the Post Partum Hemorrhage PowerPoint
advertisement
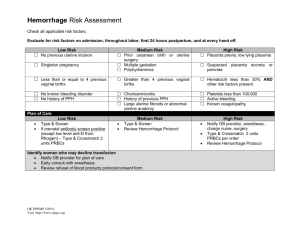
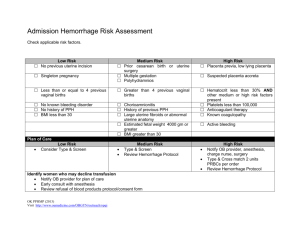
Arnold W. Cohen, MD, Chairman Department of Obstetrics & Gynecology Albert Einstein Medical Center Professor of Ob/Gyn Jefferson Medical College Philadelphia, PA. Old Problem – Consistent Thoughts Definition… Arbitrary and problematic Traditionally: (Baskett, 1999) EBL >=500 cc after vaginal delivery EBL >=1000 cc after a cesarean section Excessive blood loss that makes the patient symptomatic (ie lightheadedness, vertigo, syncope) +/-signs of hypovolemia (ie hypotension, tachycardia, or oliguria) Incidence… Affects 5-15% of women giving birth Two categories: Early (primary) hemorrhage: occurs within the first 24 hours postpartum Late (secondary) hemorrhage: occurs after 24 hours postpartum Be Prepared… Risk Factors: Macrosomia Labor induction and augmentation Prolonged second stage Chorioamnionitis Magnesium sulfate use Previous PPH (Jackson, 2001) Be Prepared… Risk Factor OR CI Retained placenta 3.5 2.1-5.8 Failure to progress during the second stage of labor 3.4 2.4-4.7 Placenta accreta 3.3 2.4 2.3 1.9 1.7-6.4 2.0-2.8 1.6-3.4 1.6-2.4 Induction of labor 1.7 1.4 1.2-2.1 1.1-1.7 Augmentation of labor with oxytocin 1.4 1.2-1.7 Lacerations Instrumental delivery Large for gestational age (LGA) newborn Hypertensive disorders Sheiner et al 2005 Prevention Active management of the 3rd stage of labor uterotonic administration (preferably oxytocin) immediately upon delivery of the baby (or shoulders) early cord clamping and cutting gentle cord traction with uterine countertraction when the uterus is well contracted (ie, Brandt-Andrews maneuver). Benefits of Active Management Vs Physiological management Outcome Ctrl rate RR CI PPH > 500ml 14 % 0.38 0.32-0.46 PPH > 1000ml 2.6% 0.33 0.21-0.51 Hgb < 9 g/dl 6.1% 0.4 0.29-0.55 Blood transfusions 2.3% 0.44 0.22-0.53 Therapeutic Uteretonics 17% 0.2 0.17-0.25 Prendiville, 2000 Etiologies (4T’s)… Tone: uterine atony (80%) Tissue: retained placental tissue Trauma: uterine, cervical or vaginal lacerations Thrombin: dilutional coagulopathy, consumptive coagulopathy and coagulation disorders Clinical findings in Ob PPH… Blood Loss SBP Symptoms and signs Degree of shock 500-1000 mL (10-15%) Normal Palpitations, tachycardia, dizziness Compensated 1000-1500 mL (15-25%) Slight fall (80100 mm Hg) Weakness, tachycardia, sweating Mild 1500-2000 mL (25-35%) Moderate fall Restlessness, (70-80 mm Hg) pallor, oliguria Moderate 2000-3000 mL (35-50%) Marked fall Collapse, air (50-70 mm Hg) hunger, anuria Severe Two important facts… 1. Caregivers consistently underestimate visible blood loss by as much as 50%. The volume of any clotted blood represents half of the blood volume required to form the clots. 2. Most women giving birth are healthy and compensate for blood loss very well. This, combined with the fact that the most common birthing position is some variant of semirecumbent with the legs elevated, means that symptoms of hypovolemia may not develop until a large volume of blood has been lost 25 ml peripad 50 ml peripad 100 ml peripad A saturated 4x4 12-ply sponge = 5 ml Other methods of quantification: •Weight •Direct Measurement 25 ml 100 ml chux 250 ml chux 350 ml chux 500 ml chux 50 ml 75 ml 18x18 laps: 25 ml approx 50%; 50 ml approx 75%; 75 ml entire surface; 100 ml saturated and dripping 100 ml Treatment… Two major components: Resuscitation and management of obstetric hemorrhage and, possibly, hypovolemic shock Identification and management of the underlying cause(s) of the hemorrhage Philadelphia Delivery Centers Organize the team… Call for help ( Attending, nurse , anesthesiologist) Designate a nurse to record vital signs, urine output, fluids and drugs administered Assess the vital signs every 5-10min Resuscitation… Administer 5-7L/min of Oxygen by face mask Place 2 large bore IV lines Initial Blood work: Type and cross match, CBC, PT/PTT/INR, Fib, FSP, Cr, S-8 Fluid Resusciation with NS or LR to maintain BP at 90 mm/Hg Blood transfusion using Massive Transfusion Protocol Correct coagulopathy if present Massive Transfusion Protocol “1:1:1” Consider activation of a MT protocol when patient actively bleeding and any of the following: Systolic blood pressure < 90 mmHg Ph < 7.1 Base deficit > 6 meq/L Temperature below 34°C INR > 2.0 Platelet count < 50,000/mm³ Once activated, the blood bank will send 6 units of PRBC, 6 units of FFP, 6 units of platelets, and 10 units of cryoprecipitate. After this, if the patient remains bleeding (the protocol has not being inactivated), 6 more units of PRBC and FFP will be prepared along with 20 units of cryoprecipitate. The latter product is given in order to elevate the fibrinogen level since the next step of the protocol is to Recombinant Activated factor VII administer. At any point, if the patient’s hemorrhage stops, the blood bank should be notified so that the protocol can be terminated. If bleeding persists, the sequence is started again. Blood Products General considerations Keep the platelet count > 50,000. If less than that, administer 10-12 units initially If surgical intervention is necessary, maintain Plt count > 80-100,000. Cryoprecipate may be used along with FFP for fibrinogen levels <100, give in 6-12 unit doses Blood Component Therapy Product Vol Contents Effect PRBCs 240 RBC, WBC, plasma Increase hematocrit 3 percentage points, hemoglobin by 1 g/dL Platelets 50 Platelets, RBC, WBC, plasma Increase platelet count 5,000– 10,000/mm3 per unit FFP 250 Fibrinogen, antithrombin III, factors V and VIII Increase fibrinogen by 10 mg/dL Cryoprecipitate 40 Fibrinogen, factors VIII and XIII, von Willebrand factor Increase fibrinogen by 10 mg/dL Targets after Transfusion… Fibrinogen > 100mg/dl Hematocrit >21% Hemoglobin >7g/dl Platelet count >50,000 PT/PTT <1.5 times control Response to Resuscitation… Pay attention to pt’s level of consciousness Monitor BP Maintain BP around 90 mm/Hg Systolic Monitor RR Frequent auscultation of lung fields Start Blood if BP cannot be maintained or when Bleeding is controlled Work up… Exam Patient- DR or in OR Uterine Tone Genital Lacerations Placenta Bleeding Sites Lab Studies: Type and cross match, CBC, PT/PTT/INR, Fib, FSP, Cr, S-8 Imaging Studies: bedside U/S Initial Management… Empty bladder Vigorous bimanual Uterine massage Manual exploration of uterine cavity. (Use U/S to r/o retained placenta) Uterontonics Careful inspection of cervix, vagina, vulva and perianal area for lacerations and/or hematomas in OR Consider coagulopathy if no other cause identified Medical Management… UTEROTONICS… Pitocin: 40 units in 1 liter NS or LR IV rapid infusion or 10 units IM (Avoid undiluted IV push) Methergine: 0.2mg IM q2-4hr, max 5 doses (Contraindicated with HTN) Hemabate: 0.25mg IM or intramyometrial q 2090min, max 8 doses (Contraindicated with Asthma) Cytotec: 800-1000mcg PR or SL (not per vagina) Management Monitor CBC, Coagulation studies, ABG Monitor pulse oximetry Monitor Urine output with indwelling catheter Correct coagulopathy FFP- preferred because of volume Cryoprecipitate If PPH hemorrhage continues after uterotonics… Shift to OR Exam under anesthesia: carefully re-inspect the cervix, vagina, vulva and perianal areas for lacerations and /or hematomas Perform D&E to make sure that there is no retained placental tissue (“Banjo” curette) Packing and Tamponade… If PPH still continues…. Packing: 4 inch gauze pack into uterus using a sponge stick. If thrombin available, soak gauze with 5,000 units thrombin in 5cc sterile saline SOS Bakri Tamponade Balloon: Insert balloon, instill 300-500 cc saline Foley catheters: if Bakri balloon unavailable. Insert one or more bulbs, instilled with 60-80cc of NSS SOS BAKRI TAMPONADE BALLOON CATHETER Illustration by Lisa Clark The Simple Solution for Postpartum Hemorrhage Intractable PPH at vaginal delivery Uterine Artery Embolization No coagulopathy Hemodynamically stable to go to Radiology suite Interventional Radiologist available UAE: special considerations… If patient is relatively stable, not coagulopathic and an intervention radiologist is available; consider arterial embolization before proceeding to exploratory laprotomy. Temporizing measures like packing and SOS Bakri balloon tamponade can be used in the meanwhile. Intractable PPH at Vaginal delivery Laparotomy Make midline vertical abdominal incision Begin with bilateral uterine art ligation-Figure of 8’s If unsuccessful, consider… B-Lynch suture or square compression suture Vicryl 1 Hpogastric artery ligation Hysterctomy (supracervical) PPH at cesarean delivery Aggressive resuscitation Direct bimanual compression Direct intramyometrial injection of Hemabate may be undertaken Retained placenta can be removed under direct visualization Compression sutures may be placed LUS can be packed with end in the vagina for 24-30 hrs Hypogastric Artery Ligation Supracervical Hysterectomy Post Op care… Continue resuscitation Monitor vital signs and urine output Monitor vaginal bleeding Repeat labs as indicated Disposition: ?ICU Monitor for coagulopathy Monitor for complications: anemia, ARDS, ATN being most common Documentation… Infusion type and rate Massive Transfusion Protocol (1:1:1) Blood Platelets Fibrinogen Medications administered Patient response Vital signs and urine output Nursing and Physician notes Management of Post Partum Hemorrhage Post Partum Hemorrhage Box Post Partum Hemorrhage Box Post Partum Hemorrhage Meds H.A.E.M.O.S.T.A.S.I.S H A E M O S T A S I S ask for help Assess (VS, EBL) and resuscitate Establish etiology, ensure availability of blood, ecbolics Massage uterus Oxytocin/Methergine/Hemabate/Cytotec Shift to OR Tamponade balloon, uterine packing Apply compression sutures Systematic pelvis devascularization Interventional radiologist – UAE Subtotal/total abdominal Hysterectomy Thank-you from the Chairs of Ob/Gyn in Philadelphia