Dermatology in Family Medicine
advertisement

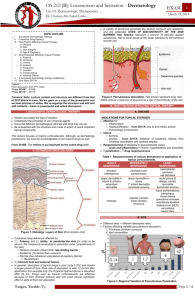
Dermatology in Family Medicine 1 Clerkship Briefing Dr. Clayton Dyck Dermatology in Family Medicine 1 (Or, How To Suck Less in Derm) Clerkship Briefing Dr. Clayton Dyck Objectives 1. 2. 3. 4. Use appropriate terminology to describe common skin presentations seen in family medicine Apply a systematic approach to their diagnosis Know the modalities used in their treatment Understand basic principles of topical therapy A call from Victoria Beach… Dermatologic Diagnosis Approach is same as for any other medical condition: History Examination Formulate differential diagnosis Apply investigations to confirm/rule out Dermatologic Diagnosis Use whatever algorithm you like: TTIINNMAP VITTAMIN DD CITTIN VD Tools Used in Dermatologic Assessment Our ears Our eyes Our hands Our noses (thankfully infrequently!) Lab tests Biopsies Scrapings/clippings Blood and urine samples Questions to ask Onset Pattern Skin symptoms Systemic symptoms Related factors Environmental Occupational Other medical conditions Drugs Others affected? To name a few… An overview of terms… macule papule plaque nodule pustule vesicle bulla ulcer wheal purpura excoriation papulosquamous Some Common Conditions Herpes Zoster VZV reactivation Pain may precede rash Usually dermatomal Crusts usually fall off in 2-3 weeks Worse in immunocomprimised, elderly Herpes Zoster - Treatment Wet dressings Antivirals May reduce post herpetic neuralgia Within 48-72 hours of vesicle appearance Eg famcyclovir 500 mg tid x 7 days Ophthalmic Zoster Treatment Hutchinson’s sign Refer to ophthalmologist urgently 50% complications if antivirals not given Tinea infections Dermatophytes, candida Topical antifungals Keep dry! If resistant/severe consider Scraping DM, immunocomprimised PO antifungals Onychomycosis Trichophyton sp., Candida Do KOH prep, culture first Topical treatment only in simple cases Usually needs oral treatment Eg Lamisil 250 mg od x 12 weeks Watch for toxicity Dyshydrotic Eczema Common if hands frequently moist/wet Consider other irritants, allergens, fungi Watch for superinfection Treatment: Moisturize x 3 Topical steroids (usually moderate to high potency) Topical immune modulators Psoriasis Peaks in 20s and 50s Multifactorial Exacerbated by trauma, infections, drugs, winter 5-8% have psoriatic arthritis Psoriasis - Treatment Topical tar (ick!) High - ultrahigh potency steroids Vitamin D analogues Phototherapy Immunosuppressive agents Topical Therapy Choice of vehicle important: Powder Paste Solutions (water or alcohol based) Gels Lotions Creams Ointments Topical Therapy Usually only a thin layer needed 1 gram = 10 cm x 10 cm area OD to BID usually sufficient Topical Steroids Consider thickness of skin, thickness of lesion, moistness of area Choose one drug of each potency Consider occlusion with lower potency steroids Avoid extended periods of treatment Topical Steroids - Examples (by potency) Low Hydrocortisone 1 % Medium Betamethasone 0.1% High Mometasone Ultrahigh Augmented betamethasone Topical Steroids - Adverse Fx Irritation Hypopigmentation Skin breakdown Rebound phenomenon Atrophy Striae Systemic adsorbsion And many more! Nevus Superficial spreading melanoma Basal cell carcinoma Cherry hemangioma Actinic keratosis When to biopsy Change in: Colour Size (<6 mm) Shape Especially if weeks to months, rather than months to years Bleeding Any doubt Impetigo S. aureus, S. pyogenes, or both Common in schools, daycares Treatment Bactroban tid x 10 days Cloxacillin 250 qid x 5-10 days Keflex 250 qid x 5-10 days Resistance common, may need swab Consider Bactroban in nares bid x 5 days Fifth’s Disease Parvovirus B19 Peaks in school age children Mild flu-like symptoms Arthritis in 10% Teratogenic, especially before 20 weeks Erysipelas Group A Streptococci Sudden onset, can be painful Fever, sick Penicillin V po/iv for 2 weeks Macrolide if penicillin allergic Hand Foot and Mouth Disease Coxsackie A16 virus Mild flu Sx, fever Usually children < 5 years Self limited, resolve within 10 days Scabies Itchy - worse at night Usually more than one family member A great mimic - consider if: Impetigo Eczema Idonomata Scabies - Treatment Treat family concurrently Wash all clothes/bedding/towels Permethrin cream Everywhere but hair, mouth, eyes Rinse after 12 hours Infants - precipitated sulfur Consider 2nd treatment Itchiness persists days to weeks later Some short snappers Pityriasis rosea paronychia Molluscum contagiosum rosacea Stasis dermatitis wart Subungual hematoma Take home “berries” Know your terminology When in doubt - back to first principles Always keep a differential diagnosis Use the right topical for the job Don’t be afraid to overbiopsy Objectives 1. 2. 3. 4. Describe common skin presentations seen in family medicine Apply a systematic approach to their diagnosis Know the modalities used in their treatment Understand basic principles of topical therapy References Skin Diseases: Diagnosis and Treatment, T P Habif et al, Elsevier 2005 Color Atlas and Synopsis of Clinical Dermatology, T B Fitzpatrick, McGraw-Hill, 1997 Images.MD (NJM Library Database) http://missinglink.ucsf.edu/lm/DermotologyGloss ary Questions? Or itching to leave?