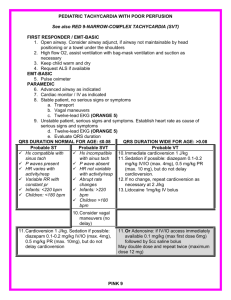
MANAGEMENT OF ATRIAL FIBRILLATION INTRODUCTION • Atrial fibrillation (AF) is the most common sustained dysrhythmias seen in the emergency department (ED). • Because these are age related conditions, the prevalence and frequency of both are increasing. • Worldwide, the literature suggests the same trend; as of 2010, 33.5 million patients, worldwide, had AF. • Emergency clinicians are positioned to not only diagnose but also to help direct follow-up care for patients with AF. INTRODUCTION • Atrial tachyarrthymia characterized by uncoordinated atrial activation with consequent atrial mechanical function. • Presence of irregularly irregular RR intervals and absence of any distinct P wave on ECG • AF leads to predisposition of thrombus formation eventually causing stroke and thromboembolism • Therefore, only antithrombotic therapy can reduce AF related deaths Normal ECG vs AF Pathophysiology • AF is an “irregularly irregular” rhythm that is a manifestation of highfrequency excitation of the atrium, which produces dyssynchronous atrial contractions and irregular ventricular excitation. • The underlying pathophysiology of AF is often a re-entry circuit. • AF can also be caused or maintained by rapid focal ectopic firing. • The location of the ectopic electrical activity or reentry circuits can be the pulmonary veins, right atrium, or left atrium. Risk Factors for Atrial Fibrillation Clinical presentation and AF related outcomes EHRA score Simple clinical tool to assess severity of symptoms during AF Classess explaination Class 1 No symptoms Class II Mild symptoms, normal daily activity not affected Class III Severe symptoms, normal daily activity affected Class IV Disabling symptoms, normal daily activity discontinued Management of AF • Diagnosis of AF • Assessment of duration- Based on types of AF • Assessment for anticoagulation - CHADS2/CHA2DS2VASc • Rate or rhythm control • Treatment of underlying/associated diseases Initial Approach to Management • The goals of treatment for all patients presenting to the ED with AF include achieving hemodynamic stability, controlling symptoms, and preventing complications. • Initial stabilization includes establishing IV access, providing supplemental oxygen as needed to maintain oxygen saturation >92%, and cardiac monitoring. • In the sections that follow, we will discuss rate control, pharmacologic rhythm control, and electrical cardioversion. Emergent Stabilization of Critically Ill Patients • Initial management should focus on obtaining IV access, placing the patient on cardiac monitoring, and quickly assessing the patient’s hemodynamic status. • While Advanced Cardiovascular Life Support (ACLS) focuses on direct current cardioversion for unstable patients in AF who present with hypotension, acute chest pain, acute heart failure, altered mental status, or other features of shock, this recommendation fails to recognize that many patients presenting with AF and one of these features have an underlying medical cause for their rapid rate. Emergent Stabilization of Critically Ill Patients • Therefore, initial evaluation should focus on identifying and then treating an acute medical illness that may be contributing to the patient’s hemodynamic instability. • If the patient remains unstable despite medical resuscitation, and electrical cardioversion is required, the maximum energy setting of the cardiac defibrillator should be used rather than employing an escalating energy approach. ABC Pathway • A: anticoagulation/avoid stroke • B: Better symptoms management • C: Cardiovascular and comorbidity optimization Compared to usual care, implementation of ABC pathway significantly associated with lower risk of AF-related outcomes 1/ A:Anticoagulant/avoid stroke • 1.1 Stroke risk assessment scale 1/ CHADS2 score Risk Factors Score Congestive heart failure 1 HPT 1 Age more than and equal 75 y/o 1 DM 1 Hx of stroke/ TIA 2 Score more than or equal 2: chronic oral anticoagulants eg:vit K antagonist(warfarin) 2/ CHA2-DS2-VASc score - More detailed /comprehensive stroke risk assessment Risk Factors Score Congestive heart failure 1 HPT 1 Age more than and equal to 75 y/o 2 DM 1 Stroke 2 Vascular disease(MI, aortic atherosclerosis) 1 Age 65-74 y/o 1 Sex (Female) 1 3/ ABC Risk score 1.2 Bleeding risk assessment • When initiating antithrombotic therapy, risk of bleeding to be assessed 1.3 Absolute contraindication • Active serious bleeding • Severe thrombocytopenia, plt< 50 • Severe anaemia • Recent high risk bleeding event, ICB 1.4 Medications • Vitamin K antagonist (warfarin) -reduce stroke 64% and mortality 26% • Non vitamin K antagonist(thrombin inhibitors) - dabigatran, apixaban, endoxaban, rivaroxaban - 19% reduction significant stroke/systemic embolism - 51% reduction in hemorrhagic stroke - 10% reduction in mortality Antiplatelet monotherapy was ineffective for stroke prevention in AF Combination of antiplatelet and anticoagulant showed limited evidence for stroke prevention in AF, with no effect on reductions in stroke, myocardial infarction, or death, but with a substantial increase in the risk of major bleeding and ICH 1.5 Surgical interventions • Left atrial appendage occlusion and exclusion 2. Better symptoms control • Target rate control< 110 bpm 2.1 Agents for rate control-used in stable patients - Beta blocker - Verapamil - Digoxin - Combination therapy 2.2 AV node ablation and pacing • Electrical cardioversion should be considered in unstable patients 2.3 Rhythm control Aims to restore sinus rhythm by means of: - Electrical cardioversion - Pharmacological cardioversion: antiarrhythmic medication - AF catheter ablation Together with adequate rate control, anticoagulation therapy and comprehensive cardiovascular prophylactic therapy Cardioversion • Immediate - Acute rythm control in unstable patients - Electrical cardioversion is more effective • Elective - Stable patients DIRECT CURRENT CARDIOVERSION(DCCV) • Effective method of converting AF to sinus rythm • Successful DCCV defined as termination of AF as presence of two or more consecutive P waves after shock delivery • 2 conventional positions are commonly used for electrode placement - Anterolateral - Anteroposterior Several studies shown that anteroposterior placement is more effective Pre treatment with amiodarone , or other anti arrythmic drugs should be considered to facilitate successful cardioversion Complications of DCCV • Thrombo-embolic events • Post cardioversion arrythmias eg: VT or VF, bradycardia • The risks of general anesthesia - Respiratory depression • Local effect eg: skin burns Pharmacological cardioversion-AAD 3/ Cardiovascular and comorbidity optimization • Lifestyle intervention -obesity and weight loss -alcohol and caffeine use -physical activity • Specific CVS risk factors/comorbidities -HPT -HF -DM -Sleep apnea Summary • The goals of initial ED evaluation of patients with AF are stabilizing the patient, assessing underlying causes of AF, and controlling rate and/or rhythm. • Recent literature shows a low incidence of thromboembolic events following ED cardioversion, and it should be considered for patients with symptom onset of <48 hours and in anticoagulated patients. • Patients who are deemed poor cardioversion candidates should undergo rate control using a beta blocker or calcium channel blocker. • The CHA2DS2-VASc score should be calculated for all patientspresenting to the ED in AF, and anticoagulation should be started in those at high risk for thromboembolism. In summary Referrences • CPG AF 2012 • 2020 European Society of Cardiology Guidelines for the diagnosis and management of AF