Body
advertisement
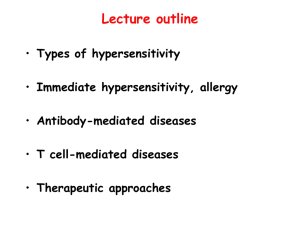
LEUKOCYTE/ IMMUNE SYSTEM DISORDERS VARIATIONS IN IMMUNE FUNCTION Fetal and Neonatal Immune Function Antibody, phagocytic and complement functions deficient at birth. Maternal antibodies are protective 5- 6 months Immune Function in Elderly Diminished T cell and antibody response Increased auto antibodies Factors Affecting System Stress Nutrition Drugs Other diseases • • • • renal failure malignancy diabetes mellitus systemic infections HYPERSENSITIVITY DISORDERS Type I Immediate—IgE mediated Type II Sub-Acute—IgG or IgM Type III Sub-Acute—IgG or IgM Type IV—Delayed –T Cell mediated Type I Hypersensitivity Allergies, anaphylaxis, anaphylactic shock anaphylactoid reactions Occurs in seconds to minutes IgE normally binds to surface of basophils and mast cells Concentrates in lining of respiratory and GI tracts, skin Fig 8-1 Fig 8-1 continued Type I Hypersensitivity Offending antigen enters body—ingestion, injection, inhalation • Peanuts, walnuts, latex • Any insect venom (bee stings) When appropriate antigen binds to 2 IgE molecules, they cross link • Histamine, leukotrienes, interleukins, kinins released Type I Hypersensitivity Get contraction smooth muscle, increased permeability of vessel walls Fluid leaks into interstitial space, smooth muscle in respiratory and GI tracts spasms Angioedema, esp of face, hands, feet Vessels not damaged If this is local, irritating but not likely to be fatal Signs of Anaphylaxis begin within seconds to minutes Body wide reaction to ingested, inhaled, injected ag Acute systemic reaction due to IgE release Urticaria Itching, laryngeal edema, angioedema Bronchospasm—may die from anoxia Hypotension—may die from hypotensive shock GI and UG cramping (least common) Administer epinephrine, establish airway, give antihistamines and glucocorticoids Atopy-chronic, inherited disorder IgE at mucosal surfaces reacts with normally innocuous compounds • Pollen, animal dander, certain types of foods Reaction is localized to surface stimulated Multiple manifestations Associated with increased incidence of allergic rhinitis and asthma Atopic eczema (atopic dermatitis) Associated with allergic rhinitis or asthma T helper 2 cells overproduce IL 31 (believed to be underlying problem) Weeping, eroded, red, scaly patches of skin • scalp, face, and diaper area most often affected • exacerbated by weather changes, drying from XS soap and water • severe itching2º bacterial infection Atopic eczema Atopic eczema (atopic dermatitis) May spontaneously disappear as child ages Other allergies commonly appear Areas of knee, elbow, neck, etc. involved if continues Points of flexion/extension May spread over entire body in adults—remission rare Treat with dietary restrictions (infants), moisturizers, antihistamines Antibiotics for skin infections Topical steroids/T cell modulators as needed Allergic rhinitis—nasal allergy Seen more in developed nations with high standards of cleanliness less exposure to pathogens and more exposure to chronic irritants Less development of the suppressor (regulatory)) T cells May predispose person to developing asthma Allergic Rhinitis--S&S Stuffy, runny nose; red, weepy eyes; itching of eyes and nose Dark circles under eyes, chronic sinusitis may develop May report ringing in ears or sensation of pressure in ear Eosinophils in nasal secretion distinguishes from infection Subsets of allergies Seasonal form (hay fever)—pollen, mold Perennial allergies—more likely dust mites, animal dander Cytotoxic (Type II) and Immune Complex (Type III) Diseases Type II involves antibodies binding cells— tissue specific reaction—rapid Type III involves antibodies binding soluble proteins—serum sickness • Develops 7-10 days after antigen is introduced • Urticaria, angioedema, fever, generalized lymphadenopathy • Activation of complement as complexes precipitate in capillaries • Joint pain, renal dysfunction, GI problems Fig 8.4 Type III Figure 8-5 Type IV Hypersensitivity—48-72 hours Allergic Contact Eczema—delayed hypersensitivity T lymphocytes Poison ivy, nickel allergies Weeping, red, puritic vesicles at site of contact Localized edema initially, thickening of skin if contact continues avoid offender, steroids as needed Contact dermatitis Fig 8-7 Type IV Fig 8-6 AUTOIMMUNE DISORDERS #3 cause of death in the US AI Disorders -- general Immune system must tolerate normal antigens by removing all T and B cells that would react with self proteins AI diseases occur when the immune system starts to attack the cell of the body—break in tolerance • Occur more frequently in females than males • Precise cause unknown—believe that foreign antigen resembles a self antigen • Several are associated with HLA antigens--see T 8-5 • Presence of one increases risk of others Relapse and remission common • Seem to get worse when stressed Immune system removes foreign compound first • Continued surveillance sees normal cell proteins presented by MHC I molecules as foreign, and attacks those cells • System eventually turns on to normal proteins Some suggestion that may start if inflammation accompanies apoptosis reaction AI diseases be cytotoxic T cell mediated or antigen-antibody reaction or both Organ specific AI diseases Damage is limited to one organ/tissue Rest of the body suffers as a result of damage done to that organ/tissue Examples Idiopathic thrombocytopenic purpura Autoimmune hemolytic anemia Type I Diabetes Mellitus Autoimmune thyroiditis Addison’s Disease Celiac Disease Multiple organ system AI diseases Most of these involve antibodies that react with the body’s connective tissue Examples Rheumatoid arthritis Systemic Lupus Erythematosis (SLE) Scleroderma Rheumatoid arthritis In women 2.5X as often as in men, peak incidence 40-60 years; 1% all adults Seems to have some association with HLA-DR4 (Minor HC) antigens (varies with ethnic group) Production of multiple destructive enzymes: collagenase, protease Attacks synovial membranes Produces granulation tissue that extends into jointspannus Destruction of cartilage, ligaments, tendons, bones Signs & Symptoms Fever, fatigue, malaise Swollen, painful joints; often bilateral Hands, knees, feet Morning stiffness that lasts > 1 hour Deformed joints as cartilage is destroyed Juvenile rheumatoid arthritis Systemic onset—boys and girls equally—20% poorest prognosis Multiple organs, any age Polyarticular onset—girls 2X as often as boys—40% 5 or more joints, and age Little involvement outside joints Pauciarticular onset—girls 6X as often as boys—40% best prognosis Max of 4 joints, typically < 6 yrs old Signs and symptoms of JRA Fatigue, anorexia, weight loss, fever Shifting, symmetrical polyarthritis; any diarthrotic joint is possible Morning stiffness of joints > 1 hour Erosive arthritis seen on X rays, followed by deformity Both age groups Rheumatoid nodules, usually indicates active or severe disease Damage to other organs—heart, lungs, eyes, blood vessels Normocytic, normochromic anemia if bone marrow is involved Turbid, non-viscous synovial fluid with high WBC count Increased T cell activity causes increased TNF, which causes increased osteoclast activity Rheumatoid factor in 85 % of pts IgM that reacts with altered human IgG Anti-gamma globulin factor Complexes ppt onto joint tissue, stim immune reaction May show up in other AI connective tissue diseases Seen in 5-20% of normal people Increased incidence as get older Systemic lupus erythematosis Signs and symptoms are diverse, easily missed in early stages Butterfly rash across face is classic sign (40% of cases) AB form vs nucleic acids (anti-nuclear antibodies) RBC, WBC, platelets, coagulation proteins, etc, Mild to rapidly fatal In US: incidence in Fe 10x M Incidence in Black Fe 8x White Fe Signs and symptoms of SLE Symmetric arthritis or joint pain (90%)—not erosive or deforming Fever, fatigue, weakness (50% have mild anemia), weight loss, possibly severe hair loss Vasculitis (80%) with butterfly rash that gets worse if exposed to sunlight Pleurisy chest pain; myocarditis, pericarditis Anemia or other marrow deficiencies Renal complications Antinuclear antibodies attach to DNA, deposit in glomerulus Complement attaches to immune complex, renal inflammation begins 65% of SLE pts develop glomerulonephritis 40% have clinical renal disease 25% have severe renal damage (renal failure) CNS complications usually fatal Diagnose with + antinuclear antibody test Scleroderma Now called Progressive Systemic Sclerosis Usually starts in 20‘s-40’s, least common of diseases mentioned here Disease is overproduction of collagen, may be localized or systemic Slow, progressive fibrosis of skin and other organs Proliferation of collagen in walls of blood vessels—lose elasticity Localized scleroderma—restricted to skin May occur as result of repeated exposure to some chemicals Milder, better prognosis Generalized scleroderma Limited cutaneous systemic sclerosis (Raynaud’s phenomenon) • Vasospasm when extremities are exposed to cold • Digits become white, then blue, then red in each attack • Thickening and tightening of skinsausage appearance Diffuse cutaneous—CT of skin and viscera, rapid progression Progression of Scleroderma Gradually spreads up limbs, involves trunk, face Very taut face, wrinkled mouth, smooth forehead Arthritis, joint pain and stiffness common Esophageal dysfunction, GI dysfunction Decreased pulmonary volumes Renal vessels damaged—proteinuria, hematuria, hypertension Renal failure is leading cause of death for generalized scleroderma