Syphilis - Community HealthCare Association of the Dakotas
advertisement

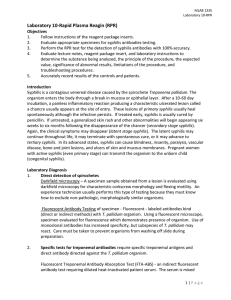
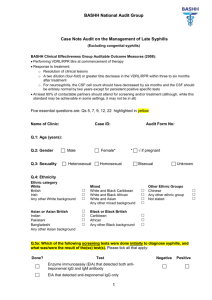
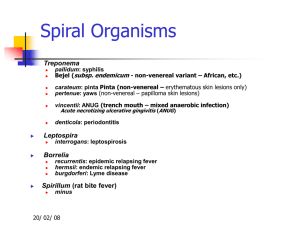
Syphilis: Diagnosis and Treatment Veronica T. Soler MD Infectious Diseases Medical Director& Principal Investigator South Dakota AIDS Education and Training Center Clinical Challenges: Syphilis Most providers have little experience in diagnosing syphilis Even in cities with syphilis outbreaks, most providers see few cases and under-diagnose Syphilis manifestations are protean, and easily misdiagnosed, particularly rashes, spots, lesions, CNS problems, eye disorders A high degree of clinical suspicion is necessary; routinely perform RPR serology's in high risk persons even if they are asymptomatic Clinical Presentation: Clinical Stages of Syphilis • • • • Primary Stage- chancre- ulcerative lesion Secondary Stage- rash Tertiary- cardiovascular or gummatous Congenital Syphilis- oral defects, teeth and bone deformities; saber shins, Hutchinson's incisors • Neuro-syphilis-eye symptoms and central nervous system problems • Latent Syphilis – Early latent < 1 year – Late latent > 1 year Latent Syphilis • A period of time in which there may be no outward signs of infection • Between primary and secondary stage, between secondary relapses, or after secondary stage • Categories: – Early latent: < one year duration – Late latent: > one year duration Diagnosis of Syphilis • Treponema pallidum; has never been cultured. • The organism can be viewed; indirectly via Dark Field Microscopy or directly via Fluorescent Microscopy. • Serological testing is necessary for diagnosis. • Multiple tests are often necessary in sequence. • Services of reference laboratories and clinical experts are often needed. • Both non-treponemal and treponemal serologies are involved and will be discussed. MICROSCOPY • Obtain a specimen by scraping the base of the ulcer/lesion and smearing the material on a microscope slide • Place the slide and view directly under the dark field microscope- not readily available • Apply antibody tagged fluorescent dye to the slide and observe under a fluorescent microscope- also not readily available 80% sensitive; varies with experience/skill of examiner ; decreased sensitivity as the lesion ages Fluorescent Microscope: Demonstration of T. pallidum by using fluorescein-conjugated monoclonal antibodies It is the most specific test for the diagnosis of syphilis when lesions are present. Special microscope, and some specialized laboratory handling is required. Syphilis Serology • Non-treponemal tests: – RPR – VDRL • Treponemal tests: – – – – FTA-ABS TP-PA ELISA/Western Blot Syphilis PCR- able to detect as low as one to 10 organisms per specimen with high specificity ; limited availability and not FDA approved RPR/VDRL • All non-treponemal tests measure both immunoglobulin IgG and IgM anti-phospholipid antibodies formed by the host in response to lipoidal material released by damaged host cells early in infection and lipids from the cell surface of the treponeme itself. • Tests are reported as a qualitative result (RPR) and then as a quantitative titer (VDRL) which falls back to normal with successful cure. • The RPR is reported as a positive or negative result. • The VDRL is quantified and is followed serially from high titer to low or undetectable titer as the infection responds to treatment and resolves (cure). RPR/VDRL Non-treponemal serology • A negative RPR does not exclude the diagnosis of syphilis; only ~75-85% sensitive in primary syphilis but 100% sensitive in secondary disease. • The VDRL is quantified (example 1:32) and used to assess treatment response with four fold drop in titer indicative of treatment success • These tests lack specificity (biologic false positives occur) all reactive tests need to be confirmed by a treponemal test for a definitive syphilis diagnosis Potential Pitfalls of Non-treponemal tests • False positives- the test is measuring something else that reacts with the reagin but is not syphilis.. • False negatives- the test is not always positive in the very earliest phase of infection and sometimes reverts to negative in tertiary disease. Benefits of Non-treponemal Tests • Easy, inexpensive, fast (RPR). • Can be quantified (titer) and degree of antibody levels can be measured (VDRL) • The antibody titer drops with successful treatment and reverts to undetectable with successful treatment. • The titer becomes positive again with reinfection or relapse of the infection. Treponemal Tests Measure specific antibodies to T. pallidum • TP-PA test; The Treponema pallidum particle agglutination (TP-PA)- sensitive in primary syphilis, easy to perform • FTA-ABS: sensitive in primary syphilis, complicated and expensive • Treponemal EIA tests- detect serum antibodies to T. pallidum Treponemal Serology FTA-ABS and others… • Treponemal tests are used mainly as confirmatory tests to verify the reactivity in non-treponemal tests. • However, in populations of low disease prevalence, treponemal tests can be used for screening. • All positive patients would either be treated presumptively because the serious consequences of untreated infection far outweigh the effect of overtreatment, or have a follow-up RPR or VDRL to determine if they have active infection before treatment. • Usually remain positive for life and are not useful to determine re-infection. Diagnostic Flow Chart DO NOT CONFUSE Three IM PNC Preparations • Penicillin G procaine: 600,000 units/mL (1 mL, 2 mL) • Bicillin® C-R; Bicillin® C-R 900/300: Penicillin G benzathine and penicillin G procaine; 1.2 million units/mL (1mL, 2mL) • Bicillin L-A: PNC G Benzathine: 600,000 units/mL (1 mL); 1,200,000 units/2 mL (2 mL); 2,400,000 units/4 mL (4 mL) Prevention “ an once is worth a pound” • Detection of cases; consider it when you have skin sores, oral lesions, rash or any unusual situation: – Syphilis is the greatest mimic of all infectious diseases- “when you do not have a snowballs chance in hell send an RPR/VDRL”. • Low threshold of testing; RPR/VDRL should be part of your STD/HIV bundle especially for pregnant, or at risk individuals. – HIV patients best practice is yearly RPR! – Treat presumptively for primary syphilis when in doubt. • Risk reduction- condoms- remember this important prevention message to all sexually active persons. • Partner notification and empiric treatment of all sexual contacts within 90 days. • Syphilis is a reportable disease in all states. • Syphilis is curable- treatment as prevention! Contact Information: www.aidsetc.org Veronica Soler, MD PI and SD Medical Director DAETC vtsolermd@gmail.com Char Lowman Program Coordinator clowman@usd.edu Rita Shewmake SD Special Projects Coordinator ritashewmake@gmail.com