PPH and THIRD STAGE EMERGENCIESfinal
advertisement

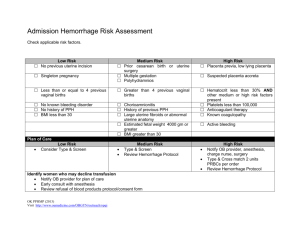
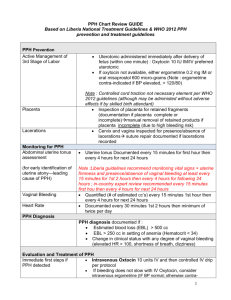
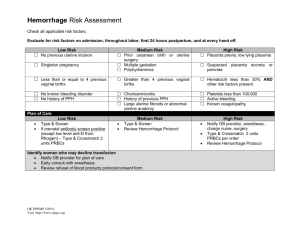
Postpatrum Hemorrhage and Third Stage Emergencies Postpartum Hemorrhage • 3-5% of vaginal deliveries • Definition: >500ml blood loss • Potentially serious complications for mother • Common cause of maternal morbidity and mortality worldwide PPH Risk Factors • • • • • Antepartum Pre-eclampsia Multiparity Multiple gestation Previous postpartum hemorrhage Previous cesarean section • • • • • • Intrapartum Prolonged third stage (>30 mins) Arrest of descent Episiotomy Lacerations: cervical, vaginal, perineal Assisted delivery: forceps, vacuum Augmented labour Causes of PPH: The Four “Ts” • • • • Tone (70%) Trauma (20%) Tissue (10%) Thrombin (1%) PPH: Resuscitative Measures • • • • • • Call for help Airways, Breathing, Circulation Two large-bore IVs Oxygen Stat labs: type & cross, hb, coags Consider transfusion Treatment Approach for PPH • • • • • Catheterise bladder Uterine massage Oxytocics Inspect for lacerations Surgical intervention Tone – Uterine Atony • Most common cause of PPH • Initial step = bimanual uterine massage and compression • Oxytocic agents – Oxytocin – Methylergometrine – Prostaglandins Oxytocin • • • • • Drug of choice 10 – 40 units in 1 litre at 250 cc/hr 1M (10 units) or IV infusion No contraindications Hypotension with IV push Ergot Alkaloide • Ergometrine 0.25 mg • IM only • Contraindicated in hypertension Prostaglandins • 15-methyl prostaglandin F2a – carboprost, Hemabate® • 0.25 mg IM or intramyometrial • Side effects: nausea, diarrhea, flushing, headache • Contraindication: hypersensitivity • Caution: asthma, HTN, cardiopulmonary disease Trauma • Uterine inversion • Uterine rupture • Vaginal or cervical lacerations • Perineal tears • Hematoma Uterine Rupture • Associated with uterine surgery • Suspect if: – – – – vaginal bleeding abdominal tenderness maternal tachycardia signs of shock are out of proportion to viable blood loss Uterine Inversion • Rare, but important to recognize quickly • Suspect if shock disproportionate to blood loss • Replace uterus immediately or after resuscitation • Watch for vasovagal reflex Tissue • Retained placenta – Not delivered within 30 minutes – 3% of deliveries • Retained placental fragments • Invasive placenta Manual Placental Removal • • • • • Cease uterine massage Identify cleavage plane Cup cotyledons in palm Explore uterine cavity Give oxytocin Thrombin - Coagulopathy • Pre-existing conditions – ITP, von Willebrands • Coagulaopthic: Obstetric-related – – – – Hypertension disorders, HELLP Abruption Fetal demise Sepsis • Drugs (e.g. asprin) Coagulation Lab Studies • • • • FBC with platelet count PT-INR, aPPT Fibrinogen level FDP / D-dimer PPH Summary • Unpredictable – be prepared • Uterine atony is the main cause • Remember 4-Ts: Tone, Trauma, Tissue, Thrombin • Consider active management of the third term