Learning Guide
advertisement

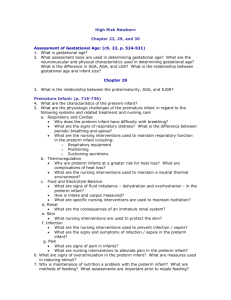
High Risk Newborn Chapter 30 Conditions Present at Birth Identification of High Risk Newborns: 1. How is gestation divided according to the newborn classification and neonatal mortality risk chart? (p. 768-769) Small for Gestational Age / Intrauterine Growth Restriction Newborns: 2. What factors contribute to IUGR/SGA. (p. 771) 3. What are the complications associated IUGR/SGA? (p. 772) 4. What is focus of nursing care for the SGA newborn? (p. 773; see NCP on pages 774-777). Large for Gestational Age Newborns: (p. 773; 777-778) 5. What maternal condition is associated with the development of LGA? 6. What are the complications associated LGA? Infant of Diabetic Mother/ Hypoglycemia: (p. 778; 832-835 ) 7. Infant of a Diabetic Mother: a. What causes the excessive fetal growth? b. What are the complications associated with the IDM? c. Why are infants of diabetic mothers at risk for hypoglycemia? d. What are the clinical manifestations and nursing interventions for an infant with hypoglycemia? Postterm Newborn: (p. 780-781) 8. Define the term "post term infant". 9. What are the physical manifestations of postmaturity? 10. What complications does this condition cause in the neonate? Premature Infant: (p. 782-794) 11. What are the physiologic challenges of the premature infant in regard to the following systems and related treatment and nursing care a. Respiratory and Cardiac What are the nursing interventions used to maintain respiratory function in the preterm infant? What are the signs of respiratory distress? b. Thermoregulation What are the nursing interventions used to maintain thermal neutrality? Why is thermal neutrality a priority goal? c. Gastrointestinal/Nutritional and Hydration” What are specific nursing interventions are used to maintain nutrition and hydration? What are signs of dehydration in the preterm infant and how do they differ from those in a term infant? What assessments should the nurse complete prior to feeding a preterm infant? d. Renal How does renal filtration in the preterm infant affect medication administration? 12. What are the nursing interventions used to prevent infection / sepsis? a. What are the signs and symptoms of infection / sepsis in the preterm infant? 13. What are specific nursing interventions to facilitate and promote parent-infant attachment with the high risk/preterm neonate? a. What are measures to assist the mother of the preterm infant with lactation and breastfeeding? Newborn of Substance Abuse Mother: (p. 794; 797-805) 14. What are the clinical manifestations of an infant suffering from Fetal Alcohol Syndrome? 15. What are the clinical manifestations by systems of an infant undergoing Withdrawal? 16. What nursing interventions would the nurse initiate for the drug-dependent newborn? 17. What are the risks and complications of the infant of a mother who smokes including responses to nicotine and carbon monoxide. Chapter 31 Birth-related Stressors Asphyxia in the Newborn: (p. 814-818) 18. What are risk factors predisposing to asphyxia? 19. What are methods used in resuscitation? 20. What medication is used in resuscitation? Respiratory Distress Syndrome: (p. 818-829) 21. Discuss the pathophysiology involved with RDS. 22. What are the clinical manifestations of RDS? 23. What are major nursing diagnosis and interventions for the newborn with RDS Including: Oxygenation, ventilation Surfactant replacement therapy Heat stabilization Meconium Aspiration Syndrome: (p. 829-831) 24. Explain the cause of meconium aspiration. 25. What precautions do healthcare providers take to prevent the occurrence of meconium aspiration? Care of the Newborn with Jaundice: (p. 835-844; 361-364) Hyperbilirubinemia: 26. Discuss the Pathophysiology of hyperbilirubinemia. 27. Explain the cause of hemolytic disease. a. What additional assessments are necessary for an infant at risk for RH incompatibility? b. What does a positive Coombs test indicate? c. What are the nursing interventions used for an infant receiving phototherapy? d. Why is an exchange transfusion performed? e. What is the indication for, and action of Rh immune globulin (RhoGam or Rhophylac)? (361-364) f. Explain ABO incompatability. g. What complications occur as a result of hemolytic disease? Retinopathy of Prematurity: (1354-1359) 28.What is ROP? 29.What nursing interventions assist with preventing ROP? Necrotizing Enterocolitis: (p. 1595-1597) 30.Explain the cause of NEC. 31.What assessment findings does the nurse monitor to assure early detection of NEC? 32.What is the treatment and nursing care for the newborn with NEC? Care of Newborn with an Infection: (p. 846-850) Infectious diseases- TORCHA: Toxoplasmosis 33.What is the cause of toxoplasmosis? 34.What are the possible results of the infections on the newborn? Other: 35.What are the signs and symptoms of congenital syphilis? 36..What is the treatment for congenital syphilis? 37.How does an infant become infected with Hepatitis B? 38.What is the treatment of an infant whose mother tests positive for Hepatitis B? Rubella: 39.What are the anomalies associated with congenital rubella? 40.At what point is a woman offered MMR immunization if she is rubella nonimmune? Cytomegalovirus: 41.How does a neonate become infected with cytomegalovirus? 42.What are the effects of a cytomegalovirus infection on the newborn? Herpes Simplex Type 2: 43.How is herpes simplex type 2 transmitted to a neonate? 44.What are the effects of a neonatal herpes infection on the newborn? HIV- AIDS: (p. 1284-1295) 45.How is AIDS transmitted to an infant? 46.Explain the laboratory tests used in determining the severity of the disease including: Viral load CD4 count ELISA 47.When is the infant tested? 48.Discuss the nursing interventions for an infant born to an HIV positive mother including: Isolation Medications – protocol for administration