Guidelines on Indications of Use of Steoroids
advertisement
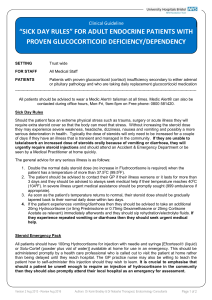
Guidelines on Indications of Use of Steroids Annie Kung Specialist in Endocrinology, Diabetes & Metabolism Types of Steroids • • • • • • Replacement Therapy glucocorticoid (hydrocortisone) mineralocorticoid (fludrocortisone) Anti-inflammatory Therapy Short acting: hydrocortisone Intermediate acting: prednisolone; methylprednisolone; triamcinolone • Long acting: dexamethasone Chinese Translation for Steroid From Google; English-Chinese Dictionary Steroid 類固醇 Corticosteroid類固醇;皮質類固醇; 糖皮質激素;皮質激素 Hydrocortisone副腎荷爾蒙;腎上腺荷爾蒙 Routes of Administration • Systemic : oral, transrectal, IV, IM • Local: topical, intranasal, intraocular, intraarticular Availability of International Guidelines on Use of Steroid • No one-for-all guideline • Glucocorticoid Replacement Therapy : Guidelines published by Royal College of Physicians of London, UK ; not available from Endocrine Society, USA. • Systemic Use of Glucocorticoid: Guidelines available for EULAR (European League for Rheumatology) • Local Use of Steroid: guidelines on individual disease, general guidelines not available Royal College of Physicians of London Guidelines on Glucocorticoid Replacement Therapy • • • • • • • Recommended Daily Dose for Glucocorticoid Hydrocortisone (cortisol) 15-30mg Cortisone acetate 25-37.5mg Prednisolone 5-7.5mg Dexamethasone 0.5mg Recommended Daily Dose of Mineralocorticoid Fludrocortisone 100-200mcg Monitoring hydrocortisone replacement • Hypoadrenalism is a rare condition and should be managed by a specialist • Biochemical monitoring enables detection of minor degrees of under- or over-replacement • Symptoms of hypo- or over-replacement are vague • 24 h urine free cortisol measurement should be in the normal range; mid-day and evening plasma cortisol should be >50nmol/l Long-term Follow Up • Regular review • Steroid card/bracelet/medallion indicating the diagnosis and replacement therapy • Advice for concurrent illness management and augmentation of replacement dose; IV therapy for surgery/hospitalisation • College of Physicians London, UK recommend patients on glucocorticoid replacement longterm FU by endocrinologist EULAR evidence-based recommendations on the management of systemic glucocorticoid therapy in rheumatic diseases J N Hoes et al, Ann Rheum Dis 2007;66:1560–1567 EULAR Expert Recommendation • Top Number 1 Recommendation • 1 a The ADVERSE effects of glucocorticoid therapy should be considered and discussed with the patient before glucocorticoid therapy is started • 1 b This advice should be reinforced by giving information regarding glucocorticoid management • 1 c If glucocorticoids are to be used for a more prolonged period of time, a ‘‘glucocorticoid card’’ is to be issued to every patient, with the date of commencement of treatment, the initial dosage and the subsequent reductions and maintenance regimens Hoes et al Ann Rheum Dis 2007 EULAR Recommendation on Systemic Steroid • Initial steroid dose/dosage reduction/long-term dosing depends on underlying rheumatic disease, disease activity, patient response • Comorbidity should be evaluated: hypertension, DM, peptic ulcer, fractures and osteoporosis, cataract/glaucoma, infection, dyslipidaemia, NSAID • Monitoring: body weight, BP, oedema, lipid, glucose, ocular pressure, cardiac insufficiency • Prevention of bone loss with antiresorptives+calcium+Vitamin D (assess of steroid dose/duration/BMD) • Children should be monitored for growth • IV Steroid during surgery if systemic steroid is used for >1 month • Gastric protection if concomittent use of NSAID Intra-articular Steroid Injection • First use dated back to 1951 by Hollander et al for arthritic joints; evidence for effectiveness was based on anecdotal studies rather than placebo-controlled trials • Few facts but mostly opinions about diagnosis, which lesions to treat, optimal steroid choice, dosage, injection techniques, intervals, frequency • Triamcinolone; methylprednisolone; dexamathesone. • Insoluble/long-acting steroid remained in the joint, contact with inflamed synovial surface, taken up by synovial cells and absorbed into blood stream • Similar side-effects as systemic steroids although the percentage of patients having side-effects is less • Recommendation: injection by trained personnel, e.g. rheumatologist, orthopaedic surgeon, orthopaedic physiotherapists practitioners in certain countries Common Indications for Local Steroid Injection • • • • • • • • Trigger finger Carpel tunnel syndrome De Quervain’s tenosynovitis Joint Arthritis Chronic spinal pain/facet joint pain Sacroiliac joint arthritis Osteoarthritis Rheumatoid arthritis Side-effects of Steroid Injection Therapy • • • • • Systemic Side-effects Facial Flushing Menstrual Irregularity Hyperglycaemia Suppress pituitaryadrenal axis • Emotional upset • Anaphylaxis • Local Side-effects • Post-injection flare of pain • Skin depigmentation • Subcutaneous atrophy • Bleeding • Infection • Steroid Arthropathy • Tendon rupture/atrophy • Soft tissue calcification Frequency of Intra-articular Steroid Injection • Prolonged steroid injection is associated with osteonecrosis • Injection frequency into major joints in lower limbs at no less than 3-4 month intervals. This is based on consensus rather than evidence • Joint sepsis is a known complication but rare (1 in 17,000-77,000) • Injection should be given by trained personnel Use of Topical Corticosteroids according to British National Formulary • Indications: inflammatory condition of the skin other than infection. • Common indications: eczema, contact dermatitis, insect sting, eczema of scabies • Contraindications: infection (bacteria/viral/fungal), rosacea • Use of systemic and potent steroid in psoriasis should be avoided or given only under specialist supervision • BNF Formulary Guide: potency grouped as Mild/Moderate/Potent/Very Potent • Potent topical steroid should generally be avoided on the face and skin flexures except under special circumstances by specialist supervision • Intralesional steroid injection should be reserved by severe cases/localised lesions, eg keloid scars, hypertrophic lichen planus, alopecia areata Side-effects with topical Steroid • • • • • • • • Spread/worsening of untreated infection Thinning of skin Irreversible striae and telangiectasia Contact dermatitis Perioral dermatitis Acne, worsening of acne rosacea Depigmentation hypertichosis Caution with Topical Steroid • No more frequently than twice daily, apply thinly to the affected area only • Use the least potent formulation which is fully effective • Avoid prolonged use on the face and keep away from eyes • Caution in children and during pregnancy • Suppression of pituitary adrenal axis and even cause Cushing’s syndrome with prolonged use in large area