Dermatology
advertisement

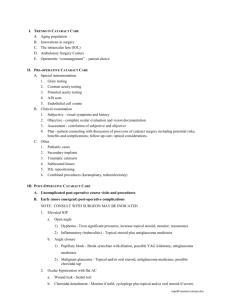
OS 212 [B]: Locomotion and Sensation - Dermatology Lec 10: Dermatologic Therapeutics March 19, 2014 Dr. Charissa Mia Salud-Gnilo TOPIC OUTLINE I. Successful Dermatologic Therapy II. Cutaneous Drug Delivery III. Host Factors Affecting Topical Therapy A. Disaese B. Site C. Skin Integrity D. Age & Pregnancy IV. Drug Properties Affecting Topical Therapy A. Potency B. Occlusion C. Vehicle D. Amount E. Frequency F. Duration G. Compounding H. Adverse Effects V. A successful dermatologic therapy (additional) VI. Quiz (from 2017A) 1 A variety of structures penetrate the stratum corneum and epidermis and are potenstial SITES OF DISCONTINUITY OF THE SKIN BARRIER. Hair follicles represent a resrvoir of topically applied substances. Hair is most dense at the scalp, followed by the forehead and the calf. Legend: From discussion, from PPT notes “From 2016B” – 2016B “From 2017A” – 2017A Transers’ Note: Lecture content and structure are different from that of 2017 Block A trans. Ma’am gave us a copy of the powerpoint and we took pictures of slides. We re-organize the structure and edit and add contents – basis is powerpoint and actual discussion. Figure 2. Percutaneous absorption. Red arrows represent drug. Hair follicle acts as a reservoir of drug and as a site of discontinuity of the skin. I. SUCCESSFUL DERMATOLOGIC THERAPY A. DISEASE Assess accurately the type of eruption Understand the principles of use of topical agents Know the different dermatological vehicles and what they can do Be acquainted with the structure and mode of action of some important topical compounds This lecture focuses on topical corticosteroids. Although, as dermatology practitioners, we must be knowledgeable of non-topical drugs as well. From 2016B: The vehicle is as important as the active drug itself. II. CUTANEOUS DRUG DELIVERY III. HOST FACTORS AFFECTING TOPICAL THERAPY INDICATIONS FOR TOPICAL STEROIDS effective for: o inflammation o hyperproliferation – from 2017A: due to anti-mitotic activity o immunologic involvement relieve o burning o pruritus – from 2017A: inhibition of histamine release, thus inhibiting vasodilation and cytokine release Responsiveness of diseases to glucocorticoids varies. o acute and inflammatory > chronic, hyperkeratotic and lichenified penetration – drug responsiveness Table 1. Responsiveness of various dermatoses to application of topical corticosteroids. HIGHLY MODERATELY LEAST RESPONSIVE RESPONSIVE RESPONSIVE palmoplantar proriasis psoriasis trunk psoriasis intertriginous parapsoriasis nail psoriasis atopic dermatitis in atopic dermatitis in acute phase of infants & children adults allergic contact seborrheic 1o irritant dermatitis dermatitis dermatitis nummular eczema dyshidrotic eczema lupus erythematosus pemphigus lichen planus papular urticaria granuloma annulare intertrigo lichen simplex necrobiosis lipoidica chronicus diabeticorum (NLD) sarcoidosis insect bites B. SITE Figure 1. Histology: Layers of Skin (from lionden.com) Cutaneous drug delivery is affected by 1.) Potency and 2.) ability to penetrate the skin (In order to be absorb, the compound necessitate to penetrate some compartments of the skin) o Stratum corneum (20um thick; rate limiting barrier o Epidermis (5x thicker than corneum) o Dermis (has cutaneous vasculature at papillary dermis) Bloodstream 3.) Inherent host and external factors In general, absorption of topical drugs is poor (only 1-2%) and require a longer period of time. Peak rate of absorption is after 12-24 hrs after application. For example only 2% of topical Hydrocortisone is absorbed after 24 hrs. Drugs such as topical corticosteroids are effective because of their inherent potency and can exert clinical significant effect in spite of their low absorption. Tangco, Turalde, Ty Different sites = different absorption rates Factors affecting variable percutaneous absorption: 1. Thickness (stratum corneum) 2. lipid composition Figure 3. Regional Variation of Percutaneous Penetration Page 1 / 4 OS 212 Lec 10: Dermatologic Therapeutics thickness of the stratum corneum penetration responsiveness and local side effects Table 2. Regional variation in percutaneous penetration of hydrocortisone in man. SITE % ABS SITE % ABS sole of the foot back 0.14 1.7 ankle (bilateral) scalp 0.42 3.5 palm axilla 0.83 3.6 Forearm (ventral) forehead 1 6 forearm (dorsal) eyelid 1.1 42 C. SKIN INTEGRITY diseased skin – altered stratum corneum (/ penetration) increase penetration of topical meds Skin integrity affects BIOAVAILABILITY There is increased penetration in o Inflamed diseased skin o Hydrated skin In atopic dermatitis, the penetration is 2-10x greater than that through healthy skin D. AGE EXTREMES & PREGNANCY PEDIATRIC CONSIDERATIONS More susceptible to the side effects of topical drugs due to : o Greater skin surface area-to-body weight ratio (2.5-to 3x that of adults) o fragile skin o decreased drug metabolism o Use the lowest potency corticosteroid that is effective. Occlusive coverings may increase percutaneous absorption. need for a less potent drug PREGNANCY fetal risk categories A-C IV. DRUG PROPERTIES AFFECTING TOPICAL THERAPY A. POTENCY Describes the intensity of a topical corticosteroid’s clinical effect. From 2017A: potency – efficacy – side effects; important to approximate side effects with desired therapeutic effect Table 5. WHO corticosteroid potency classification. INCLUSION HYDROCORTISONE methylprednisolone, prednisolone DESONIDE, TRIAMCINOLONE clobetasone, hydrocortisone butyrate, hydrocortisone buteprate, flumetasone, alclometasone, BETAMETHASONE, FLUOCINOLONE ACETONIDE, FLUOCORTOLONE, DIFLUCORTOLONE, III FLUOCINONIDE, MOMETASONE, (potent) METHYLPREDNISOLONE ACEPONATE hydrocortisone aceponate IV CLOBETASOL (very halcinonide potent) CAT I (weak) II (mod. potent) From 2016B: memorize the drugs in all caps, Dr. Salud-Gnilo did not mention anything about memorizing the ones in allcaps. GERIATRIC CONSIDERATIONS Increased risk for side effects from topical corticosteroids o thinness and fragility secondary to age-related skin atrophy. Similar precautions as with infants and children should be taken From 2017A: Because of the reasons above, infants and the elderly (age extremes) are more prone to the side effects of corticosteroid treatment. As such, the lowest potency drug that is effective is used. CONSIDERATIONS DURING PREGNANCY From 2017A: o fetal risk should be minimal to none o as much as possible, use category A and B drugs o category C (used only after careful consideration the patient’s case; risk-benefit assessment) CAT A B C D X Table 3. FDA pregnancy categories for drugs. INCLUSION no fetal risk in controlled studies no risk to human fetus despite possible animal risk OR no risk in animal studies but human studies lacking human risk cannot be ruled out animal studies may or may not show risks evidence of risk to human fetus contraindicated in pregnancy some oral and topical drugs are excreted in breast milk no adverse effects on lactation from the use of topical corticosteroids has been documented Application of topical drugs to the breasts should be done immediately following nursing to allow as much time as possible before the next feeding or not less than 2 hrs. to the next feeding. Table 4. (From 2017A) Summary of Host Factors Affecting Topical Therapy DISEASE Presentation Site acute, inflamed, abraded, eczematized, hydrated skin thickness (-) lichenified hair follicles penetration drug responsiveness need for a more potent drug AGE EXTREMES skin thickness penetration drug effect kidney, liver function elimination side effects Tangco, Turalde, Ty Figure 4. Topical Corticosteroids – Efficacy correlates with side effects. The more potent the steroid, the greater the side effects B. OCCLUSION Occlusion can increase drug delivery from 10 to 100 times. Immerse in water for 5 minutes Apply airtight dressing (vinyl/cotton gloves, socks, plastic wrap) E.g. Medication impregnated in an airtight dressing/tape ex. Flurandrenolide –Cordran Up to 10x increase in steroid penetration Can be used in combination with all vehicles Often used overnight Watch out for: Irritation, folliculitis and infection C. VEHICLE serve as carrier for the active drug adjunct for skin hydration augmentation of drug penetration Excipient (Vehicle) + Active Ingredient = DRUG Table 6. Different vehicles. PREP COMP’N MOISTURE ointment water in oil very moisturizing cream oil in water mod. moisturizing gel lotion immune function solution cellulose + alcohol/ acetone oil in water + alcohol alcohol drying DERMATOSES thick lichenified scaly acute subacute weeping SITE COSMESIS IRRITATION palmar plantar very greasy low moist, intertriginous occluded areas, scalp, hair-dense, mucosa variable elegant elegant high If lesion is wet, dry it (cream – mod. moisturizing only). If it’s dry, moisturize it (ointment). Page 2 / 4 Lec 10: Dermatologic Therapeutics D. AMOUNT Figure 5. Fingertip Guide for the Amount of Topical Steroid. One fingertip unit (FTU) – distal IP joint to tip of finger equivalent to 0.5g of steroid From 2017A 1-3% body surface area = 1 FTU = 1/2 g steroid Table 7. Fingertip unit requirements for adults. BID (g) BID (g) BID (g) AREA FTU APP’N, 7 APP’N, 4 APP’N days weeks face and neck 2.5 2.5 17.5 70 anterior/posterior 7 7 49 196 trunk arm 3 3 21 84 hand (both sides) 1 1 7 28 leg 6 6 42 168 foot 2 2 14 57 BID means ‘bis in die’ which is Latin for twice daily. The face and neck requires 2.5 FTU (0.5g steroid/ftu) to cover the area per application, meaning 1.25 g should be applied. Hence, 2.5 g per day is needed for BID application, 7.5 g in 7 days, and 70 g in 4 weeks. May also serve as guide to prescribing clinician on how many tubes of medication to prescribe. OS 212 usually topical corticosteroid with: o antibiotics o antifungals o salicylic acid o tar o urea There are drugs in the market which contain almost all of the above. These should be avoided to prevent unwanted effects. Targeted therapy is still better - ↓ side effects H. ADVERSE EFFECTS Educating the public regarding the adverse effects of steroids is essential. Some of these are irreversible. generally uncommon local > systemic o striae (rubrae distensae) – irreversible o atrophy – irreversible o periorbital dermatitis – irreversible o steroid acne – reversible; monomorphic (magkakamukha) o easy bruisability o systemic – Cushing’s (Tx: discontinue or taper, supplemental oral steroids) critical – 50 g in a week will already have systemic side effects from 2017A; there could be HPA (hypothalamic-pituitary-adrenal) axis suppression, especially if drug is more potent (e.g. clobetasol) E. FREQUENCY usually 1-2x daily because absorption is 12-24 hours more frequently in: o skin with thick stratum corneum (e.g. palms, soles) o sites from which the medication is easily removed during normal activity (e.g. hands – washing) DEPOT Effect o Stratum corneum may act as a reservoir for TCS for up to 5 days. o Retention is TCS concentration and formulation dependent. o From 2017A: to lessen need for reapplication stored steroids for sustained release pilosebaceous unit – lipophilic drugs sweat glands – hydrophilic drugs “LESS IS MORE” o Benefits of less frequent application: ↓ side effects and tachyphylaxis ↑ patient compliance ↓ cost of therapy F. DURATION discontinue or taper potency when the skin lesion has resolved long term therapy may be used for chronic chronic skin disease that is responding to treatment with the medication – watch out for tachyphylaxis Every-other-day therapy or weekend-only (pulse therapy; e.g. psoriasis treatment regimen wherein vit.b analog is given during weekends and steroid during weekday) application for chronic conditions limit to </= 3 weeks for superpotent drugs up to </= 3 months for midpotent drugs clinically, 2 week course then reassess if used >3 weeks, do not discontinue abruptly, taper to avoid rebound and systemic side effects G. COMPOUNDING combination of active drugs <1% prescriptions assess compatibility, stability and interaction of drugs Tangco, Turalde, Ty Figure 6. (first row L to R) Striae, Skin atrophy, easy bruisability (second row L to R) perioral dermatitis, steroid acne dependent on: o chemical nature / potency of the drug o vehicle o site o patient population o duration Treatment is PREVENTION o Adverse effects are avoided by discontinuing or tapering there have been deaths from overzealous use of topical corticosteroids consider referral to endocrinologists HPA AXIS SUPPRESSION: TREATMENT withdraw the topical corticosteroid reduce the frequency of application substitute a less potent steroid consider referral to endocrinologists For S/Sx of glucocorticoid insufficiency: o supplemental systemic corticosteroids o tapering topical corticosteroids V. A SUCCESSFUL DERMATOLOGIC THERAPY (ADDITIONAL) Assess accurately the type of eruption Understand the principles of use of topical agents Know the different dermatological vehicles and what they can do Be acquainted with the structure and mode of action of some important topical compounds The aspects mentioned above comprise a successful dermatologic therapy. However, those are not complete and holistic. A practitioner must also consider the aspect of ACCESS. Access entails: o 1) Rational selection o 2) affordable prices o 3) sustainable financing o 4) reliable health and supply systems Dr. Gnilo’s sharing: The department is organizing a community dermatology program at AMIGA (Alfonso, Mendez, Indang, Gen. Aguinaldo, Amadeo) Municipalities of Cavite wherein residents go to Page 3 / 4 Lec 10: Dermatologic Therapeutics the community to man skin clinics. One of their colleagues assessed the prevalent skin condition in AMIGA and the drugs available in the locality. Prevalent conditions include: scabies, fungal, bacterial, eczematous disease, contact dermatitis, acne and lice. No permethrin (anti-scabies), terbinafines (for dermatophytes). There are sources for mupirocin, oral antibiotics, and topical steroids. What their colleague did was to search literature on alternative remedies for prevalent conditions. The remedies are as follows: wheatfield ointment (for tinea), azoles (for tinea), benzyl benzoate (for scabies). As for sustainable financing, they urged AMIGA officials to buy dermatologic therapeutics by bulk to lessen cost. ESSENTIAL MEDICINES intended to be available within the context of functioning health systems at all times, in adequate amounts, in the appropriate dosage forms, with assured quality, and at a price the individual and the community can afford. OS 212 THIN ATROPHIC SKIN From 2017A: low potency From 2016B:low potency, do not occlude DRY XEROTIC SKIN VI. QUIZ (FROM 2017A) Given the following skin conditions, what are the appropriate dermatologic therapeutic agent and vehicle. DRY LICHENIFIED SKIN From 2017A: moderately potent cream (mildly moisturizing) compounded with petroleum jelly (an ointment, hence moisturizing); lotion with emollient (moisturizing) From 2016B: moderate to high potency; combination, potent then shift END OF TRANSCRIPTION From 2017A: potent ointment (moisturizing) compounded with keratolytic agents, occlude From 2016B: moderately potent, occlude OR potent, taper to mid-potent or decrease frequency; consider socioeconomic status (potency = price) WET ECZEMATOUS SKIN Wilson: Ginandahan, sinipagan, at binuhusan naming ng pagmamahal ang trans na ito :D Nawa’y iboto n;yo kaming best transers sa 2017 Awards! Ang bumoto samin, may exclusive access sa event sa baba: IMPORTANT ANNOUNCEMENT! From 2017A: low potency using a drying vehicle (cream – mildly hydrating, lotion/gel – irritating) From 2016B: low potency drug like hydrocortisone cream; antibiotics because to counter infectionz THICK SCALY SKIN From 2017A: potent ointment From 2016B: psoriasis – potent ointment/lotion (water-based because lesions are extensive), occlude, shift/taper to avoid adverse effect, maintenance at low potency; more than one formulation for maximum benefit Tangco, Turalde, Ty Page 4 / 4