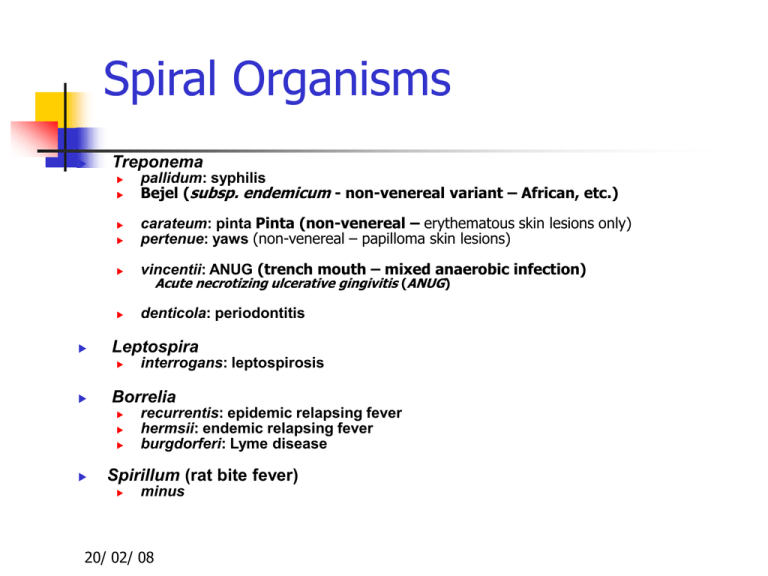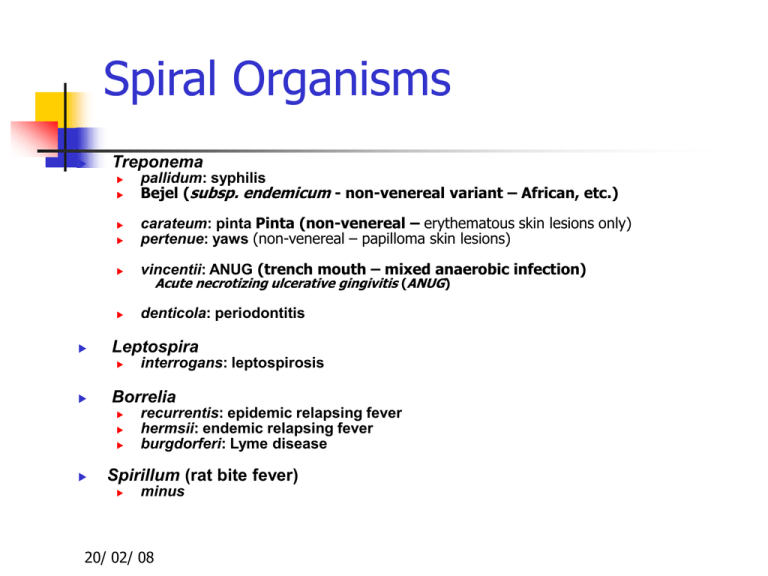
Spiral Organisms
Treponema
carateum: pinta Pinta (non-venereal – erythematous skin lesions only)
pertenue: yaws (non-venereal – papilloma skin lesions)
vincentii: ANUG (trench mouth – mixed anaerobic infection)
denticola: periodontitis
interrogans: leptospirosis
Borrelia
Acute necrotizing ulcerative gingivitis (ANUG)
Leptospira
pallidum: syphilis
Bejel (subsp. endemicum - non-venereal variant – African, etc.)
recurrentis: epidemic relapsing fever
hermsii: endemic relapsing fever
burgdorferi: Lyme disease
Spirillum (rat bite fever)
minus
20/ 02/ 08
SPIROCHETES
20/ 02/ 08
Key Words
Spirochete
Axial filament
Darkfield microscopy
Treponema pallidum
Syphilis
Hard painless chancre
Primary lesion
Secondary Lesion
Tertiary Lesion
Anti-cardiolipin antibodies
20/ 02/ 08
VDRL, RPR, TPHA, FTAABS
Borrelia burgdorferi -
Lyme disease
Relapsing fever (other
borrelia)
Leptospira (leptospirosis)Weil’s Disease
General Characteristics
Elongated, motile (endoflagella- axial filament), spiral
bacteria
Structurally complex – central protoplasmic cylinder
bounded by a cytoplasmic membrane & cell wall of
similar structure to that of Gram –ve bacteria.
20/ 02/ 08
General Characteristics
Larger spirochetes are gram negative, others
are too thin to be seen with light microscope.
Seen under Dark Ground Microscope by
staining with silver
20/ 02/ 08
What are Spirochetes?
Small, motile, slender, helically coiled,
flexible bacteria
Require special staining techniques;
Gram-stain ineffective
20/ 02/ 08
Dark field
Fluorescent
Silver stain for tissue
Wright’s or Giemsa may detect Borrelia in
blood smears
Classification of Spirochetes
Human pathogens belong to following 3
genera:
1.
2.
3.
Treponema
Leptospira
Borrelia
Others (saprophytes) are found in water,
sewage and in mouth & genital tracts of
humans.
20/ 02/ 08
Comparative Morphology
20/ 02/ 08
Treponema
Main treponemes are:
T. pallidum - Syphilis:Venereal (sexual) disease
T. pertenue - Yaws
Non venereal
T. carateum - Pinta
disease
All three species are morphologically identical
20/ 02/ 08
Treponema pallidum
Characteristics :
Discovered by Schaudin & Hoffman in 1905.
Better seen under DGM - prolonged Giemsa
stain, Silver impregnation method
Fontana’s – smears
Levaditi’s – tissue sections
20/ 02/ 08
Characteristics of T.pallidum
Morphology – thin, 10μ with tapering ends
Culture –
1.
2.
3.
20/ 02/ 08
Do not grow on artificial media.
Virulent strains can be maintained in rabbit testis
by serial passages e.g. Nichol’s strain – used for
diagnosis & research
Reiter’s strain – nonpathogenic strain cultivated
for diagnosis.
Characteristics of T.pallidum
Very delicate, easily killed by drying or
heating at 42C for an hr.
Antigenicity – 3 types of Abs are produced.
1.
2.
3.
20/ 02/ 08
Non specific - Reagin Ab
Group specific – found in T.pallidum & Reiter
strains.
Species specific – polysaccharide Ag of T.pallidum
Pathogenicities
Causes Syphilis which can be:
1.
2.
3.
20/ 02/ 08
Venereal
Congenital
Non venereal
Venereal Syphilis
Sexually transmitted disease.
Entry through minute abrasions on mucosa or skin.
Incubation period - about a month (10 to 90 days).
Infectivity is maximum during first 2 years of disease
– primary, secondary & early latent stages
20/ 02/ 08
Stages of venereal syphilis
Primary syphilis –
1.
2.
20/ 02/ 08
hard chancre on genitals: painless, avascular,
circumscribed, indurated & ulcerated lesion;
covered with a thick glairy exudate rich in
spirochetes
Heals spontaneously
in 10-40 days
Primary Lesions
20/ 02/ 08
Stages of venereal syphilis
Secondary syphilis –
1.
2.
3.
4.
Most infectious stage
Sets in 2-6 months after 1 lesion heals.
Pt is asymptomatic but widespread dissemination
occurs via blood
Maculopapular skin rashes on the body, mucous
patches in the oropharyngeal area & condylomata
at mucocutaneous junctions
20/ 02/ 08
Stages of venereal syphilis
Latent syphilis – quiescent stage which
follows secondary stage
Tertiary syphilis – after 10 to 20years,
cardiovascular lesions like aneurysm, aortitis
Late tertiary or quaternary syphilis –
neurosyphilis : tabes dorsalis or general
paralysis of insane
20/ 02/ 08
20/ 02/ 08
Congenital syphilis
Mother to fetus via placenta
After 4th month of gestation
Clinical features – keratitis, saddle shaped
nose, Hutchinsons teeth, 8th nerve deafness.
Non venereal syphilis
In doctors & nurses
Rarely by blood transfusion
20/ 02/ 08
Saddle shaped
nose
Hutchinsons
teeth
20/ 02/ 08
Laboratory Diagnosis
Microscopy –
Dark ground(DGM) - used in 1 & 2 syphilis
Silver staining
Direct fluorescent Ab test (DFA – TP)
1.
2.
3.
Serology – mainstay of diagnosis
1.
2.
3.
20/ 02/ 08
Non specific test/ standard tests for syphilis
Group specific test
Specific tests
Non specific / Standard tests
Test for reagin Ab using cardiolipin Ag.
1.
2.
3.
4.
20/ 02/ 08
Wasserman complement fixation test
Kahn flocculation test
VDRL (Venereal Disease Research Laboratory) test
RPR (Rapid Plasma Reagin) test
Biological false positive reactions are seen
in 1% of human sera
Group specific test
Using Reiter strain Ag – Reiter protein CFT
Specific tests
Using Nichol’s strain
1.
2.
3.
4.
20/ 02/ 08
T. pallidum immobilisation (TPI) test
T. pallidum haemagglutination test (TPHA)
Fluorescent treponemal Ab absorption test (FTAABS) – very specific, standard reference test
T. pallidum enzyme immunoassay(TP-EIA)
Non-treponemal False Positives
(1-2%; generally low titer)
Autoimmune disease
Injection drug use
TB
Vaccinations
Pregnancy
Infectious mononucleosis
HIV
Rickettsial infections
Spirochetal infections other than pallidum
Bacterial endocarditis
20/ 02/ 08
Non-treponemal reactivity diminishes over time
(aside: also after successful treatment)
20/ 02/ 08
Evaluating Serologies
Non-treponemal antibodies develop 4-8 weeks after
infection (within 2 weeks of chancre formation in
70% of patients)
4-fold increase in titer may be seen in early syphilis;
in secondary, titers are often high
Quantitative tests are used to assess treatment; 4fold decreases demonstrate adequate therapy.
Increases after treatment suggest reinfection or
relapse.
Positive CNS reactivity indicates neurosyphilis
Confirm positives with treponemal-specific tests
20/ 02/ 08
Syphilis Serologic Testing
20/ 02/ 08
Treatment
Penicillin is the drug of choice
2nd line- Erythromycin, Tetra/ Doxycycline
Neurosyphilis - Ceftriaxone
20/ 02/ 08
CDC-Recommended Treatments
for Syphilis (2002)
Primary, secondary, or early latent syphilis *
Late latent syphilis, syphilis of unknown duration, tertiary syphilis
Recommended: benzathine penicillin G, 2.4 million units in a single dose, intra
muscularly
Penicillin allergy: doxycycline, 100 mg by mouth twice daily for 14 days
Recommended: benzathine penicillin G, 2.4 million units weekly for 3 weeks,
in tramuscularly
Penicillin allergy: doxycycline, 100 mg by mouth twice daily for 28 days
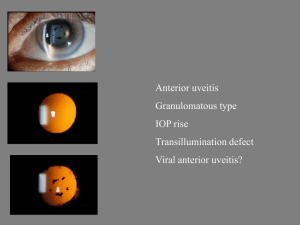
Neurosyphilis, syphilitic eye disease, syphilitic auditory disease
Recommended: Aqueous crystalline penicillin G, 18-24 million units per day
ad ministered as 3-4 million units intravenously every 4 hours or continuous
in fusion for 10-14 days
Alternative: procaine penicillin 2.4 million units intramuscularly once daily
plus probenecid 500 mg by mouth 4 times a day, both for 10-14 days
*Latent syphilis is defined as seroreactivity without other evidence of disease. Early latent syphilis is diagnosed
in patients infected within the preceding year as defined by 1 of the following: (1) a documented
seroconversion; (2) unequivocal symptoms of primary or secondary syphilis; or (3) a sex partner
documented to have primary, secondary, or early latent syphilis. Pregnant women should not be treated
with doxycycline.
Patients with non–life-threatening allergies to penicillin should ideally be desensitized. Patients with serious
allergies to sulfonamides should not be treated with probenecid-containing regimens.
20/ 02/ 08
Prevention and Control
Screening
All pregnant woman at first prenatal visit
Individuals with other STDs
High risk behaviors (drug use, prostitution,
etc.); again at 28 weeks gestation if
pregnant
Exposure
Reporting of contacts and tracing of
sexual partners
Education
20/ 02/ 08