Spiral-shaped forms of pathogenic bacteria
advertisement

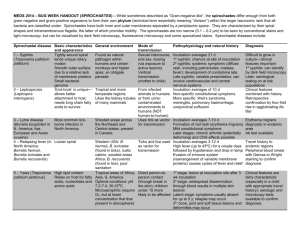
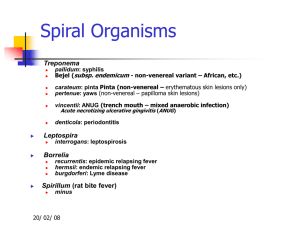
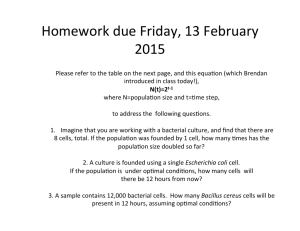
Chair of Microbiology, Virology, and Immunology Spiral-shaped pathogenic bacteria Lecturer Prof. S.I. Klymnyuk Groups of spiral shaped bacteria, which are pathogenic for human Vibrio Campylobacter Helicobacter Spirilla Spirochetes – Treponema – Borrelia – Leptospira Evolution of spiral-shaped bacteria Vibrio, Campylobacter, Helicobacter and Spirilla develop together with Eubacteria. Spirochetes are differed according to their morphological and physiological signs. There is hypothesis about their intermediate evolution position between Protozoa and Bacteria Morphlogy of Campylobacter Morphlogy of Campylobacter S-shaped form S-form Comma-shaped form Spiral-shaped form Campylobacter jejuni 42oC 48h microaerophilic conditions Main biochemical differences between Campylobacter and Helicobacter Species Cata- Н2S Hippurate Oxilase test dase Urease Growth at 42 0С C. jejuni + + + + - + C.coli + + - + - + C. fetus + + - + - - H.pylori + + - + + - Campylobacteriosis in human Diarrhea (enterococlites), sometimes bloodly Endoracditis, pericarditis, meningitis, encephalitis, septicemia Disease of genitourinary tract Pathology of pregnancy (abortion, premature delivery) Autoimmune pathology with alteration of central nervous system Helicobacter pylori History In 1982 following the Easter holidays in the Microbiology Dept of the Royal Perth Hospital a culture of a spiralshaped bacterium from gastric biopsies of patients with gastritis was isolated The discovery was by Dr.Robin Warren and Dr.Barry Marshall Noble Prize inNobel 2005 prize in 2005 •2005 This discovery have revolutionised the diagnosis, treatment and prognosis of upper gastrointestinal disease H. pylori causes gastritis in over half of the world`s population and is the aetiological agent of 95% of duodental ulcers, 70-80% of gastric ulcers and has casual rate in probably up to 60-70% of Gastric Cancer World-wide prevalence of H. pylori H. pylori diseases in human Chronic gastritis Gastric and duodenal ulcer Adenocarcinoma and BLymphoma of stomach Alterations of cardiovascular system? Ulcerated gastric adenocarcinoma Evidances of etiologic role of Helicobacter pylori in pathogenesis of ulcer disease > 95% patients with duodenal ulcer and > 80 % patients with gastric ulcer are infected with H. pylori: this level is more then in healthy persons; In persons, which are infected with H. pylori, duodenal ulcer develops more frequently then in non-infected ones; Antibacterial drugs have medicinal effect and safely prevent ulcer disease relapses Morphology of Helicobacter Helicobacter pylori in mucous membrane of a stomach Helicobacter pylori Peculiarities of Helicobacter pylori Microaerophilic bacterium (5% О2, 5-10 % СО2); They require special nutrient media, a surface of medium must be moist); Selective medium required for isolation-10% sheep blood agar + selective antibiotic supplement They give growth in 48-72 hours, when antibiotics are used – in 13 days; They have high urease, catalase and oxidase activity; They are motile; They are polymorphic bacteria (comma-shaped, spiral-shaped, coccal-shaped forms) Cultivation of Helicobacter pylori Growth of H. pylory Pathogenesis of ulcer disease 1. Infection develops in antral part of stomach 2. Inflammation causes gastritis, duodenitis, but sometimes it is without any symptoms 3. Ulcer is result of inflammation, its complication perforation and hemorrhage Pathogenicity factors of H.pylori Enzymes of virulence: – Urease – Phospholipase А – Proteases Аdhesins Toxins: – Endotoxin – Exotoxin-cytotoxin (factor which is responsible for formation of vacuoles) Bacteriology Catalase: antioxidant and protects from toxic oxygen metabolites from activated neutrophils Protease: further degrade mucus Phospholipase: alter phospholipid content of gastric barrier to change surface tension, hydrophobicity, and permeability Receptor-mediated adhesion: Cag genes encode bacterial membrane proteins Detection of vacuolizing factor in cell culture Positive results Negative results фактору Survival factors of Helicobacter pylori in a stomach Neutralization of acidic contents of the stomach near bacteria (urease, “altruistic autolysis”) Active invasion in mucous layer which covers stomach epithelium (lophotrichates) Ability to adhere to epitheliocytes of stomach (fimbria with hemagglutinin activity) Micro-aerophilism – for survival within the mucous gel Evasion of Immune response Immune Response Recall H Pylori is non-invasive but stimulates hearty inflammatory/immune response Marked increase in platlet activation and aggregation: contribute to microvascular dysfunction and inflammatory cell recruitment Antigenic substances: heat shock protein, urease, lipopolysaccharide (all activate T cells) – Cellular disruption at epithelial tight junctions enhances antigenic presentation Increased IL-1, IL-6, TNF-alpha, and most notably IL-8 – IL-8: chemotactic, activates, recruits neutrophils Immune Response Also stimulates B cell response (IgG and IgA) locally and systemically (role of local antibodies unclear) IgM antibodies: insensitive indicator of acute infection (and not clinically useful) IgA and IgG remain present while infection active and decrease after infection cured Antibodies to CagA protein detectable in gastric tissue and serum (more virulent organism) Reservoir Humans: major reservoir but seen in primates and domestic cats (may transfer to humans!) Sheep: natural host? – H pylori seen in milk and gastric tissue – Higher infection rate in shepherds! Transmission Person to person: isolations of genetically identical strains from multiple family members Fecal/oral: contaminated water in developing countries (h pylori can remain viable in water for several days) Oral/oral: seen in dental plaque but prevalence is low – dentists don’t have higher prevalence Iatrogenic infection: from endoscopes – GI docs/nurses increased risk for H pylori infection! Diagnosis of Helicobacter pylori Bacteriologic Isolation of causative agent Hystologic Examination of causative agent in histological sections and biopsy specimen Urease Examination of biochemical activity in biopsy specimen Respiratory test Examination of of urease activity of causative agent in the stomach with help of C isotopes (13С, 14С) Immunologic ELYSA, examination of bacterial antigens in feces Chain Biopsy specimen polymerase reaction Diagnosis MODALITY ADVANTAGES DISADVANTAGES Endoscopy with Biopsy ( must be performed symtoms of Gastriccarcinoma or > 50Years) Culture Permits inspection of pathology, allows detention of ulcers, neoplasms. Invasive, expensive, time consuming. Permits determination of antimicrobial susceptibilities and pathogenic features of isolates. Not optimally sensitive in most laboratories. Requires several days for results. Generally more sensitive than culture. Allows direct visualisation of organism and extent and nature of tissue involvement. Gastritis may be patchy and biopsy may be performed on wrong area. Insensitivity to detect small numbers of organisms. Requires several days for results. Performed in those Who have failed 2nd Line therapy Histology Diagnosis Urease Detection Rapid, most positives seen within 2 hours Increased sensitivity requires longer incubation. May be false positives with bacterial overgrowth. Serology Not reliable in young children Noninvasive, rapid, quantitative, inexpensive. No determination of lesions or pathology, no antimicrobial susceptibility. Not rapidly responsive to therapy. Urea Breath Tests 90% sensitivity and specificity Relatively non-invasive, relatively rapid, quantitative, rapidly responsive to therapy. Most valuable for assessing response to eradication therapy after 4-8 weeks. Involves expensive instrumentation or administration of radioisotopes. More invasive and less convenient than serology. No determination of lesions or pathology, no antimicrobial susceptibility. Urease test for diagnosis of helicobacteriosis Test-system for diagnosis of helicobacteriosis Standard triple therapy-Eradication therapy, which is probably the most widely used treatment for eradication of H. pylori.-7days mimimal Proton pump inhibitor B.D. (e/g Lansoprazole 30 mg BD) + Clarithromycin 500mg B.D. 1/52 90% plus effective + Amoxycillin 1g B.D. Or If penicillin allergic Proton pump inhibitor B.D. (e/g Lansoprazole 30 mg) Clarithromycin 500mg B.D. Metronidazole 400 mg B.D If treatment failure refer to Gasterenterologist Sodoku (Spirillum minor) Rat-bite fever A febrile, systemic illness usually acquired by direct contact with rats or small rodents Streptobacillus moniliformis Spirillum minor Bites of lab rats are an increasing source of infection Two distinct forms “sodoku” – S. minus Semticemia – S. moniliformis, epidemic arthritic erythema or Haverhill fever Rat-bite fever Clinical manifestations are similar Both produce a systemic illness characterized by fever, rash, and constitutional symptoms Clinical differentiation is possible Semticemia – S. moniliformis, generalized morbilliform eruption to include palms and soles, may become petechial “sodoku” – S. minus, bite site is often inflamed and may become ulcerated Eruption begins with erythematous macules on the abdomen, which enlarge, become purplish red and forming extensive indurated plaques Taxonomy Order: Spirochaetales Family: Spirochaetaceae Genus: Treponema Borrelia Family: Leptospiraceae Genus: Leptospira Main pathogenic bacteria of Spirochetaceae Genus Species Subspecies Treponema T.pallidum T.pallidum T. pallidum T.сarateum T.vincentii Borellia B.recurrentis B.caucasica, B.duttoni, B.persica та ін Epidemic relapcing fever Endemic relapsing fever B.burgdorferi Lyme disease Icterohaemorrhagiae Leptospirosis Leptospira pallidum endemicum Pertenue Disease Syphilis Bejel Yaws Pinta Vincent’s angina General Overview of Spirochaetales Gram-negative spirochetes • Spirochete from Greek for “coiled hair” Extremely thin and can be very long Tightly coiled helical cells with tapered ends Motile by periplasmic flagella (a.k.a., axial fibrils or endoflagella) Outer sheath encloses axial fibrils wrapped around protoplasmic cylinder • Axial fibrils originate from insertion pores at both poles of cell • May overlap at center of cell in Treponema and Borrelia, but not in Leptospira • Differering numbers of endoflagella according to genus & species Spirochetes structure CrossSection of Spirochete with Periplasmic Flagella NOTE: endoflagella, axial fibrils or axial filaments. Spirochetes morphology Treponema Leptospira Borrelia Spirochetes ultrastructure Borrelia Leptospira Classification of Human Treponema Non-pathogenic – T.denticola – T.macrodenticum – T.orale Conditionally pathogenic – T.vincentii Pathogenic – T.pallidum pallidum (syphilis) – T.pallidum endemicum (bejel) – T.pallidum pertenue (yaws) – T.carateum (pinta) The treponemes responsible for these diseases cannot be distinguished serologically, morphologically, or by genome analysis, and they have not been successfully cultivated on artificial media. Vincent’s angina Noma (gangrenous stomatitis) Historical Background Most accepted theory is that Christopher Columbus and his Crew brought back the bacteria which caused the disease Syphilis from the journey to the New World. No distinctive signs of syphilis were found in Europe before he came back. http://www.solarnavigator.net/history/christopher_columbus.htm Background Between 1905 -1910, Schaudinn & Hoffman identified T pallidum as the cause of syphilis The name "syphilis" was coined by Italian physician and poet Girolamo Fracastoro in his Latin written poem “Syphilis sive morbus gallicus” ("Syphilis or The French Disease") in 1530 General Characteristics of Treponema pallidum Too thin to be seen with light microscopy in specimens stained with Gram stain or Giemsa stain • Motile spirochetes can be seen with darkfield micoscopy • Staining with anti-treponemal antibodies labeled with fluorescent dyes Intracellular pathogen Cannot be grown in cell-free cultures in vitro • Koch’s Postulates have not been met Do not survive well outside of host • Care must be taken with clinical specimens for laboratory culture or testing Treponema in tested material Cell attacked by treponema Virulence Factors of T. pallidum Outer membrane proteins promote adherence Hyaluronidase may facilitate perivascular infiltration Antiphagocytic coating of fibronectin Tissue destruction and lesions are primarily result of host’s immune response (immunopathology) Epidemiology of T. pallidum Transmitted from direct sexual contact or from mother to fetus Not highly contagious (~30% chance of acquiring disease after single exposure to infected partner) but transmission rate dependent upon stage of disease Long incubation period during which time host is non-infectious • Useful epidemiologically for contact tracing and administration of preventative therapy Prostitution for drugs or for money to purchase drugs remains central epidemiologic aspect of transmission Pathogenesis of T. pallidum Tissue destruction and lesions are primarily a consequence of patient’s immune response Syphilis is a disease of blood vessels and of the perivascular areas In spite of a vigorous host immune response the organisms are capable of persisting for decades • Infection is neither fully controlled nor eradicated • In early stages, there is an inhibition of cell-mediated immunity • Inhibition of CMI abates in late stages of disease, hence late lesions tend to be localized Pathogenesis of T. pallidum (cont.) Primary Syphilis Primary disease process involves invasion of mucus membranes, rapid multiplication & wide dissemination through perivascular lymphatics and systemic circulation Occurs prior to development of the primary lesion 10-90 days (usually 3-4 weeks) after initial contact the host mounts an inflammatory response at the site of inoculation resulting in the hallmark syphilitic lesion, called the chancre (usually painless) • Chancre changes from hard to ulcerative with profuse shedding of spirochetes • Swelling of capillary walls & regional lymph nodes w/ draining • Primary lesion heals spontaneously by fibrotic walling-off within two months, leading to false sense of relief Hard chancre Primary syphilis lesion, chancre 57 Pathogenesis of T. pallidum (cont.) Secondary Syphilis Secondary disease 2-10 weeks after primary lesion Widely disseminated mucocutaneous rash Secondary lesions of the skin and mucus membranes are highly contagious Generalized immunological response Clinical findings of Syphilis Secondary syphilis Generalized Mucocutaneous Rash Hetchinzone teeth Manifestations of syphilis 60 Pathogenesis of T. pallidum (cont.) Latent Stage Syphilis Following secondary disease, host enters latent period •First 4 years = early latent •Subsequent period = late latent About 40% of late latent patients progress to late tertiary syphilitic disease Pathogenesis of T. pallidum (cont.) Tertiary Syphilis Tertiary syphilis characterized by localized granulomatous dermal lesions (gummas) in which few organisms are present • Granulomas reflect containment by the immunologic reaction of the host to chronic infection Late neurosyphilis develops in about 1/6 untreated cases, usually more than 5 years after initial infection • Central nervous system and spinal cord involvement • Dementia, seizures, wasting, etc. Cardiovascular involvement appears 10-40 years after initial infection with resulting myocardial insufficiency and death Tertiary syphilis Progression of Untreated Syphilis Late benign Gummas in skin and soft tissues Tertiary Stage Pathogenesis of T. pallidum (cont.) Congenital Syphilis Congenital syphilis results from transplacental infection T. pallidum septicemia in the developing fetus and widespread dissemination Abortion, neonatal mortality, and late mental or physical problems resulting from scars from the active disease and progression of the active disease state Congenital syphilis - early evidence of infection - bullae and vesicular rash Multiple, punched out, pale, blistered lesions, with associated desquamation of palms & plantars Intraoral mucous Multiple, punched out, pale, blistered patches & facial skin lesions, with associated desquamation lesions of palms & plantars Late-onset CS Manifestations include neurosyphilis and involvement of teeth, bones, eyes, and 8th cranial nerve E.g.: Frontal bossing, short maxilla, high palatal arch, Hutchinson triad, saddle nose, and perioral fissure (Rhagades = bacterial infection of skin lesions ) 1. 2. 3. Hutchinson triad Deafness (10 – 40 years) Hutchinson’s teeth = centrally notched, widely-spaced peg-shaped upper central incisors Interstitial Keratitis → blindness (5-20 years) Manifestations include neurosyphilis and involvement of teeth, bones, eyes, and 8th cranial nerve E.g.: Frontal bossing, short maxilla, high palatal arch, Hutchinson triad, saddle nose, and perioral fissure (Rhagades = bacterial infection of skin lesions ) Notched incisors known as Hutchinson’s teeth Metaphyseal osteomyelitis Radiolucent distal radius & ulna with cupping distal ulna “Sabre shins” = Osteoperiostitis Tibia Interstitial keratitis Possible Complications Blindness Deafness Facial deformity Neurological problems Microbiologic diagnosis of Syphilis Microscopy (native an fixed material) – Romanovsky-Giemsa stain – Phase contrast – Dark field Chain polymerase reaction Serologic diagnosis – Wassermann’s test (CFT) – Sedimentation reartions (Каhn’s and SachsWitebsky’s tests) – Microreaction of Treponema pallidum immobilization – IFT, ELYSA, IHAT Diagnostic Tests for Syphilis (Original Wasserman Test) NOTE: Treponemal antigen tests indicate experience with a treponemal infection, but cross-react with antigens other than T. pallidum ssp. pallidum. Since pinta and yaws are rare in USA, positive treponemal antigen tests are usually indicative of syphilitic infection. Conditions Associated with False Positive Serological Tests for Syphillis Prevention & Treatment of Syphilis Penicillin remains drug of choice • • • WHO monitors treatment recommendations 7-10 days continuously for early stage At least 21 days continuously beyond the early stage Prevention with barrier methods (e.g., condoms) Refraining from sexual contact with a individual infected with Syphilis will prevent spreading Prophylactic treatment of contacts identified through epidemiological tracing Facts The group with the highest infection rate in 1998 was between the ages of 20 to 39. If you were African-American you were three times greater to be infected with syphilis than the white population. Factors that may increase your risk of being infected are poverty levels, availability of medical treatment, and access to educational opportunities. Tropic trepanematoses: pinta (T.carateum), bejel (T.endemicum), yaws (T.pertenue) Yaws (tropic granuloma) Bejel (endemic syphilis) Treponema pallidum ssp. endemicum Bejel (a.k.a. endemic syphilis) • Initial lesions: nondescript oral lesions • Secondary lesions: oral papules and mucosal patches • Late: gummas (granulomas) of skin, bones & nasopharynx Transmitted person-to-person by contaminated eating utensils Primitive tropical/subtropical areas (Africa, Asia & Australia) Treponema pallidum ssp. pertenue (May also see T. pertenue) Yaws: granulomatous disease • Early: skin lesions (see below) • Late: destructive lesions of skin, lymph nodes & bones Transmitted by direct contact with lesions containing abundant spirochetes Primitive tropical areas (S. America, Central Africa, SE Asia) Papillomatous Lesions of Yaws: painless nodules widely distributed over body with abundant contagious spirochetes. Treponema carateum Pinta: primarily restricted to skin • • • 1-3 week incubation period Initial lesions: small pruritic papules Secondary: enlarged plaques persist for months to years • Late: disseminated, recurrent hypopigmentation or depigmentation of skin lesions; scarring & disfigurement Transmitted by direct contact with skin lesions Primitive tropical areas (Mexico, Central & South America) Hypopigmented Skin Lesions of Pinta: depigmentation is commonly seen as a late sequel with all treponemal diseases Pinta Borrelia morphology Borrelia in blood smear Epidemiology of Borrelia Infections Borrelia recurrentis Pediculus humanus Ornithodoros spp. Borrelia spp. Borrelia burgdorferi Ixodes spp. Epidemiology of Relapsing Fever Associated with poverty, crowding, and warfare Arthropod vectors • Louse-borne borreliosis = Epidemic Relapsing Fever Transmitted person-to-person by human body lice (vectors) from infected human reservoir Infect host only when louse is injured, e.g., during scratching Therefore, a single louse can only infect a single person Lice leave host that develops a fever and seek normal temperature host • Tick-borne borreliosis = Endemic Relapsing Fever Sporadic cases Transmitted by soft body ticks (vectors) from small mammal reservoir Ticks can multiply and infect new human hosts Pathogenesis of Relapsing Fever Relapsing fever (a.k.a., tick fever, borreliosis, famine fever) • Acute infection with 2-14 day (~ 6 day) incubation period • Followed by recurring febrile episodes • Constant spirochaetemia that worsens during febrile stages Epidemic Relapsing Fever = Louse-borne borreliosis • Borrelia recurrentis Endemic Relapsing Fever = Tick-borne borreliosis • Borrelia spp. Clinical Progression of Relapsing Fever Lyme disease Causative agents: Borrelia burgdorferi Borrelia garinii Borrelia afzelii B. burgdorferi Epidemiology of Lyme Borreliosis Lyme disease was recognized as a syndrome in 1975 with outbreak in Lyme, Connecticut Transmitted by hard body tick (Ixodes spp.) vectors • Nymph stage are usually more aggressive feeders • Nymph stage generally too small to discern with unaided eye • For these reasons, nymph stage transmits more pathogens White-footed deer mice and other rodents, deer, domesticated pets and hard-shelled ticks are most common reservoirs Pathogenesis of Lyme Borreliosis Lyme disease characterized by three stages: i. Initially a unique skin lesion (erythema chronicum migrans (ECM)) with general malaise ECM not seen in all infected hosts ECM often described as bullseye rash Lesions periodically reoccur ii. Subsequent stage seen in 5-15% of patients with neurological or cardiac involvement iii. Third stage involves migrating episodes of nondestructive, but painful arthritis Acute illness treated with phenoxymethylpenicillin or tetracycline Erythema chronicum migrans of Lyme Borreliosis Bullseye rash Diagnosis of Lyme Borreliosis Leptospira morphology Obligate aerobes Characteristic hooked ends (like a question mark, thus the species epithet – interrogans Leptospirosis Clinical Syndromes Mild virus-like syndrome (Anicteric leptospirosis) Systemic with aseptic meningitis (Icteric leptospirosis) Overwhelming disease (Weil’s disease) Vascular collapse Thrombocytopenia Hemorrhage Hepatic and renal dysfunction NOTE: Icteric refers to jaundice (yellowing of skin and mucus membranes by deposition of bile) and liver involvement Clinical findings of leptospirosis Clinical Progression of Icteric (Weil’s Disease) and Anicteric Leptospirosis (pigmented part of eye) Epidemiology of Leptospirosis Mainly a zoonotic disease • Transmitted to humans from a variety of wild and domesticated animal hosts • In USA most common reservoirs rodents (rats), dogs, farm animals and wild animals Transmitted through breaks in the skin or intact mucus membranes Indirect contact (soil, water, feed) with infected urine from an animal with leptospiruria Occupational disease of animal handling Pathogenesis of Icteric Leptospirosis Leptospirosis, also called Weil’s disease in humans Direct invasion and replication in tissues Characterized by an acute febrile jaundice & immune complex glomerulonephritis Incubation period usually 10-12 days with flu-like illness usually progressing through two clinical stages: i. Leptospiremia develops rapidly after infection (usually lasts about 7 days) without local lesion ii. Infects the kidneys and organisms are shed in the urine (leptospiruria) with renal failure and death not uncommon Hepatic injury & meningeal irritation is common