Laser Surgical Treatment of the Glaucomas
advertisement
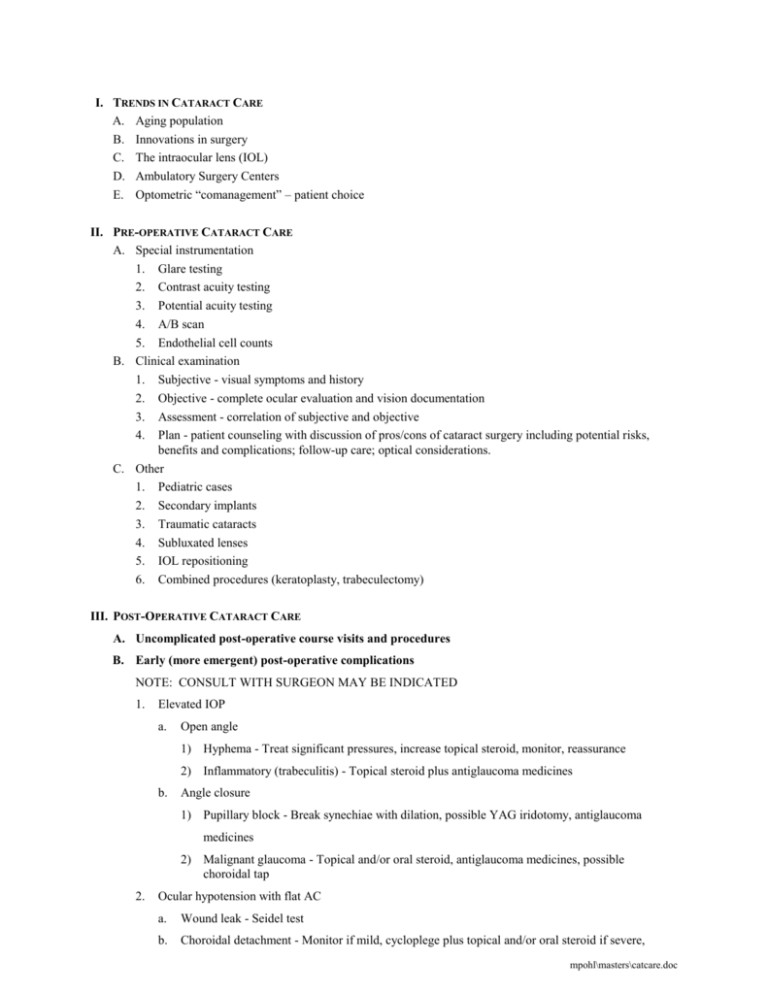
I. TRENDS IN CATARACT CARE A. Aging population B. Innovations in surgery C. The intraocular lens (IOL) D. Ambulatory Surgery Centers E. Optometric “comanagement” – patient choice II. PRE-OPERATIVE CATARACT CARE A. Special instrumentation 1. Glare testing 2. Contrast acuity testing 3. Potential acuity testing 4. A/B scan 5. Endothelial cell counts B. Clinical examination 1. Subjective - visual symptoms and history 2. Objective - complete ocular evaluation and vision documentation 3. Assessment - correlation of subjective and objective 4. Plan - patient counseling with discussion of pros/cons of cataract surgery including potential risks, benefits and complications; follow-up care; optical considerations. C. Other 1. Pediatric cases 2. Secondary implants 3. Traumatic cataracts 4. Subluxated lenses 5. IOL repositioning 6. Combined procedures (keratoplasty, trabeculectomy) III. POST-OPERATIVE CATARACT CARE A. Uncomplicated post-operative course visits and procedures B. Early (more emergent) post-operative complications NOTE: CONSULT WITH SURGEON MAY BE INDICATED 1. Elevated IOP a. Open angle 1) Hyphema - Treat significant pressures, increase topical steroid, monitor, reassurance 2) Inflammatory (trabeculitis) - Topical steroid plus antiglaucoma medicines b. Angle closure 1) Pupillary block - Break synechiae with dilation, possible YAG iridotomy, antiglaucoma medicines 2) Malignant glaucoma - Topical and/or oral steroid, antiglaucoma medicines, possible choroidal tap 2. Ocular hypotension with flat AC a. Wound leak - Seidel test b. Choroidal detachment - Monitor if mild, cycloplege plus topical and/or oral steroid if severe, mpohl\masters\catcare.doc c. choroidal tap if persistent or diminishing vision Ciliary body shutdown - Monitor 3. Endophthalmitis - IMMEDIATE TREATMENT; may include topical, injectable, and oral antibiotics and steroids, vitrectomy, IV medicines, hospitalization 4. Iris prolapse/vitreous to wound - Lysis with YAG laser; surgical repair of iris, anterior vitrectomy 5. Retinal break/detachment - Treatment may include laser photocoagulation, cryopexy, pneumopexy, scleral buckling 6. IOL dislocations - Surgical relocation or replacement C. Early (less emergent) post-operative complications 1. Glaucoma (steroid-induced) - Antiglaucoma medicines; consider other steroid or NSAID 2. Hyphema - Treat significantly elevated IOP, increase topical steroid, monitor, reassurance 3. Persistent iritis - Topical steroid 4. Wound leak with well-formed AC - Pressure patch with Ab ung, stop topical steroid, monitor 5. Retained lens material 6. a. Cortical - Monitor; increase topical steroid if increase inflammatory response b. Nuclear – Surgical removal; increase topical steroid IOL malpositions a. Decentrations - monitor; consider repositioning or replacement if visual symptoms significant b. Pupillary capture – Monitor; consider repositioning or replacement if visual symptoms significant 7. Diplopia - Monitor; consider prism or surgical correction if persisting at time of spectacle Rx. 8. Ptosis - Monitor; consider surgical repair if persisting after 3 months 9. Corneal edema 10. a. Epithelial - If persistent, hypertonic solution and/or ointment b. Stromal - Monitor, increase topical steroid or add NSAID c. Striate keratopathy - If persistent, may be secondary to inflammation or high IOP; treat accordingly Anterior ischemic optic neuropathy (AION) – Rule out temporal arteritis D. Intermediate to late post-operative complications 1. Cystoid macular edema (CME) – Topical/periocular/oral corticosteroids and/or topical/oral NSAIDs 2. Corneal decompensation (pseudophakic bullous keratopathy) - Treatment may consist of hypertonic solution and/or ointment, topical steroid and/or NSAID, and antiglaucoma medicines; consider PKP in persisting, visually debilitating cases 3. Recurrent iritis - Topical steroid 4. Glaucoma - Antiglaucoma medicines, steroids if inflammatory etiology 5. Diplopia - Differential diagnosis is important to rule out other etiologies such as mass lesion, vascular, myasthenia gravis; treat symptoms and consider referral to neuroophthalmology or neurology 6. Ptosis – Determine etiology; consider surgical repair if persisting and stable after 3 months 7. Retinal detachment – Same approach as early complication mpohl\masters\catcare.doc