUNCTION RESEARCH NEWS Migraines Increase Stroke Risk November 18, 2009 Pooling results from 21 studies, involving 622,381 men and women, researchers at Johns Hopkins Univ. have affirmed that migraine headaches are associated with more than two-fold higher chances of the most common kind of stroke: those occurring when blood supply to the brain is suddenly cut off by the buildup of plaque or a blood clot. PRE LECTURE QUIZ F T F F T Cerebral edema, or brain swelling, is characterized by a decrease in volume secondary to an abnormal fluid accumulation. The brain tissue and interstitial fluid represent the majority of the skull content. Concussions are listed under the category of focal brain injuries. All seizure events are related to epilepsy. Alzheimer disease is characterized by cortical atrophy and loss of neurons. PRE LECTURE QUIZ Glasgow __________________ is defined as an abnormal increase in cerebrospinal fluid (CSF) volume in any part or all of the ventricular system. Hydrocephalus The ______________ Coma Scale is a method for assessing level of consciousness in persons with brain injury. Meningitis A ______________ is an acute focal neurologic deficit from an interruption of blood flow in a cerebral vessel due to thrombi or emboli or to bleeding into the brain. ______________ is an inflammation of the pia mater, the arachnoid, and the CSF-filled space that can spread rapidly because of CSF circulation around the brain and spinal cord. A ___________ represents the clinical manifestations of an abnormal, uncontrolled electrical discharge from a group of neurons in the cerebral cortex. Seizure stroke GLASGOW COMA SCALE scale that is used to assess the severity of a brain injury values from 3 to 15 obtained by summing the ratings assigned to three variables depending on whether and how the patient responds to certain standard stimuli by opening the eyes, giving a verbal response, and giving a motor response, a low score (as 3 to 5) indicates a poor chance of recovery a high score (as 8 to 15) indicates a good chance of recovery QUESTION What two substances are needed by the mitochondria in order to produce ATP? a. O2 and CO2 b. Glucose and O2 c. Glucose and fatty acids d. Proteins and monosaccharides ANSWER Glucose and O2 Rationale: Glucose and oxygen are necessary for ATP production. Without ATP, no physiologic work can be done—the cells, and eventually the organism, will die. When oxygen is not available, anaerobic pathways are used, creating lactic acid that also damages the cell. b. HYPOXIA AND ISCHEMIA Hypoxia causes ATP depletion or “power failure” Aerobic metabolism stops less ATP is produced Na+/K+ º ATPase cannot run fast enough Cell swells up with water Anaerobic metabolism used lactic acid produced Acid damages cell membranes, intracellular structures, and DNA HYPOXIA AND ISCHEMIA (CONT.) Ischemia also interferes with: Delivery of energy stores (e.g., glucose) Damage to blood vessels Vasomotor paralysis Vasoconstriction Changes in blood Desaturation Clotting Sludging CALCIUM CASCADE Ischemia depolarization Depolarization glutamate release Glutamate calcium cascade Calcium influx depolarization the predominant molecular Receptor for controlling synaptic plasticity and memory function INTRACRANIAL PRESSURE (ICP) Compartment syndrome in the skull Intracranial pressure Arteries pressure greater than arterial blood collapse; blood flow to brain cut off Brain swelling Vasogenic: Cytotoxic: extracellular fluid intracellular fluid Hydrocephalus: cerebrospinal fluid Tumors BRAIN HERNIATION Increased intracranial pressure pushes the brain out of position Brain tissue is compressed into the center of the brain (2), against bone (4) or against rigid folds of the dura mater (1, 3) Compression of the oculomotor nerve is an early sign TRAUMATIC BRAIN INJURY Primary injuries—due to impact Microscopic damage: concussion, diffuse axonal injury Contusions Secondary injuries—due to: Hemorrhage Ischemia Infection Increased intracranial pressure QUESTION Tell whether the following statement is true or false. Increased ICP results in primary brain injury. ANSWER False Rationale: Increased pressure in the brain leads to secondary brain injury (there’s nowhere for the pressure to be released because the brain is encased in bone). Primary brain injury is caused by trauma. HEMATOMA—BROKEN BLOOD VESSELS Epidural space: meningeal arteries Rapid bleeding; unconsciousness may be followed by brief lucid period Dura mater Subdural space: bridging veins Slower bleeding; gradual development over days or weeks CEREBRAL BLOOD FLOW Carotid arteries branch into: External carotid – facial Internal carotid - brain Middle cerebral artery Internal carotid arteries branch into: Anterior cerebral arteries Anterior º Medial and superior cerebral surfaces of brain; artery frontal lobes Middle cerebral arteries º Lateral surfaces of brain: face and arm motor and sensory cortexes, optic radiations, speech centers Brain (lateral view) Internal carotid artery CEREBRAL BLOOD FLOW (CONT.) The basilar artery runs up to the back of the brain It splits to form the two posterior cerebral arteries º Posterior cerebral artery They supply the medulla, pons, cerebellum, midbrain, occipital lobes, temporal lobes, thalamus Basilar artery CIRCLE OF WILLIS Anterior communicating artery Connects right and left anterior cerebral arteries Blood from one carotid can cross over to supply the other side of the brain Posterior communicating arteries Connect the posterior and middle cerebral arteries Blood from the basilar artery can run forward and supply the front of the brain Brain: ventral view QUESTION Which of the following blood vessels ensures collateral circulation in the brain? a. Internal carotid arteries b. Cerebral arteries c. Basilar arteries d. Circle of Willis ANSWER Circle of Willis Rationale: The circle of Willis connects the right and left anterior cerebral arteries and the posterior and middle cerebral arteries. Blood from one carotid can cross over to supply the other side of the brain; blood from the basilar artery can run forward and supply the front of the brain. d. STROKE Stroke = “brain attack” Ischemic stroke Large vessel (thrombotic) Small vessel (lacunar infarct- occlusion of one of the penetrating arteries that provides blood to the brain's deep structures) Cardiogenic embolic Hemorrhagic stroke Transient ischemic attacks (“brain angina”) EXCITOTOXICITY Neuron firing releases glutamate Causes neighboring neurons to fire Spreading injury across the ischemic area DISCUSSION Mr. X has cor pulmonale. Mr. Y has a left ventricular aneurysm. Questions: Which of them is more likely to have a stroke? Which is more likely to have a pulmonary embolism? ANEURYSMAL SUBARACHNOID HEMORRHAGE Aneurysm Sudden-onset headache with nausea, vomiting, dizziness Hemorrhage Sudden severe headache, neck stiffness, photophobia, vision and motor problems Complications Rebleeding, vasospasm and ischemia, hydrocephalus, hypothalamus dysfunction, seizures BRAIN TUMORS Focal disturbances Dysfunction of particular brain areas Seizures, hallucinations, weakness or palsies in specific areas, sensory deficits Generalized disturbances Increased intracranial pressure: headache, vomiting, visual problems SEIZURES Spontaneous nerve firing Provoked seizures Fever Electrolyte imbalances (hypocalcemia, alkalosis) Hypoglycemia CNS infection or damage Unprovoked seizures: cause unknown EPILEPTIC SYNDROMES Partial seizures Begin in one cerebral hemisphere Secondarily generalized seizures Begin in one hemisphere and spread to other Generalized seizures Involve both hemispheres KINDS OF SEIZURES Absence (petit mal): disturbances in consciousness Atonic: loss of muscle tone Myoclonic: muscles contract Tonic-clonic (grand mal): muscle contraction and loss of consciousness Generalized convulsive status epilepticus: seizures continue without recovery between them QUESTION Which type of seizure affects only one cerebral hemisphere? a. Partial b. Secondarily generalized c. Generalized d. All of the above ANSWER Partial Rationale: Partial seizures affect one cerebral hemisphere; secondarily generalized seizures begin in one hemisphere and then spread to the other side; generalized seizures involve both hemispheres. a. DEMENTIAS Many dementias are associated with abnormal inclusions in the brain Alzheimer disease: amyloid plaques Pick disease: Pick bodies Prion diseases: prion proteins Creutzfeldt-Jakob disease ALZHEIMER DISEASE (50 – 70 % OF DEMENTIA) Amyloid-beta protein-forming plaques Neurofibrillary tangles Decreased acetylcholine production ALZHEIMER DISEASE Characterized by loss of neurons and ventricular enlargement ALZHEIMER DISEASE LOSS OF FUNCTION Normal function Alzheimer function ALZHEIMER DISEASE A healthy neuron (top right) contrasted with a damaged neuron (note its shriveled state and the presence around the nucleus of neurofibrillary tangles) Tom Dolan, UK Medical Illustrator ALZHEIMER DISEASE amyloid precursor protein normally soluble protein fragments cleared away in Alzheimer disease amyloid b stick together to form fibrils amyloid plaques STAGES OF ALZHEIMER DISEASE First: short-term memory loss Second: confusional stage Disorientation, lack of insight, impaired hygiene and language use, sundown syndrome Third: incontinence, inability to recognize family and friends OTHER CAUSES OF DEMENTIA Microinfarcts: vascular dementia Vitamin B12 deficiency: Wernicke-Korsakoff syndrome Inherited atrophy of brain structure: Huntington disease QUESTION Which cause of dementia is vascular in nature? a. Alzheimer b. Microinfarcts c. Vitamin B12 deficiency d. Inherited ANSWER Microinfarcts Rationale: Small infarctions cause blood flow to be cut off to certain areas of the brain, causing tissue death. Depending on the extent of the infarctions, the dementia may be more or less severe. b.