1- Gonorrhea
Causative agent: Neisseria gonorrhea.
Morphology:
- gram-ve kidney-shaped diplococci.
- in pathological specimens, the organism appears
intracellularly in pus cells and extracellularly.
Cultural characters:
- Grows best on enriched media as chocolate agar
and Thayer-Marten agar (chocolate agar
containing antibiotics to suppress normal flora).
- Aerobic and needs 5-10% CO2 for growth at 37ºC
for 24-48 hours.
Gm-stained smear of
pathological discharge
Gm stain from colonies
Gm-ve diplococci
Morphology of
N. gonorrhea
on chocolate agar
Biochemical reactions:
- Oxidase positive.
- Ferment glucose.
- Does not ferment maltose or sucrose (in contrary to
N. meningitidis and N. sicca).
Antigenic structure and virulence factors:
Gonococci are antigenically heterogeneous and
capable of changing their surface structure invitro and
may be invivo to avoid host defense
1- Pili:
Important virulence factor as they mediate
i- attachment to host cells.
ii- resistance to phagocytosis.
iii- Antigenic heterogeneity: According to antigenic variation of
pilus protein (pilin), gonococci are classified to about 100
serotypes.
2- OPa: surface proteins help in the attachment to host cells.
3-Lipoolygosaccharides (LOS) (Endotoxin): Toxicity in
gonococcal infection is largely due to toxic effect of LOS.
4- IgA1 protease: Inactivates secretory IgA.
5- Por proteins: several types, play role in antigenic diversity
Pathogenesis: Invasive organism
- Gonococci attack mucus membranes of the
genitourinary tract, eye (ophthalmia neonatorum),
anorectal area and throat producing acute
suppuration and tissue invasion. This is followed by
chronic inflammation and fibrosis.
- Invasion of blood stream (bacteremia) and
disseminated gonococcal infections (DGI) leads to
skin lesions (hemorrhagic papules and pustules),
tenosynoviitis and suppurative arthritis , usually the
knees, ankles and wrists.
- Gonococcal endocarditis is uncommon but sever.
Occurrence of DGIs depends on:
1- certain strains of gonococci cause DGI more
frequently than others. These strains are
characterized by:
- Resistant to bactericidal action of serum.
- Marked sensitivity to penicillin.
- Need arginin, uracil and hypoxanthin for growth.
2- persons deficient in complement components C6C9 (as woman during menses and pregnancy) are
at risk of DGI.
Gonococcal Pathogenesis:
Clinically:
In females:
- The primary infection is in the endocervix and extends to the
vagina and urethra. There will be a mucopurulent discharge.
- The paraurethral and Bartholin glands are usually involved.
- Infection may extend to salpingitis, fibrosis and obliteration of
the tubes (PID, pelvic inflammatory disease) → infertility
In males:
- Gonorrheal urethritis.
- Acute case is characterized by copious discharge.
- chronic case by morning drops.
- Infection may extend to cause prostatitis and epididymitis.
Lab Diagnosis:
Specimen:
- In females: cervical swab in acute and chronic infection.
- In males: urethral discharge in acute infection and morning
drops in chronic infection.
A- Gram stain.
B- Culture on chocolate agar or modified Thayer- Marten agar.
- Cultured plates are incubated aerobically at 36ºC for 24-48
hours in presence of 5% CO2.
- Suspected colonies are identified by:
1- morphology
2-gram stain
3- oxidase test
4-Sugar fermentation
C- Gonococcal antigens in the specimen can be detected by
ELISA and DNA probe.
Serological diagnosis:
- by detection of specific antibodies to gonococcal pilin and
outer proteins by ELISA.
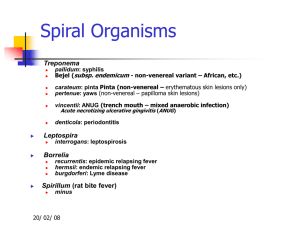
2-Syphilis
Causative organism:
Treponema pallidum which is a spirochete that belongs
to the family treponemataceae, group spirochetes.
Morphology:
- long slender, spiral-shaped bacilli.
- actively motile by axial endoflagellae which lies
between the peptidoglycan layer and an outer
sheath.
- can not be stained with gram stain, but can be
visualized by dark ground microscopy and can be
stained by IFT and Fontana stain.
Morphology of Treponema pallidum
Treponema pallidum smear
Stained by silver impregnation
Technique (Fontana Stain)
Dark-ground microscopy
IF staining
culture:
- It has never been cultured on artificial media or tissue
culture.
- The non-pathogenic treponema (Reiter strain) can be
grown anaerobically in broth enriched with serum.
- The pathogenic Nicola΄s strain can grow in the
testicles of the rabbits.
- In whole blood or plasma stored at 4ºC, the organism
remain viable for at least 24 hours (important in
blood transfusion).
Antigenic structure
- The antigen make up is not exactly known, but
human with syphilis develops:
1- antibodies capable of staining T. pallidum by
indirect IF, immobilizing live motile organism.
2- antibody-like substance, reagin, which gives
positive CF (complement fixation) and flocculation
tests with aqueous suspension of cardiolipin
extracted from normal mammalian heart tissue
Ways of transmission of syphilis
A- Acquired syphilis:
- Is mainly a sexually transmitted disease.
- Can be acquired as a clinical hazard in hands of
doctors and nurses by contact with patients.
- It can be rarely transmitted by blood transfusion of
fresh blood.
B- Congenital syphilis:
- A pregnant woman can transmit the organism to the
fetus through the placenta,
Clinical stages of acquired Syphilis
Primary syphilis:
- Appear 3 weeks after exposure to infection.
Pathogenesis: invasion
- T. pallidum can penetrate intact mucus membrane or
damaged skin or through hair follicles causing the
characteristic lesion of primary syphilis. Then there is a rapid
systemic spread via the blood and lymphatics.
- The lesion begins as a papule which breaks down to form an
ulcer with clean base (chancre).
- The site of the lesion is usually the skin and mm of external
genitalia (vulva and vagina in females, glans penis and penis
in males), but may be intrarectal, perianal or oral.
- Primary lesion usually heals spontaneously.
Secondary syphilis:
Appear 6-10 weeks after appearance of the chancre.
- It is characterized by lesions that follow systemic spread via
the blood and lymphatics :
-
1- fever.
2- maculopapular rash any where in the body, notably in
the palm and sole.
3- moist papule in anogenital region; codyloma lata.
4- mucus patches in the mouth.
- T. pallidum is found in large number in the lesions of primary
and secondary syphilis.
5- During this phase there may be also syphilitic meningitis,
chorioretinitis, nephritis (immune complex type), or periostitis.
maculopapular rash
in the palm
codyloma lata
maculopapular rash
in the body
mucus patches in the mouth
Tertiary syphilis
- About 30% of cases of early syphilis may progress to
complete cure without treatment.
- About 30% of untreated infection remain latent.
- The remainder cases progress to tertiary syphilis.
- Tertiary syphilis is characterized by rare T. pallidum in the
lesions.
Lesions:
1- appearance of granulomatous lesions (gummas) in skin,
bones and liver.
2- degenerative changes in CNS, meningeovascular syphilis,
paresis, tapes dorsalis.
3- cardiovascular lesions aortitis, aortic aneurysm, aortic valve
insufficiency.
Syphilitic gummas in skin
Lab diagnosis of syphilis
I- Detection of T. pallidum in lesions:
Serous exudate from lesions of 1ry and 2ry stages is
examined by:
1- wet film for dark ground microscopy.
2- IFT using fluorescein-labelled antitreponemal antibodies.
3- staining with silver impregnation technique (Fontana stain).
II- Serological diagnosis:
A- non-treponemal antigen tests:
- detect the reagin antibody that react with a non-specific
antigen, cardiolipin, which is an alcohol extract of beef heart
muscle supplemented with lecithin and cholesterol.
- Reagin is a mixture of IgG and IgM that appear 2-3 weeks in
the patient serum and 4-8 weeks in the CSF after exposure
to infection.
Non-treponemal antigen tests include:
1-Flocculation tests: VDRL and RPR (rapid plasma
reagin) tests.
2- CFT, complement fixation test (Wasserman test).
They are characterized by:
- Non-specific and can lead to false positive results.
- Become negative 6-18 months after effective
treatment, so can be used to follow up the effect of
treatment.
- They are mainly used for screening and
epidemiological studies because they are sheep,
rapid and simple.
B- Treponemal antigen tests:
- Highly specific and sensitive tests as they use
T. pallidum as the antigen.
- But they are complex and expensive, so used
mainly for confirmation of diagnosis.
-They remain positive for life, so cannot be used to
judge the efficacy of treatment.
1- Fluorescent treponema antibody test (FTA).
The presence of IgM FTA in the blood of a new-borne
is good evidence of in-utero infection.
2-Treponema pallidum hemagglutination (TPHA).
3- T. pallidum Particle Agglutination Assay (TPPA)
3- Lymphogranuloma venerium
Causative organism:
Chlamydia trachomatis serotypes L1-L3.
Lesion:
- The initial lesion is a painless papule on the external
genitalia, which ulcerates.
- The inguinal L.N. enlarge (pubos), suppurate and the
pus is drained through the overlying skin.
- Healing by scaring leads to strictures and
lymphatic obstruction→ elephantiasis of
labia and scrotum.
Pubos
Chlamydia
- Chlamydia are intracellular parasites that are
considered as gram –v bacteria.
- They lack the mechanism for production of
metabolic energy and can not synthesize ATP →
energy parasite.
- According to outer membrane proteins, chlamydia
are classified into number of serotypes from A-L:- A,B,C cause trachoma.
- D-K cause occulogenital diseases, non-gonococcal
urethritis, cervicitis and PID.
- L1-L3 cause LGV.
Developmental cycle of Chlamydia
There are 2 forms of the organism:
- the elementary body (EB): the infective form. It is
taken by the host cell after attachment by
phagocytosis-like process.
*it enlarges inside the cell forming the reticulate body
(RB).
*RB grows inside the cell and divides by binary fission
forming large number of EBs that are seen as
inclusion bodies.
*EBs are released by a process reversible to
phagocytosis to infect new cells.
Developmental cycle of Chlamydia
Lab Diagnosis
- Smears from the lesion and aspirate from the LN
stained by Giemsa or IF to see the intracytoplasmic
inclusions.
- Direct detection of chlamydial antigens in the
specimen using specific monoclonal antibodies by
ELISA or IFT.
- Direct detection of nucleic acid by PCR and DNA
probes.
- Isolation in tissue culture.
- Serological diagnosis, to detect specific IgM or high
titer of IgG by ELISA or IFT.
4- Non-gonococcal urethritis
Causative agent:
- Chlamydia trachomatis serotypes D-K.
In females → cervicitis, salpingitis and pelvic inflammatory
disease (PID). It can lead to infertility.
In males → urethritis and epididymitis.
- Infection of the new borne during birth causes inclusion
conjunctivitis.
Lab diagnosis: as in case of LGV.
Other causes of non-gonococcal urethritis in males:
1- Mycoplasma (Ureaplasma urealyticum, M. genitalium).
2- Gardnerella vaginalis
3- Trichomonas vaginalis
4- Herpes Simplex virus
5- Chancroid
Causative organism:
Hemophilus ducreyi.
- Gram –v short rods or coccobacilli.
- Facultative anaerobe, grow on chocolate agar,
needs 5% CO2 during incubation at 37ºC.
- Needs X factor (hemin) but not V factor (NAD) for
growth (H. influenza needs both X and V factors).
Chancroid is characterized by soft ulcer on the
external genitalia, regional LN are enlarged and
painful.
Diagnosis:
1- Scraping from the lesion or aspirate from the
enlarged lymph nodes:a- gram stained smear.
b- culture on chocolate agar.
2- Serological diagnosis
6- Mycoplasma hominis
Belong to the family mycoplasmataceae that includes:Genus: Mycoplasma
- Species: M. pneumoniae
- Species: M. hominis
- Species: M. genitalium
Genus: Ureaplasma
- Species: U. urealyticum
In females: M. hominis causes cervicitis, salpingitis, tuboovarian abscess (PID), post partum fever. It may play a role in
bacterial vaginosis.
In males: U. urealyticum, M. genitalium and hominis cause nongonococcal urethritis that may be complicated by epididymitis.
Characters of Mycoplasma
- Smallest free-living bacteria (0.2 - 0.8 :m)
- Facultative anaerobes, except M. pneumoniae →
strict aerobe
- Lack a complete cell wall Thus, they can assume
multiple shapes including round, pear shaped and
even filamentous.
- The only bacteria that contain sterol in the cell
membrane.
- require complex media containing sterols for growth
and for membrane synthesis
- they can not be treated with penicillin or
cephalosporin, Why?
Lab diagnosis:
- Culture of the specimen on specific media→ fried
egg appearance.
- Direct detection of Mycoplasma antigen in the
specimens by IFT and PCR.
- Serological diagnosis: detection of specific IgM or
rising titer of IgG in the patient serum.
7- Granuloma inguinale (granuloma contagiosa)
Donovanosis
- is a chronic, ulcerative, granulomatous disease of the skin
and lymphatics.
Causative agent: Calymmatobacterium granulomatis is a Gram
–ve capsulated rods with characteristic bipolar staining
(Donovan bodies).
- The bacteria invade and multiply in mononuclear cells and
liberated when cells rupture.
CP:
- Initially the lesions are papules, almost always on the
genitalia, that tend to ulcerate slowly.
- Patients develop subcutaneous granulomas in the inguinal
regions; they do not usually involve the lymph nodes, so
called pseudo-buboes.
Diagnosis:
- the nature of the lesion (nodules which erode to
form painless, beefy, granulomatous ulcers).
- The organism is difficult to culture.
- Smear from the lesion stained with Giemsa shows
the enlarged mononuclear cells containing vacuoles
filled with the organism (Donovan bodies).
Candida vulvovaginitis
Mycotic vulvovaginitis
- Candida albicans is found as a part of normal flora in the
vagina in 25% of women.
- Yeast fungus, in pathological specimens pseudohypha are
seen. Strongly gm +ve.
Pathogenesis:
- Factors that are responsible for pathogenicity of the
fungus are: diabetes, pregnancy, immunosuppression,
antibiotics, contraceptive pills, cystic fibrosis and poor
feminine hygiene. There will be excessive growth of the fungus.
- The condition may be complicated by urethritis and dysuria.
Manifestation:
- A thick, curd like white vaginal discharge
- intense pruritis of the vulva
- pH of the discharge is < 4.5
- erythematous vagina and labia
Diagnosis:
1- clinical manifestation.
2- gram stain of vaginal discharge.
3- culture on Sabouraud agar
Gm stain of vaginal discharge in case of mycotic vulvovaginitis
Shows: gm+ve candida yeast and pseudohyphae
Colonies of Candida albicans on
Sabouraud dextrose agar
Candida infection of male genitalia candida balanitis
- Can be recovered from the coronal sulcus in the absence of
clinical infection.
- The strains are usually the same in both partners
- Diabetes plays an important role in the pathogenicity of
candida and candida balanitis may be the representing
symptom.
- Clinically, there is glazed non-purulent surface, slightly
scaling edge. Eroded pustule may occur. Recurrent infection
causes fibrosis and fissuring.
Lab diagnosis:
Gram stain and culture.
Non-specific vaginitis
(bacterial vaginosis)
The commonest cause of vaginal discharge.
- It is due to complex inter-relationship between
Gardenerella vaginalis (small aerobic gm-v bacilli or
coccobacilli) and anaerobic bacteria as Mobiluncus.
- Mycoplasma hominis may play a role.
- The discharge is thin, white-gray, adherent and has
fishy odor.
- Fishy odor is accentuated by addition of 10% KOH.
- pH > 4.5 (5.5)
- Itching is minimal or absent.
- Microscopically→ clue cells, which are epithelial
cells adherent to them the involved organisms.
Clue cells
Clue cell: vaginal epithelium cells adherent to it
Gardenerella vaginalis which are gm-ve
coccobacilli.