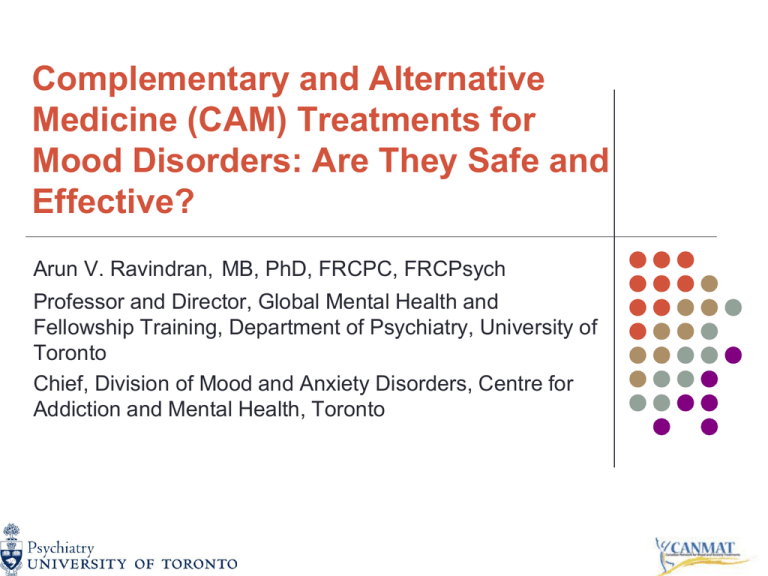
Complementary and Alternative
Medicine (CAM) Treatments for
Mood Disorders: Are They Safe and
Effective?
Arun V. Ravindran, MB, PhD, FRCPC, FRCPsych
Professor and Director, Global Mental Health and
Fellowship Training, Department of Psychiatry, University of
Toronto
Chief, Division of Mood and Anxiety Disorders, Centre for
Addiction and Mental Health, Toronto
Disclaimer
Dr. Ravindran has no conflict of interest to
report. He has no financial interest and has not
received any form of support from any
companies that produce or market any
compound or instrument or procedure
described in this presentation as a main
treatment form.
2
CAM Therapies: Some Notable
Statistics
Over 1/3 of adult population uses some form of CAM
therapies
Visits to CAM practitioners exceed visits to primary
care clinicians
CAM users tend to be female, younger, better
educated and employed
Approximately 2/3 of patients with diagnosed
depression and anxiety use CAM therapies as primary
or adjunct treatments
The perceived helpfulness of CAM therapies is similar
to that of conventional treatments
3
Kessler et al., Am J Psychiatry, 2001
Evaluating CAM Treatments
“Natural is better and safer”
– not necessarily true
Limitations
Quality of evidence:
Few and poorer quality of RCTs
Variation in formulation and quality of agents
Mostly short-term studies
Few studies in severe forms of depression
4
Caveats and Cautions
In general, psychotherapy and pharmacotherapy
should be considered before CAMs
More as adjunctive than as monotherapy
Only guideline and not “standard of care”
Evidence limited to English publications
“Clinical support/use” – utility and practicality
Ravindran et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the
management of major depressive disorder in adults. V. Complementary and alternative medicine
5
treatments. J Affect Disord., 2009
Criteria for Levels of Evidence
Level
Criteria
1
At least 2 RCTs with adequate sample sizes, preferably placebo-controlled, and/or
meta-analysis with narrow confidence intervals
2
At least 1 RCT with adequate sample size and/or meta-analysis with wide
confidence intervals
3
Non-randomized, controlled prospective studies or case series or high-quality
retrospective studies
4
Expert opinion/consensus
Line of Treatment
Criteria
First-Line
Level 1 or Level 2 evidence plus clinical support
Second-Line
Level 3 evidence or higher plus clinical support
Third-Line
Level 4 evidence or higher plus clinical support
Fourth-Line
Level 1 or Level 2 evidence for lack of efficacy, plus clinical support
6
Complementary & Alternative
Therapies
A)Physical Treatments
Light therapy
Sleep deprivation
Exercise
Yoga
Acupuncture
B)Nutraceuticals
Omega-3 fatty acids
DHEA
Tryptophan
SAMe
C)Herbal Remedies
St. John’s Wort
Other herbal remedies
7
What is Light Therapy and How
Effective is It for Mood Disorders?
Exposure to bright light using a device
Seasonal MDD
Non-seasonal MDD
1st line of treatment
As effective as SSRIs
No maintenance/prophylactic studies
Less robust evidence
Combination with SSRIs is more effective
Bipolar Depression
Helps but may trigger mixed state
8
What Efficacy has Sleep
Deprivation shown in MDD?
Total vs. partial treatment options
Difficult to design RCTs – mostly small studies
Comparison with light therapy, exercise and combinations with
antidepressants
Drawbacks
Difficult to sustain treatment
Rebound depression
Tolerance of deprivation effects
Conclusion
Unlikely to be of value in day-to-day practice
Possible use as a 3rd line augmentation in mild to moderate
depression
Co-administration of antidepressants may prolong benefit
9
Is Exercise Beneficial for
MDD?
High vs. low frequency/intensity, aerobic vs. nonaerobic
Recommended – Min. 3x/week, 30 mins+
Recent meta-analyses (2) – better than no
treatment, mixed results against psychological
treatments*
RCTs – exercise + medication superior
to either alone
Some evidence for long-term benefit
and prophylaxis
Recommendation
2nd line augmentation in mild to moderate MDD
Pinquart et al., Aging Ment Health, 2007
10
What is the Neuroscientific Basis
for the Benefit of Exercise?
Increases expression of genes for
neurotropins
Stimulates growth and development of new
cells and increases neuronal plasticity
Increase in monoaminergic
neurotransmission
Possible modulation of interleukin 6.
11
Just standing here doing
nothing for TWENTY
MINUTES! Boy, am I
STRESSED!
YOGA
Class
Hi, everybody. Let’s start destressing by just sitting quietly
doing nothing for twenty minutes.
12
What is Yoga?
An ancient physical art incorporating controlled
breathing, specialized postures and meditation
Yoga forms evaluated in depression:
SKY (emphasis on cyclical hyperventilative breathing)
MDD (2 RCTs, 3 open trials) and dysthymia (3 open
trials)
Iyengar yoga (emphasis on precise postures, use of props)
MDD (1 RCT, 2 open trials)
Hatha yoga (emphasis on individualized practice)
MDD (1 RCT, 1 open trial)
Dysthymia (1 RCT, 1 open trial)
Advantages:
Low cost, non-invasive, self-supervised, highly tolerable
13
What Physiological Mechanisms
Mediate the Beneficial Effects of Yoga?
Reducing sympathetic tone and normalizing
heart rate variability
Normalization of HPA axis dysregulation
Effect on the limbic system
Activation of antagonistic neuromuscular
system
14
Is Yoga Useful for MDD?
Most studies – 4-8 weeks, 4x/week
Difficulty in blinding and placebo control
RCTs
Better than no treatment in MDD
Few comparisons to medication
Yoga as good as TCAs in MDD
Combination superior to medication alone
Useful as monotherapy or augmentation in dysthymia
No published data in bipolar disorder
Recommendation
Use as 2nd line augmentation and for prophylaxis in mild to
moderate depression
15
Efficacy Study of Yoga to Treat
Residual Depressive Symptoms
16-week augmentation pilot study with a
randomized, cross-over design in both unipolar
and bipolar patients
Subjects:
Outpatients currently taking antidepressants
Experiencing significant residual depressive
symptoms
8 weeks of Breathing Focused Yoga + 8 weeks of
psychoeducation, or the inverse
Primary efficacy measure – MADRS
Secondary efficacy measures – CGI, Q-LES-Q
16
Results
MADRS Scores
25
4.5
4
3.5
3
2.5
2
1.5
1
0.5
0
20
*
15
10
5
0
Baseline
Post Yoga
CGI Improvement
Scores
Post
Psychoeducation
QLESQ Scores
60
*
50
*
*
40
30
20
10
0
Baseline
Post Yoga
Post
Psychoeducation
Baseline
Post Yoga
Post
Psychoeducation
*p<0.05
On the MADRS and CGI, patients on yoga showed significant improvement
compared to the psychoeducation group
Both yoga and psychoeducation improved quality of life
17
Efficacy Study of Yoga for
Social Anxiety Disorder
8-week augmentation pilot study with a randomized,
cross-over design in patients with moderatesevere social anxiety disorder
Subjects:
Outpatients, mostly unmedicated
Experiencing significant social anxiety symptoms that
impact functionimg
8 weeks of Breathing Focused Yoga or wait-list
Primary efficacy measure – LSAS
Secondary efficacy measures – CGI, Q-LES-Q
18
Results – need new graphs
Clinical Global Index of
Severity (CGI-S)
LSAS Scores
Quality of Life Scores
(QLESQ)
90
85
7
80
6
75
5
70
*
65
3
55
2
50
Pre
Post
Yoga
Wait List
*
4
60
54
52
50
48
46
44
42
40
1
Pre
Post
Yoga
Wait List
Pre
Post
Yoga
Wait List
*p<0.05
On the LSAS and CGI, patients on yoga showed significant improvement
compared to wait-list
There was no impact on quality of life; however, the patient sample was also
in the severe range
19
20
Assessing the Benefits of
Acupuncture
Acupuncture has proven analgesic and
anaesthetic effects
Benefits mediated by:
The opioid system
Nitric oxide through gracile nucleus/thalamus
Monoaminergic stimulation
Glutamate and GABA
Methodological problems, especially blinding
21
What is the Evidence for
Acupuncture for MDD?
Treatments
MDD
4-8 weeks with 2-16 needles
2 RCTs – as good as antidepressants
No difference compared to sham treatment in 2 studies
Mixed results from other studies
One meta-analysis – benefits but small effect size
Bipolar Depression and Hypomania
Targeted and non-targeted treatment improved symptoms
Overall, safe and well tolerated but current data is inadequate to
make a recommendation (based on English literature only)
22
What are Nutraceuticals?
Non-prescription natural health products, usually
concentrated forms of natural substances
They are often used to support general physical and
mental well-being
Approved by Health Canada: Omega-3 fatty acids,
tryptophan, S-adenosyl-L-methionine (SAM-e), folic acid,
inositol, amino acids, and alpha-lactabumin (as an
ingredient in approved compounds)
Not yet approved in Canada: Dehydroepiandrosterone
(DHEA) and acetyl-L-carnitine are not currently licensed
in Canada.
23
What are Omega-3 Fatty Acids and
What Mediates Their Benefit?
Essential polyunsaturated fatty acids integrated in
multiple biological systems
Thought to improve brain and immune functioning
Mechanism of action still unknown
Focus on eicosapentaenoic acid (EPA) and
docosahexaenoic acid (DHA)
? Improving integrity of neural cell membranes and myelin
Form & Usage
Variable duration of use – 4 to16 weeks
Variable dosing of EPA, DHA or combination (at least 1000
mg)
24
Do Omega-3 Fatty Acids
Alleviate MDD?
Meta-analyses
1 negative, 2 positive for use as monotherapy or
augmentation in mild to moderate MDD
Safe and well tolerated
Diarrhoea, nausea and fishy taste
Watch for bleeding and switch to mania
Conclusion
Likely benefit as 2nd line monotherapy or
augmentation to antidepressants in mild to
moderate depression
25
How Useful Are Omega-3 Fatty
Acids in Bipolar Disorder?
Rates of bipolar disorder correlate inversely with consumption
of fish
As with MDD, EPA is more relevant
Data:
RCTs
Monotherapy (1)
Stoll et al. (+)
Adjunct (2)
Frangou et al. (+)
Keck et al. (-)
Likely more beneficial for bipolar depression than mania.
? Stabilize membrane fluidity
26
EPA for Bipolar Depression
Two parallel studies of efficacy and biology
Efficacy †
Biology ‡
12 week double-blind RCT
(n=51)
Augmentation with
EPA (1-2 gms) or Placebo
MRS before and after 12 weeks
of EPA or Placebo augmentation
(n=18 females)
**EPA superior to Placebo on HAMD and CGI (p=0.04)
† Frangou
et al., Brit J Psychiatry, 2006
‡ Frangou et al., J Psychopharmacol., 2007
**Higher levels of N-acetyl
aspartate (NAA) with EPA vs.
Placebo (p=0.02)
27
How Useful is S-adenosyl-Lmethionine (SAMe) for MDD?
Amino acid functioning as methyl donor
Dose & duration
Systematic reviews (6) – mostly small studies
Oral – 800 mg to 1000 mg (2-8 weeks)
IV/IM – 200 mg to 400 mg (2-8 weeks)
Superior to placebo, equal to TCAs for mild to moderate
depression
Good safety and tolerability
Short-term and monotherapy data only
Recommendation
2nd line monotherapy in mild to moderate depression
28
Does Dehydroepiandrosterone
(DHEA) have Benefits for MDD?
Anti-aging nutritional supplement
? Effect on neurogenesis and neuroprotection
Dose & Duration
30-45 mg/day for 6-8 weeks
Some evidence for benefit as monotherapy as well as
augmentation in major and minor depression, and in medically
ill
Paucity of safety data
Sex hormone effects
Recommendation
3rd line augmentation agent
Short-term use only
29
What is the Evidence for
Tryptophan in MDD?
5-HT precursor
Dose and duration
Most data as adjunctive agent
2-4 g/day, up to 12 weeks
Mostly negative
Some benefit for sleep
Association with E.M.S.? Specific to one manufacturer
Conclusion
Insufficient evidence to support use in MDD
30
Have Other Nutraceuticals been
Evaluated in MDD?
Reasonable evidence:
Preliminary evidence:
Adjunctive folic acid
Acetyl-L-carnitine (monotherapy)
Amino acid mixture (augmentation)
Multivitamins (augmentation)
No evidence:
Alpha Lactalbumin
Inositol
31
32
What is St. John’s Wort? How
Does It Work?
Herb commonly prescribed in Europe for
depression
Mechanism of action unknown
May have serotonergic and dopaminergic effects
No regulation of formulation, though hyperforin is
usually the main ingredient
Dose & duration
Variable formulations (500 mg to 1000 mg)
4-12 weeks
33
What is the Efficacy of St.
John’s Wort in MDD?
Early meta-analyses (2) – superior to placebo in
MDD (but methodological problems)
Recent meta-analyses (5)– equal to
antidepressants, mixed results vs. placebo
Cautions
Psychiatric drug interactions not well studied
Interaction with antibiotics, anti-coagulants, oral
contraceptives, etc.
Reports of induced mania and serotonin syndrome
Recommendation
1st line monotherapy in mild to moderate depression
2nd line augmentation in more severe depression
34
Is St. John’s Wort Useful in
Bipolar Disorder?
No RCTs in bipolar disorder, either as
monotherapy or as adjunct
Many reported cases of SJW-induced
hypomania
Increased risk of switch with advanced age
Inadequate data to make recommendations
35
Free and Easy Wanderer Plus
(FEWP) for Mood Disorders
Chinese herbal mixture for multiple mood and anxiety
symptoms
Acute Treatment as Adjunct †
(Bipolar Depression and Mania)
Maintenance Treatment as Adjunct ‡
(Bipolar Depression and Mania)
12 week double-blind RCT (n=235)
CBZ, CBZ+FEWP, CBZ+Placebo
26 week continuation RCT (n=188)
CBZ+FEWP, CBZ+Placebo
**CBZ superior to Placebo for Depression and
Mania
**CBZ+FEWP superior to CBZ for Depression
**CBZ+FEWP = lower discontinuation rate,
fewer side effects, lower CBZ plasma levels
Acute Treatment as Monotherapy ‡
(Unipolar and Bipolar Depression)
12 weeks double-blind RCT (n=149)
FEWP or Placebo
**FEWP superior to Placebo on HAM-D,
MADRS and CGI for both illnesses
† Zhang
‡
et al. J Psychiatr Res. 2007, 41, 360-369
Zhang et al. J Psychiatr Res. 2007, 41, 828-836
36
What are the Data with Other
Herbal Remedies?
Herbs studied:
Crocus sativus (saffron)
Echium amoenum (borage)
Gingko biloba
Lavandula (lavender)
Rhodiola rosea (roseroot)
Japanese herbal formulations
37
Other Herbal Remedies
(Cont’d)
Few RCTs with small numbers
Variation in formulation, dose, duration
Short-term data only (4-8 weeks)
Recommendation: Crocus sativus for mild to
moderate depression as a 2nd or 3rd line
monotherapy
Insufficient evidence to recommend other herbs
38
Conclusions: CAM Treatments
for Depressive Disorders
Most robust evidence – Light therapy in seasonal
depression.
Evidence and clinical support in mild-moderate MDD
Bipolar disorder
Light therapy – augmentation
Exercise/yoga – augmentation
Omega-3 fatty acids – monotherapy or augmentation
SAM-e – monotherapy
St. John’s Wort – monotherapy
Omega-3 fatty acids - augmentation
Inconclusive evidence at present for other physical, herbal
or nutraceutical therapies
39
40