Neonatal Nursing Care Neonatal Complications
advertisement

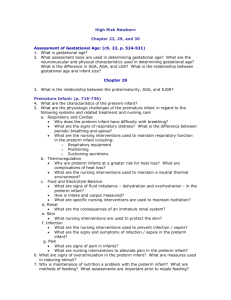
Developed by D. Ann Currie, RN, MSN The Newborn at Risk: Conditions Present at Birth Identification of At-risk Newborn Low socioeconomic level of the mother Limited or no prenatal care Exposure to environmental dangers Preexisting maternal conditions Maternal factors such as age or parity Medical conditions related to pregnancy Pregnancy complications Congenital Anomalies Small-for-gestational-age Maternal factors Maternal disease Environmental factors Placental factors Fetal factors Impact of Maternal Diabetes Mellitus (DM) on the Newborn LGA SGA Hypoglycemia Hypocalcemia Hyperbilirubinemia Birth trauma Polycythemia RDS Congenital malformations Postmaturity Syndrome Hypoglycemia Meconium aspiration and oligohydramnios Polycythemia Congenital anomalies Seizures Cold stress Preterm Infant: Respiratory Alterations Inadequate surfactant production Muscular coat of pulmonary blood vessels is not completely developed Greater risk for the ductus arteriosis to remain open Preterm Infant: Alterations in Thermogenesis Unavailability of glycogen and brown fat Inability to increase oxygen consumption High ratio of body surface area to body weight Extended position increases body surface area Decreased ability to vasoconstrict superficial blood vessels Preterm Infant: GI Alterations Poorly developed gag reflex Incompetent esophageal cardiac sphincter Poor sucking and swallowing reflexes Difficulty meeting caloric needs for growth Inability to handle the increased osmolarity of formula protein Difficulty with absorbing saturated fats Difficulty with lactose digestion Deficiency of calcium and phosphorous Increased basal metabolic rate and increased oxygen requirements Feeding intolerance Potential for the development of necrotizing enterocolitis (NEC Preterm Infant: Kidney Alterations Lower glomerular filtration rate (GFR) Limited ability to concentrate urine or excrete large amounts of fluid Excrete glucose at a lower serum glucose level Buffering capacity is reduced Excretion time of drugs is longer Preterm Infants: Liver Alterations Glycogen stores are used rapidly Glycogen stores are affected by asphyxia and cold stress Low iron stores Conjugation is impaired Preterm Infants: Other Alterations Immunologic Lack of passive IgG antibodies Skin is easily excoriated Neurologic Increased risk for IVH & ICH Delayed or absent reactivity Assessment of the Preterm Newborn Physical characteristics Gestational age Maternal prenatal risk factors Delivery risk factors Physical assessment Family assessment Hydrocephalus: Nursing Assessments Occipital-frontal baseline measurements Daily head circumferences Skin integrity Signs and symptoms of infection Signs of widening of suture lines Hydrocephalus: Nursing Interventions Assist with head ultrasounds and transillumination Change position frequently Clean skin creases Keeping a sheepskin under the head Postoperatively position head off the operative site Choanal Atresia: Nursing Assessment Cyanosis and retractions at rest Nosy respirations Difficulty breathing during feeding Thick mucous Patency of the nares Pass feeding tube to confirm the diagnosis Choanal Atresia: Nursing Interventions Assist with taping the airway in the mouth Elevate the head to improve air exchange Cleft Lip and/or Palate: Nursing Assessment The extent of the cleft Difficulty in sucking Expulsion of formula through the nose Cleft Lip and/or Palate: Nursing Interventions Provide nutrition through feedings with a special nipple Monitor weight gain Clean the cleft with sterile water Supporting parent coping Provide role modeling Position infant prone or side-lying Tracheoesophageal Fistula: Nursing Assessments Excessive oral secretions Constant drooling Abdominal distention Periodic choking and cyanosis Immediate regurgitation of feeding Inability to pass a nasogastric tube Tracheoesophageal Fistula: Nursing Interventions Withholding feedings until esophageal patency is determined Place on low intermittent suction to control saliva and mucus Place in a warmed, humidified incubator Keep infant quiet and elevate head of bed 20-40 degrees Maintain fluid and electrolyte balance Provide parent education and information Diaphragmatic Hernia: Nursing Assessments Barrel chest and scaphoid abdomen Asymmetric chest expansion Absent breath sounds Displacement of heart sounds to the right Spasmodic attacks of cyanosis and difficulty feeding Bowel sounds heard in thoracic cavity Diaphragmatic Hernia: Nursing Interventions Maintenance of adequate respiratory status Gastric decompression Involve parents in care Place infant in high semi-Fowler’s position Turn to affected side to allow unaffected lung expansion Nursing Care of the Drug-Exposed Newborn Neonatal abstinence scoring Monitoring VS and pulse oximetry until stable Small frequent feedings IV therapy if needed Positioning on the right side-lying or semi-Fowler’s Monitoring frequency of diarrhea and vomiting Nursing Care of the Drug-Exposed Newborn Weigh infant every 8 hours during withdrawal Swaddle infant Protect face and extremities from excoriation Place infant in quiet, dimly lighted area of the nursery Administration of medications Infants Born to HIV/AIDS Infected Mothers: Consequences Prematurity SGA Failure to thrive Enlarged spleen and liver Swollen glands Recurrent respiratory infection Rhinorrhea Recurrent GI problems Persistent or recurrent candidiasis Nursing Care of the Infant Born to HIV/AIDS Infected Mothers Provide comfort Keep the newborn well nourished Keep the infant protected from infections Facilitate growth, development, and attachment Congenital Cardiac Disease: Symptoms Cyanosis Heart murmur Signs of congestive heart failure Cardiac Defects Cardiac Defects Cardiac Defects Cardiac Defects Nursing Care of the Newborn with Inborn Errors of Metabolism Assessment of signs of the disorder State-mandated newborn testing Referral of parents to support groups Referral of parents to centers for education Dietary management The End of Part V