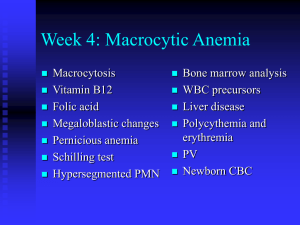
16-Megaloblastic Anemias lecture
advertisement

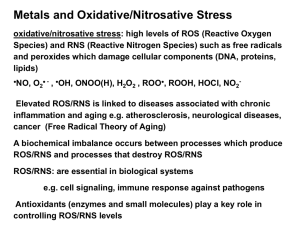
Megaloblastic Anemias Disorders caused by impaired DNA synthesis. Affected cells are mainly those with rapid turnover such as hematopoietic precursors & GIT mucosae. Vitamin B12 def & folic acid def Folic Acid It is pteroylmonoglutamic acid. Synthesized by many plants (fruits & vegetables) & bacteria. Destroyed by excessive cooking. Daily requirement 50 µg ( ↑ by metab demands as preg) Dietary polyglutamate converted into mono & diglutamates then absorbed in jejunum. Folate-binding protein in plasma, milk, & body fluids. Folate body stores = 5-20 mg (1/2 in liver) Function of folate to transfer 1-carbon moiety such as methyl & formyl groups to various organic compounds. They are usually transferred from serine that reacts with tetrahydrofolate to produce glycine & methyl tetrahydrofolate or from formiminoglutamic acid to produce formiminotetrahydrofolate & glutamic acid. This is essential for synthesis of purines, thymidine, & methioninie. Dihydrofolate has to be reduced to tetrahydrofolate by folate reductase. Inhibitors of this enzyme cause folate def such as MTx, pyrimethamine, triamterene, pentamidine, trimethoprim. Cobalamin A complex organometallic vitamin with cobalt atom situated in the middle of a corrin ring. It cannot be synthesized in the human body & must be taken in diet (only animal products) Daily req = 2.5 mg In stomach it is released from diet, then binds R protein (glycoprotein found in saliva, milk, gastric juice & bile). Cobalamin-R in duodenum is digested releasing Cobalamin that binds to intrinsic factor (IF). IF is a 50 kDalton glycoprotein produced by gastric parietal cells (parallel to hydrochloric acid secretion). Cobalamin-IF not digested by proteolytic enzymes reaches terminal ileum where specific receptors for absorption. Within intestinal mucosal cell IF destroyed & Cobalamin transferred to TC-II (B12 binding transfer protein) CBL-TC complex enter circ taken up rapidly by liver, BM & other cells. Liver store = 2 mg. Other stores = 2mg. 3-6 years needed to develop B12 deficiency in malabs Most Cbl in circ bound to TC-I. Methyl-Cbl is required for methionine synthase in conversion of homocysteine to methionine therefore DNA synthesis is impaired. Plasma homocysteine ↑in both folate & vitB12 def Adenosyl Cbl is required for conversion of methylmalonyl CoA to succinyl CoA causing non-physiological fatty acids are synthesized & incorporated in neuronal lipids. Etiology I— Cobalamin deficiency 1- Inadequate intake (Vegetarian) 2-Malabsorption A) Defective release from food Gastric achlorhydria Partial gastrectomy Drugs blocking acid secretion B) Inadequate IF production Pernicious anemia Total gastrectomy Congenital absence or dysfunction of IF C) Terminal ileum disease Tropical & non-tropical sprue Crohn's disease Intestinal resection Neoplasms & granulomatous disease e.g. TB Selective Cbl malabsorption (Immerslund's syndrome) D) Competition for Cbl Fish tapeworm (Diphyllobothrium latum) Bacteria (Blind loop syndrome) 3- Others A) Nitrous oxide B) TC II def C) Congenital enzyme defects II—Folate deficiency 1- Inadequate intake, unbalanced diet, (alcoholics, teenagers & some infants) 2- Increased requirements Pregnancy Infancy Malignancy Increased hematopoiesis (chronic hemolytic anemia) Chronic exfoliative skin disorders Hemodialysis 3- Malabsorption Tropical & non-tropical sprue Drugs (phenytoin, barbiturates & ethanol) 4- Impaired metabolism Dihydrofolate reductase inhibitors (MTx, pyrimethamine, triamterene, pentamidine & trimethoprim) Alcohol Enzyme def (Dihydrofolate reductase & others) III— Other causes 1- Drugs impairing DNA metabolism Purine antagonists (6-MP, azathioprine….etc.) Pyrimidine antagonists (5-FU, cytosine arabinoside …etc) Others (procarbazine, hydroxyurea, acyclovir, zidovudine) 2- Metabolic disorders Hereditary Orotic aciduria Lesch-Nyhan syndrome 3- Megaloblastic anemia of unknown etiology Refractory Megaloblastic anemia Di Guglielmo's syndrome Congenital dyserythropoietic anemia Clinical manifestations B12 def Involve blood, GIT, nervous system Blood --Anemia ---- weakness, palpitation, light headedness, vertigo & tinnitus, angina & CHF Pallor, lemon color complexion of face, mild jaundice, tachycardia, cardiomegaly. GIT --- sore tongue, beefy red tongue, anorexia, wt. loss, diarrhea Neuropsychiatric Fail to remit fully on ttt Start with demyelination later axonal degeneration & later neuronal death Site- peripheral nerves, spinal cord, brain. May precede clinical anemia May be exaggerated or precipitated on folate ttt Numbness, paresthesia, weakness, ataxia, sphincter disturbance, diminished reflexes, +ve Babinski sign, +ve Rombergism, diminished position & vibration sense, amnesia, dementia, irritability, psychosis. Dx Blood film --- Macrocytic normochromic anemia ± pancytopenia (macrocytic hypochromic RBCs seen in Malabsorption syndrome i.e. Dimorphic RBCs) MCV ↑ > 100 fL Retic count low PMN --- nuclear hyper-segmentation (> 6 lobes) BM --- Hypercellular, ↓ M: E ratio, abundant stainable iron, megaloblasts instead of normoblasts with excessive hemoglobinization of cytoplasm yet the nucleus not mature (Nuclear/Cytoplasmic asynchrony), ineffective erythropoiesis S homocysteine level ↑ in both S methylmalonic acid level ↑ in B12 def intramedullary hemolysis (↑UCB, ↑SLDH). S Cbl ↓ ( N= 200-900 pg/mL) , STC-II ↓ S Folic acid ↓ (N = 6-20 ng/mL) RBC folate level is more accurate not affected by diet intake Schilling test Radioactive Cbl given orally, followed shortly by IM inj of unlabelled Cbl. Then 24 h urine collected & radioactivity measured expressed as percentage of ingested radioactivity (↓ in malabsorption) 2nd stage is to give labeled Cbl bound to IF (corrected in PA) 3rd stage antibiotics given (corrected in bacterial overgrowth) Treatment Cbl def ---1- Specific ttt of underlying cause e.g. AB 2- Cbl replacement usually IM 1000 µg / week for 8 weeks, then 1000 µg / month for life. After several days improve wellbeing, retic response start after 4-5 days peaks on day 7 & remission of anemia over next few weeks. Hypokalemia & salt retention, thrombocytosis may be seen 3- Bl T – for hemodynamically unstable patients Folate def ---1- Replacement ttt 1-5 mg/d orally Figure 3. Bone Marrow Aspirate showing megaloblastic erythropoeisis with very fine nuclear chromatin and asynchrony of development of nucleus (immature) and cytoplasm (more mature) Figure 4. Nuclear cytoplasmic asynchrony is evident in these erythroid precursors