tuberculin-type hypersensitivity
advertisement
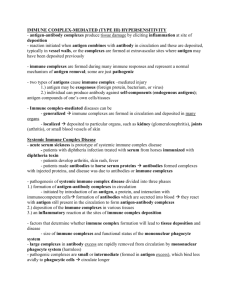
Chapter 25 Hypersensitivity (Type III) Trai-Ming Yeh, Ph.D. Department of Medical Laboratory Science and Biotechnology College of Medicine National Cheng Kung University Diseases caused by immune complexes can be divided into three groups. Persistent infection with a weak antibody response can lead to immune complex disease Renal artery FITC (green) anti-HBsAg Rhodamine (red) anti-IgM Immune complex disease is a frequent complication of autoimmune disease Immune complex following inhalation of antigen: extrinsic allergic alveolitis Precipitin antibody (P) present in the serum of a patient with pigeon fancier's lung (3) is directed against the fungal antigen Micropolyspora faeni. Normal serum (N) lacks antibodies to this fungus. Immune complexes can trigger a variety of inflammatory processes Type II and type III hypersensitivity cause damage by similar mechanisms Complement is an important mediator of type III hypersensitivity Autoimmunity causes immune complex disease in the NZB/NZW mouse Experimental models demonstrate the main immune complex diseases Injection of antigen into the skin of presensitized animals produces the Arthus reaction Type I 15 min Type III (Arthus reaction) 5-12 h Type IV 214-48 h CR1 on RBC readily binds immune complexes Immunocomplexes are transported to the liver and spleen, where they are removed by fixed tissue macrophages I-125 lable BSA /anti-BSA removed in liver Complement solubilization of immune complexes in vitro Complement can rapidly resolubilize precipitated complexes through the alternative pathway. 1. Non-erythrocyte-bound complexes are taken up rapidly by the liver (but not the spleen) and are then released to be deposited in tissues such as skin, kidney, and muscle, where they can set up inflammatory reactions. 2. Complement deficiency impairs clearance of complexes. The size of immune complexes affects their deposition 1. Larger immune complexes are rapidly removed 2. Phagocyte defects allow complexes to persist 3. Carbohydrate on antibodies affects complex clearance The class of immunoglobulin in an immune complex can also influence its deposition: IgM to IgG2a in SLE mice Ig classes affect the rate of clearance Immune complex deposition in the tissues results in tissue damage-But what cause it to deposit? • The most important trigger for immune complex deposition is probably an increase in vascular permeability-vasoactive amine antagonists, such as chlorpheniramine and methysergide prevent tissue damage (Fig. 25.18). • Immune complex deposition is most likely where there is high blood pressure and turbulence (Fig. 25.19)-kidney Summary of Chapter 25 Hypersensitivity (III) • Diseases caused by immune complexes can be divided into three groups. • Immune complexes can trigger a variety of inflammatory processes. • Experimental models demonstrate the main immune complex diseases. • Immune complexes are normally removed by the mononuclear phagocyte system. • The size of immune complexes affects their deposition. • Immune complex deposition in the tissues results in tissue damage. • Deposited immune complexes can be visualized using immunofluorescence. Chapter 26 Hypersensitivity (Type IV)antigen-specific CD4 T cells Trai-Ming Yeh, Ph.D. Department of Medical Laboratory Science and Biotechnology College of Medicine National Cheng Kung University THERE ARE THREE VARIANTS OF TYPE IV HYPERSENSITIVITY REACTION Contact hypersensitivity occurs at the point of contact with allergen (haptan) such as nickel, chromate… 1. Contact hypersensitivity is primarily an epidermal reaction, and the dendritic Langerhans' cell, located in the suprabasal epidermis, is the principal antigenpresenting cell (APC) involved 2. Birbeck granules, which are organelles derived from cell membrane and are characteristic of Langerhans' cells 3. Keratinocytes produce a range of cytokines important to the contact hypersensitivity response 1. A contact hypersensitivity reaction has two stagessensitization and elicitation 2. Sensitization (takes 10-14 days in humans) stimulates a population of memory T cells 3. Elicitation involves recruitment of CD4+ lymphocytes and monocytes Cytokines and prostaglandins are central to the complex interactions between Langerhans' cells, CD4+ T cells, keratinocytes, macrophages, and endothelial cells in contact hypersensitivity TUBERCULIN-TYPE HYPERSENSITIVITY 1. The tuberculin skin test reaction is an example of the recall response to soluble antigen previously encountered during infection which involves monocytes and lymphocytes 2. The tuberculin lesion normally resolves within 5-7 days, but if there is persistence of antigen in the tissues it may develop into a granulomatous reaction. GRANULOMATOUS HYPERSENSITIVITY • intracellular microorganisms such as M. tuberculosis and M. leprae, which are able to resist macrophage killing leads to chronic stimulation of T cells and the release of cytokines. • The process results in the formation of epithelioid cell granulomas with a central collection of epithelioid cells and macrophages surrounded by lymphocytes Macrophages, lymphocytes, epithelioid cell, and giant cells in granulomas • Granulomas occur with chronic infections associated with predominantly TH1-like T cell responses, such as tuberculosis, leprosy, and leishmaniasis, and with TH2-like T cells, as in schistosomiasis. • Epithelioid cells large and flattened with increased endoplasmic reticulum (Fig. 26.11) are derived from activated macrophage under chronic stimulation • Giant cells are formed when epithelioid cells fuse to form multinucleate giant cells (Fig. 26.12) Tuberculin-like DTH reactions are used practically in two ways: confirms past or latent infection with M. tuberculosis or measure of cell-mediated immunity IFNγ is required for granuloma formation in humans TNF and lymphotoxin-α are also essential for granuloma formation during mycobacterial infections TNF is essential for the development of epithelioid cell granulomas Many chronic diseases manifest type IV granulomatous hypersensitivity borderline leprosy has characteristics of both tuberculoid and lepromatous (no protection) leprosy tuberculoid-type reaction, lymphocyte proliferation or the release of IFNγ following stimulation with M. leprae antigens Tuberculosis is caused by M. tuberculosis • The reactions are frequently accompanied by extensive fibrosis and the lesions may be seen in the chest radiographs of affected patients • The histological appearance of the lesion is typical of a granulomatous reaction, with central caseous (cheesy) necrosis Summary of Chapter 26 Hypersensitivity (Type IV) • DTH reflects the presence of antigen-specific CD4 T cells. • Contact hypersensitivity occurs at the point of contact with an allergen. • Tuberculin-type hypersensitivity is induced by soluble antigens from a variety of organisms. • Granulomatous hypersensitivity is clinically the most important form of type IV hypersensitivity. • Many chronic diseases manifest type IV granulomatous hypersensitivity. Important points needed to understand after class • Understand the role of immune complex. • Understand the role of immune complex in tissue damage. • Understand the role of type IV hypersensitivity on diagnosis and treatment of various diseases.