Dr.MOHAMED NASR
Lecturer Of
Dermatology & Venereology
Zagazig University
SYPHILIS
SYPHILIS
Syphilis is a chronic infectious sexually
transmitted disease capable of involving every
structure of the body.
Causative organism:
Treponema pallidum is a spirochaete, with the
following characters:
Slender, motile, and regular spiral organism.
6-15 microns in length, 0.25 micron in width and
formed of 8-24 coils.
Cannot be stained by ordinary bacterial stains and
appears pale (hence the name pallidum).
Diagnosis of syphilis:
1- Clinical examination.
2- Dark-ground examination.
3- Serological tests.
4- Other investigations.
Serological tests of syphilis:
A- Reagin tests or standard tests of
syphilis (S.T.S) or non-specific tests.
B- Specific tests.
A- Reagin tests or S.T.S.:
In the course of syphilis, an antibody (reagin)
appears in the serum of the patients.
This reagin may be demonstrated by using non-
treponemal antigen, i.e. antigen not extracted from
treponema pallidum.
There are 2 types of S.T.S.
1-Complement fixation test:
Wasserman reaction (W.R.):
The reagin unites with the detecting antigen in the presence
of complement.
The union is invisible and fixation of complement could be
detected by using another antigen –antibody system
(indicator system; sheep's RBCs+sheep'S RBCs antibody).
If haemolysis occurs this means the complement is not
fixed during the first reaction i.e the test is negative.
If no haemolysis ocurrs this means that the complement is
consumed and fixed in the first antigen antibody reaction, i.e
positive result.
2-Flocculation or precipitation tests:
a- Venereal Disease Research Laboratory Test
(VDRL): the antigen –antibody reaction gives
visible flocculation with no need for an indicator
system. This can be done in a test tube or on a
glass slide.
b- Kahn's test is also a flocculation test but is less
reliable than VDRL test.
The S.T.S. tests are:
Negative in the first stage (15-30 days after the
chancre has appeared) and become positive after that
period in 50% of cases and then increasing gradually
till the onset of secondary stage.
Positive in 100% of cases in the secondary stage.
Positive in 70-90% of cases of the tertiary stage.
B-Specific tests for syphilis:
Specific antibodies against Treponema pallidum
are found in the serum of syphilitic patients and
could be demonstrated by using treponemal
antigens. These tests include:
1-Treponema Pallidum
Immobilization Test (T.P.I.):
Specific antitreponema antibodies are found in
the serum of the patient.
They can immobilize T. pallidum when patient's
serum is put on living spirochetes suspension.
The test is positive when 70% or more of living T.
pallidum are immobilized.
2-Fluorescent Treponemal Antibody
Test (F.T.A.):
A diluted serum of the patient is added to a dried
drop of suspension of dead T.pallidum fixed on a
glass slide.
If the serum contains the antibody it will adhere
and coat the treponemes.
This could be detected by adding a fluorescent
substance and examining microscopically.
3-Treponema Pallidum
Hemoagglutination Test (T.P.H.A.):
Sheep erythrocytes which are sensitized to
Treponema and treated with tannic acid are added
to the patient's serum.
Haemagglutination of the erythrocytes means
positive results due to the presence of antiTreponema antibody in the serum.
Other investigations:
1. Cerebrospinal fluid (C.S.F.):
Examination to exclude or to diagnose neurosyphilis.
2. Radiological examination:
For diagnosis of late acquired syphilis and congenital
syphilis.
3. Biopsy:
a- Chronic inflammation with infiltration of lymphocytes and
plasma cells.
b- Endarteritis obliterans of the blood vessels.
c- Fibroblastic activity in the periphery of the lesion.
ACQUIRED SYPHILIS
Classification:
a. Early infectious phase (first 2 years of the infection):
1. Primary stage (3-9 weeks).
2. Secondary stage (3-9 months).
3. Recurrent stage (relapse).
4. Early latent stage (9 months - 2 years).
b. Late non-infectious phase (after 2 years of the infection):
1- Late latent stage.
2- Tertiary stage.
3- Cardiovascular and neurosyphilis.
Mode of infection:
a. Direct:
1. Sexual intercourse with infected partner.
2. Close contact with a syphilitic person e.g. kissing.
3. Touching a syphilitic lesion, e.g. doctors, nurses.
4. Blood transfusion from a syphilitic donor.
b. Indirect
1. Using infected materials, e.g. cups, spoons....etc.
2. Unsterilized medical instruments, e.g. needles.
A. EARLY INFECTIOUS PHASE
I. PRIMARY STAGE OF SYPHILIS
Incubation period: 9-90 days, (average 2-4 weeks).
a. Chancre
It is the first tissue reaction to treponemal infection.
It is an ulcer with the following characters:
1- Single but occasionally multiple.
2-Raised border, clean dull-red granulating floor and indurated base.
3- It oozes serum which dry giving yellowish gray crust and contains
treponemas.
4- Not painful not tender unless secondarily infected.
5- Does not bleed easily on manipulation due to end arteritis
obliterans.
It occurs on the genital areas (95%).
It may rarely occur on extragenital areas (5%).
The ulcer heals, if untreated leaving a thin, atrophic and noncontractile scar.
Special types of chancre:
1.
2.
3.
4.
5.
Kissing chancre: on contagious surfaces e.g scrotum,
thigh and lips.
Condom chancre: at the root of the penis of those
wearing condoms.
Concealed chancre: intracervical, intrameatal or
intraanal.
Chancre redux: recurrence of chancre at the site of
healed chancre, during the secondary stage.
Pseudochancre redux: is a gumma that appears at the
site of original chancre.
b. Regional lymph glands
Enlarged, firm rubbery and not matted.
Painless and not tender unless secondarily
infected.
The enlargement is bilateral in genital chancre and
unilateral in extragenital one.
Fate of primary syphilis:
30% of cases: the disease burns itself out.
30% of cases: become serologically positive for
life.
20% of cases: pass to benign tertiary syphilis.
20% of cases: pass to malignant syphilis.
Diagnosis:
1-Clinical examination.
2-Dark-ground examination.
3-Serological tests: they are negative early in this
stage (sero-negative) and later become positive.
Differential diagnosis
a. Genital ulcer:
1- Scabies.
2- Fixed drug eruption.
3- Herpes genitalis; grouped painful vesicles on an erythematous
base.
4- Soft sore (chancroid).
5. Lymphogranuloma Venereum: the ulcer is small and transient.
6. Granuloma inguinale: The genital ulcer may simulate chancre
but the lymph glands are not enlarged.
7. Malignant ulcer: the ulcer is indurated with rolled everted edge
and may be fixed to the underlying structure. Lymph nodes
enlargement late and they are stony hard.
8. Herpes Zoster: unilateral Grouped painful vesicles on an
erythematous base.
b. Extragenital chancre:
On the lips or tongue:
1. Primary tuberculous lesion.
2. Herpes simplex with secondary pyogenic infection.
3. Aphthous stomatitis.
On the nipple:
1. Simple fissuring.
2. Paget's disease.
On the anus:
1. Anal fissure.
2. Thrombosed external piles.
II. SECONDARY STAGE OF
SYPHILIS
It occurs in untreated patients, this stage starts
usually 6-8 weeks after the appearance of chancre.
It is characterized by:
1. Healing or healed chancre.
2. Skin rash.
3. Generalized lymphadenopathy.
4. Mucous membrane lesions.
5. Condylomata lata.
6. Other signs.
1. Healing or healed chancre:
The chancre may still be present or a scar may
be formed indicating its previous existence.
2. Skin Rash:
a. Widely spread, bilateral, symmetrical and more
prominent on the flexor surfaces.
b. Rounded, dull red in colour and polymorphic but
never vesiculates. No itching.
c. The rash is chronic and may persist for weeks or
months if untreated.
Four main types of rash occur:
1. Macular syphilid:
Rose pink in colour, discrete lesions distributed mainly on the chest,
back, abdomen and flexural surfaces
2. Papular syphilid:
According to their distribution they may get many descriptive names:
a. Corona veneris: line of papules on the forehead just below the hair
line.
b. Follicular syphilid: follicular papules related to the hair follicles.
These follicular papules when occurring on the scalp may lead to
irregular alopecia (moth-eaten alopecia).
3. Papulo-squamous syphilid:
These are papules with scaling which resulted from diminution of
the blood supply due to endarteritis obliterans.
4. Pustular syphilid:
The papules may undergo deep central necrosis giving the
appearance of a pustule.
3. Generalized lymphadenopathy:
- Non-painful, rubbery and discrete enlargement of
lymph glands are present in 50% of cases.
4. Mucous membrane lesions:
The characteristic lesion is the mucous patch
which is painless, grayish white patch edged by a
dull red border.
These patches may be present on buccal mucosa,
tongue, larynx and soft palate leaving erosion
which is, sometimes, called snail-track ulcer.
5. Condylomata lata:
These are papules, flat-toped, dull red or grayish
white (due to necrosis), with broad base and are
very infectious (the most infective syphilitic
lesions).
6. Other signs of secondary stage:
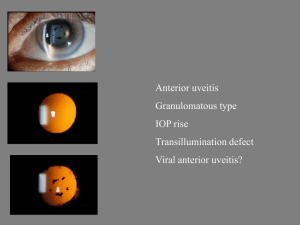
a. Hepatitis with mild jaundice.
b. Uveitis and choroido-retinitis.
c. Periostitis of long bones.
d. Onychia and paronychia.
e. Acute or subacute meningitis.
Diagnosis of secondary stage:
1. History and clinical examination.
2. Dark-ground examination from the moist lesions.
3. Serological tests for syphilis are 100% positive.
4. C.S.F examination: changes are found only in 1020% of cases (not routinely examined in
secondary stage).
III. STAGE OF RECURRENCE
(RELAPSE)
a. By relapse we mean return of the disease
(clinically or serologically) after its disappearance
with or without treatment.
b. This usually occurs in the first two years of
infection.
IV. EARLY LATENT SYPHILIS
At this stage, the patient is completely free of
signs and symptoms with positive blood tests for
syphilis.
This stage ends by the beginning of the third year
of infection.
B. LATE NON INFECTIOUS
SYPHILIS
This phase includes 3 stages:
1. Late latent sage.
2. Tertiary stage.
3. Cardiovascular and neurosyphilis.
1. LATE LATENT STAGE
This is the continuation of the early latent stage.
The disease in late latent stage may be discovered
by chance, e.g. during investigations done before
marriage, ante-natal care, before joining military
or governmental services.
The diagnosis of this stage depends upon positive
S.T.S. and should be confirmed by one of the
specific tests.
2. TERTIARY STAGE
This stage starts usually 3-10 years after infection.
The characteristic lesion of this stage is the
gumma which is a localized swelling, single or
multiple, varying in size from a pin-head to a
bigger mass several centimeters in diameter.
The gumma is characterized by:
a. Pathologically:
1. Central necrosis (due to endarteritis
obliterans) surrounded by: granulation tissue
infiltrated by plasma cells, lymphocytes and
fibroblasts.
2. No treponemas are present.
b. Clinically:
1. Asymmetrical and painless.
2. Single or in isolated groups.
3. Destructive (forming punched out ulcer)
4. Slow healing (forming thin atrophic scar).
5. It may affect:
Covering structures of the body, e.g. skin, mucous
membranes and subcutaneous tissues.
Supporting structures of the body, e.g. bones, joints, muscles
and ligaments.
Internal organs, e.g. stomach, intestines, liver, spleen, lung
and testis.
The gumma involving the skin is either:
1. Nodular.
2. Squamous or psoriasiform lesion; a nodule with
waxy scaling. It may occur on the palms and soles
leading to unilateral hyperkeratosis.
3. Subcutaneous; which may be ulcerated, giving
gummatous ulcer which is: punched out with
vertical wall and polycyclic borders, not painful
with no regional lymph glandular enlargement.
The gumma of the mucous membrane
When it ulcerates it may destruct the underlying structures:
1. In the nasal septum it leads to saddle nose.
2. In the soft palate it ends by destruction and perforation
3. In the tongue it may give one of the following pictures:
a. Macroglossia: due to diffuse gummatous infiltration.
b. Superficial glossitis: red smooth glazed area due to
destruction of the tongue papillae.
c. Chronic interstitial glossitis: the tongue may be smaller
than normal.
d. Leucoplakia: irregular white patch induced by chronic
irritation.
Diagnosis of Tertiary stage:
a.Clinically: Any residual stigmata of early syphilis
should be looked for.
b.Serologically: S.T.S. is positive in 90% of cases
(if negative specific tests should be done).
CONGENITAL SYPHILIS
Congenital syphilis is acquired by placental
transmission of infection from the mother.
Congenital syphilis can be prevented by detection
and treatment of infected mothers.
The outcome of prengancy:
During early stages of infection, there are large
numbers of T.pallidum with the following effects:
a. Abortion.
b. Stillbirth.
c. Early neonatal death.
If infection occurs late in pregnancy or is milder; the
following may occur:
a. Premature born child.
b. Some children are born apparently healthy and
signs may be delayed for days, weeks or months.
I. EARLY CONGENITAL
SYPHILIS
In this phase the manifestations, occur in the first
2 years of life.
They are similar to those of secondary stage of
acquired syphilis.
There is no primary stage in congenital syphilis as
the infection is blood-borne.
1. Skin:
a. Bullous eruption mainly on the palms and soles.
b. Rashes like those in the secondary stage of
acquired syphilis.
c. Condylomata lata in the napkin area.
d. Fissuring of the angles of the mouth and wrinkling
of the skin of the face due to weight loss (old man
look).
e. Brownish yellow patches on the skin (café au lait
tint).
2. In the mucous membrane:
(mucous patches)
a. The lips, mouth and throat.
b. The mucoperiosteum of the nasal cavity giving
rise to syphilitic rhinitis.
c. The larynx leading to thin or aphonic cry.
3. Lymphadenitis.
4. Bones:
a. In the first six months : Osteochondritis of the long
bones.
b. After 6 months: Periostitis of the long bones.
c. After one year: Osteoperiostitis of the phalanges
(syphilitic dactylitis).
5. Viscera:
a. Enlarged liver and spleen.
b. Lungs (Pneumonia Alba).
c. Meningitis
Diagnosis of early congenital syphilis:
1- Dark-ground examination.
2- Serological tests.
II. LATE CONGENITAL SYPHILIS
After the first 2 years of life.
1. Interstitial keratitis (the commonest):
Circumcorneal vascularization of the sclera, which
then extends to the deep layers of the cornea.
2. Gummatous osteoperiostitis of the
bones:
Thickening of the middle third of tibia (Sabre
tibia).
Bony swellings of the skull (Parot's nodes).
Destruction of the nasal septum with depression
of the lower part of the nose.
Swelling (not painful) of big joints, especially
the knee joint (Clutton's joint).
3. Auditory nerve affection.
4. Skin and mucous membrane affection: Similar
to those in late acquired state.
5. C.N.S. affection.
III. THE STIGMATA
These include the scars and deformities of
previous syphilitic lesions and remain for life.
1. Stigmata of early congenital syphilis:
a. Saddle nose:
Depression of the bridge of the nose due to decreased
growth of the nasal bones and septum which is the end
result of syphilitic rhinitis.
b. Hutchinson's Teeth:
Small, separated and screw driver like central incisors of
the permanent teeth due to affection of tooth buds late in
pregnancy.
c. Syphilitic Rhagades:
Scars radiating from the angles of the mouth due to papular
eruption with maceration and secondary infection in the
mouth angles.
2. Stigmata of late conegnital syphilis:
a. Sabre tibia:
Due to osteoperiostitis in the tibia with new bone formation.
b. Perforation:
Perforation of nasal septum and soft palate.
c. Ghost vessels:
Network of empty vessels deep in the cornea end result of
interstitital keratitis.
d. Frontal bossing:
Broad frontal region due to periosteal nodes in the frontal
bone.
e. Optic atrophy:
A part of C.N.S. affection.
N.B.: Hutchinson's triad:
Hutchinson's teeth +
Interstitial keratitis +
8th nerve deafness.
Diagnosis of late congenital syphilis:
1. Clinical manifestations
2. S.T.S. are positive in 80-90% of cases and when
negative specific tests should be done.
TREATMENT OF SYPHILIS
Penicillin is the drug of choice as:
1-Procaine penicillin G (2% aluminum monostearate
was added to prolong its action (P.A.M) but this
is historical and not used now)
2-Benzathine penicillin G.
TREATMENT REGIMEN
STAGE OF
SYPHILIS
Benzathine penicillin G
Aqueous procaine penicillin G
Early syphilis
(primary,
secondary,
early latent).
2.4 million Units
IM once.
600.000 units
IM daily
for 15 days
Late latent and
late benign
syphilis
2.4 million units IM once/week for
3 weeks
600.000 units
IM daily
for 15 days
Cardiovascular
syphilis
-
600.000 units
IM daily
for 20 days
Neurosyphilis
-
600.000 units
IM daily
for 20 days
Congenital
syphilis
Not recommended, as it is painful.
450.000 units /kg IM divided on 10 days
COMPLICATIONS OF
TREATMENT
1. Jarisch-Herxheimer reaction (J-H):
Following the first injection of penicillin by 2-12 hours as
the patient may get fever and flushing with influenza like
attack.
The syphilitic lesion becomes inflamed and intensified.
This reaction usually disappears the next day.
The cause of this reaction is unknown but it is said that it
may be a hypersensitivity reaction to the products of the
treponemes destroyed by penicillin i.e it is not a drug
reaction.
It is an all or none type of reaction regardless the type or
dose of penicillin
2. Penicillin hypersensitivity:
a- Anaphylactic shock (immediate).
b- Skin rash (delayed) e.g. urticaria.
If the patient is allergic to penicillin, other drugs should be
used:
a. Tetracyclines:
2 grams daily for 15-20 days.
b. Erythromycin:
2 grams daily for 15-20 days.
c. Cephaloridine.
2 grams daily for 10-15 days.
d.quinolones
3. Therapeutic paradox:
It is defined as worsening of the disease after
antisyphilitic therapy resulting from excessive
scarring produced by too rapid destruction of
treponemes and healing of syphilitic lesions by
fibrosis. This fibrosis leads to distortion of the
surrounding structures. It is most notable in
patients with aortic disease.
THANK YOU