Document
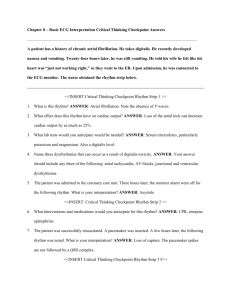
advertisement
Ali Alsayegh, MD, FRCPC,FACC Consultant Cardiologist, Consultant Cardiac Electrophysiologist One AF is relatively common and Challenging Prevalence of Atrial Fibrillation Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults. JAMA. 2001; 285:23702375 Clinical Events (outcomes) affected by AF Two Types of AF Clinical Types Pathophysiological Types AF cause by trigger with normal left atrium (substrate). Possible cure AF without trigger but abnormal substrate. Progressive Three Patient profile very well Common coexistent conditions European Heart Journal. ESC Guidelines EHRA score of AF-related symptoms AF = atrial fibrillation; EHRA = European Heart Rhythm Association CHADS2 score and stroke rate Risk factor-based point-based scoring system - CHA2DS2-VASc The HAS-BLED bleeding risk score Four Treatment Options Rate and rhythm control of AF. Mortality outcome The Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) Investigators Predictor of Mortality In AFFIRM Aliot E , and Ruskin J N Eur Heart J Suppl 2008;10:H32-H54 Five Prevent Stroke Before It Happens Highly preventable (65% RRR) Six Novel New Anticoagulants Approved agents for the prevention of stroke in patients with AF Antiplatelet agents used for stroke prophylaxis in patients with AF Seven Rate Control is not Bad in Many Patients Optimal level of heart rate control Rate control of atrial fibrillation AV node ablation in AF patients aClass of recommendation. bLevel of evidence. AF = atrial fibrillation; AV = atrioventricular; CRT = cardiac resynchronization therapy; LV = left ventricular; LVEF = left ventricular ejection fraction; NYHA = New York Heart Association. Quality of life and symptoms after AV junctional ablation and pacing Wood M et al. Circulation 2000;101:1138-1144 Choice of pacemakers after AV node ablation Eight Rhythm control: Drug Principles of antiarrhythmic drug therapy to maintain sinus rhythm 1. Treatment is motivated by attempts to reduce AF-related symptoms. 2. Efficacy of antiarrhythmic drugs to maintain sinus rhythm is modest. 3. Clinically successful antiarrhythmic drug therapy may reduce rather than eliminate recurrence of AF. 4. If one antiarrhythmic drug ‘fails’ a clinically acceptable response may be achieved with another agent. 5. Drug-induced proarrhythmia or extra-cardiac side-effects are frequent. 6. Safety rather than efficacy considerations should primarily guide the choice of antiarrhythmic agent. Chance of Staying in Sinus Rhythm Choice of antiarrhythmic drug according to underlying pathology Nine Rhythm control: Left Atial Ablation Current approaches to catheter ablation Catheter ablation is currently based on four main strategies: Isolation of the triggers and perpetuating re-entrant circuits located in the pulmonary veins; Disruption of the substrate for perpetuating rotors in the antra of the pulmonary veins; Disruption of putative dominant rotors in the left and right atria, recognized by high-frequency complex fractionated electrograms during mapping of AF. Targeted ablation of ganglionated autonomic plexi in the epicardial fat pads. Pulmonary veins isolation Success Rate of AF Ablation Rhythm control more likely to succeed Recent Onset AF No structural heart disease Small LA Younger Age Reversed precipitating factor Ten Newer Therapeutic options Blood thinner alternative: Left Atrial Occlusion Device Investigational Antiarrhythmic Agents Summary for AF Management from ESC Guidelines Thank You