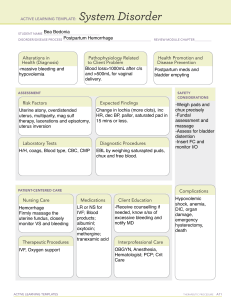
Hemorrhage Risk Assessment
advertisement

Hemorrhage Risk Assessment Check all applicable risk factors. Evaluate for risk factors on admission, throughout labor, first 24 hours postpartum, and at every hand off. Low Risk No previous uterine incision Medium Risk Prior cesarean birth or uterine surgery Multiple gestation Polyhydramnios High Risk Placenta previa, low lying placenta Less than or equal to 4 previous vaginal births Greater than 4 previous vaginal births Hematocrit less than 30% AND other risk factors present No known bleeding disorder No history of PPH Chorioamnionitis History of previous PPH Large uterine fibroids or abnormal uterine anatomy Platelets less than 100,000 Active bleeding Known coagulopathy Singleton pregnancy Suspected percreta placenta accreta Plan of Care Low Risk Type & Screen If prenatal antibody screen positive (except low level anti-D from Rhogam) – Type & Crossmatch 2 units PRBCs Medium Risk Type & Screen Review Hemorrhage Protocol Identify women who may decline transfusion Notify OB provider for plan of care Early consult with anesthesia Review refusal of blood products protocol/consent form OK PPHMP (2015) Visit http://www.opqic.org High Risk Notify OB provider, anesthesia, charge nurse, surgery Type & Crossmatch 2 units PRBCs per order Review Hemorrhage Protocol or Initial Post Delivery Hemorrhage Risk Assessment Check all applicable risk factors. Notify care provider of worsening assessment. More than one medium risk factor moves patient into High Risk category. Evaluate for risk factors on admission, throughout labor, first 24 hours postpartum, and at every hand off. Low Risk Singleton pregnancy No known bleeding disorder No history of PPH Uncomplicated vaginal delivery No genital tract trauma Low Risk Post Delivery Plan of Care Routine recovery Ongoing Quantitative Evaluation of Blood Loss Medium Risk Cesarean birth or uterine surgery Multiple gestation Polyhydramnios Chorioamnionitis History of previous PPH Large uterine fibroids or uterine anomaly Prolonged oxytocin use Rapid labor Application of forceps or vacuum Genital tract trauma Shoulder dystocia Magnesium Sulfate treatment Medium Risk High Risk Hematocrit less than 30% AND other medium or high risk factors present Known coagulopathy Active bleeding Platelets less than 100,000 Routine recovery with heightened awareness for bleeding Ongoing Quantitative Evaluation of Blood Loss Type & Screen Review Hemorrhage Protocol High Risk Post Recovery Plan of Care : First 24 hours If initial post recovery assessment is Low Risk, reassess every 8 hours or more often as condition necessitates. OK PPHMP (2015) Visit http://www.opqic.org Reassess bleeding and fundus every 4 hours or more often as condition necessitates Routine recovery with heightened awareness for bleeding Ongoing Quantitative Evaluation of Blood Loss Notify OB provider, anesthesia, charge nurse, surgery Type & Cross match 2 units PRBCs Review Hemorrhage Protocol Reassess bleeding and fundus every 4 hours or more often as condition necessitates