Pernicious Anemia
advertisement

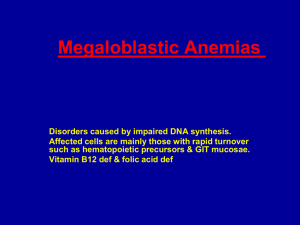
PERNICIOUS ANEMIA Saumil Shah, M.D. July 26, 2005 Description Pernicious anemia (PA) represents a macrocytic anemia resulting from cobalamin (cbl) deficiency. Epidemiology Classically described in persons of Northern European ancestry, but more recent studies indicate its incidence has been previously underestimated in patients of other ancestries, including Latin Americans and African Americans Females slightly more commonly affected than males (female:male ratio is 1.4:1) Average age of onset is 60.5 years, but has been described in all age groups Genetic component postulated – 20% of relatives of patients with pernicious anemia have pernicious anemia Associated with other autoimmune diseases including thyroid disease, type 1 DM, vitiligo, Addison’s disease, myasthenia gravis, and Lambert-Eaton syndrome Normal Cobalamin Absorption Dietary cbl is found only in animal products (meat and dairy products). In the presence of gastric acid and pepsin in the stomach, cbl separates from bound proteins in the stomach and binds to R factors – proteins that are present in saliva and gastric juices Intrinsic factor, a 45 kD glycoprotein, is secreted by gastric parietal cells In the alkaline milieu of the duodenum with the action of pancreatic proteases, cbl is cleaved from the R factors and binds to intrinsic factor The cbl-intrinsic factor complex passes through the gut to the ileum, where it is taken up by ileal mucosal cells via specific intrinsic factor receptors Causes of Cobalamin Deficiency Any disease that interferes with following steps can cause disruption in absorption. Dietary intake Acid-pepsin in the stomach to liberate Cbl from binding to proteins Pancreatic proteases to free Cbl from binding to R factors Secretion of intrinsic factor (IF) by the gastric parietal cells to bind to Cbl An ileum with Cbl-IF receptors Pathophysiology of Pernicious Anemia PA is thought to result from an autoimmune attack on gastric intrinsic factor (IF), this can occur with: Auto-antibodies to the H-K-ATPase on gastric parietal cells may contribute to achlorhydria, parietal cell death, and chronic atrophic gastritis Type I anti-intrinsic factor antibodies block binding of cbl to intrinsic factor Type II anti-intrinsic factor antibodies impede attachment of the cbl-intrinsic factor complex to the terminal ileal mucosal cell receptors Cbl normally facilitates conversion of homocysteine to methionine by transferring a methyl group from methyl-tetrahydrofolate. This reaction results in byproduct of tetrahydrofolate, which is critical to purine synthesis. Cbl deficiency results in decreased tetrahydrofolate and methionine production Impaired DNA synthesis leads to delayed maturation of granulocytic and megakaryocytic cell lines Ineffective erythropoiesis results in intramedullary hemolysis (as well as the classic nuclear-cytoplasmic dissociation seen in the megaloblast) Methionine deficiency may play role in the pathogenesis of the neuropathy, although the mechanism remains unclear Beth Israel Deaconess Medical Center Residents’ Report Cbl also serves as a cofactor in the conversion of methylmalonyl-CoA to succinylCoA; however, the significance of this pathway in the manifestations of cbl deficiency has not been elucidated Clinical Manifestations Cbl stores are large compared to daily intake, thus years of inadequate intake or malabsorption are required before the start of symptoms of cbl deficiency Classic presentation – Prematurely gray, Scandinavian woman who is mentally sluggish; has a shuffling, broad gate; appears lemon-colored (secondary to the paleness of anemia and the icterus of hemolysis); and has a shiny tongue and velvety smooth skin on exam However, most patients will present with the primary symptoms of anemia or neuropathy Anemia 58% Paresthesias 13% GI symptoms 11% (although diarrhea may be present in 50% of patients, and a substantial minority may report paroxysmal abdominal pain, nausea, and vomiting) Weight loss 5% Gait abnormalities 3% Neurologic manifestations do not correlate with the degree of anemia Subacute combined degeneration of dorsal columns and lateral spinal columns is specific for cbl deficiency. It begins with symmetrical paresthesias, loss of positional and vibratory sense, and progressive sensory ataxia (dorsal column manifestations). It can progress to weakness, spasticity, clonus, and even paraplegia (lateral column manifestations). Slowed mentation and dementia are also reported Laboratory Studies CBC with macroovalocytic anemia, leucopenia, and thrombocytopenia Reticulocyte count is usually low or low normal MCV is directly correlated to probability of vitamin deficiency (folate or cbl), with an MCV of >130 reported to be 100% predictive of vitamin deficiency Peripheral blood smear Macroovalocytes and occasional megaloblasts (large, nucleated erythrocyte precursor) Hypersegmented neutrophils – more than 5% of neutrophils with > 5 lobes, or more than 1% of neutrophils with > 6 lobes highly predictive of cbl deficiency Elevated serum bilirubin and LDH evidence intramedullary hemolysis Decreased serum cobalamin – levels less than 200 pg/mL are consistent with cbl deficiency, but higher levels do not exclude the diagnosis Normal serum or RBC folate concentration Metabolite testing: elevated methylmalonic acid and homocysteine are 94% sensitive and 99% specific for the diagnosis of cbl deficiency Anti-intrinsic factor antibodies are highly specific, but are only 50-84% sensitive; antiparietal cell antibodies are less sensitive and specific Schilling test – rarely used due to difficulty in performing the test as well as relatively high false positive and false negative rates Note: Patients may present with only a mild anemia, and macrocytosis can be masked by concurrent iron-deficiency or hemoglobinopathy Treatment Cbl repletion is basis for treatment of pernicious anemia Cbl 1000 ug IM qd x 1 week, then 1000 ug q week x 4 weeks, then 1000 ug q month for life High dose oral cobalamin (1000-2000 ug po qd) appears to be as effective as parenteral therapy, but requires more compliance. It is based on the existence of a second, lower efficiency transport system for cbl that is independent of intrinsic factor or a functional ileum. Reticulocytosis peaks approximately 1 week after initiating replacement therapy. Increases in hemoglobin can be seen within 2 weeks, and hemoglobin levels usually return to normal in 8 weeks. Beth Israel Deaconess Medical Center Residents’ Report