pharm 25 [3-21
advertisement

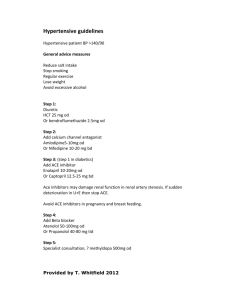
Chapter 25 Learning Objectives 1. What defines stage 1 hypertension? 140-159/X or X/90-99 mm Hg 2. What is the most attractive treatment for pump-based hypertension? β-antagonists, because they treat the high cardiac output and mostly leave vascular resistance alone 3. What drug class treats vascular resistance-based hypertension, even though it’s primary effect is to reduce cardiac preload (not nitro)? When should this drug class be used? Thiazide diuretics Hypothesized to have a vasodilatory effect which compensates for the stimulation of the RAAS that occurs after they decrease intravascular volume First line for hypertension unless there is some other specific indication; start at low dose 4. 5. When are loop diuretics preferable to thiazides? Malignant hypertension and advanced kidney disease with volume-based hypertension When should K+ sparing diuretics be used for HTN? How do drug regimens need to be altered when this class is involved? Only as combination, except for spironolactone which can be used for hyperaldosteronism causing secondary hypertension May need to decrease K+ supplements and ACE inhibitors because of potential for hyperkalemia 6. What two systems do β-antagonists impact? When are they better than [thiazide] diuretics? Heart and RAAS—kidney effects decrease secretion of renin Hypertension plus coronary artery disease (e.g. MIs) or heart failure i. Also good for younger patients? 7. Why aren’t alpha antagonists used much for hypertension? What is their one current indication? α1 antagonists don’t seem to have a good long-term advantage α2 antagonists cause unopposed reflex tachycardia i. pheochromocytoma 8. Even though they aren’t used much anymore except for pheochromocytoma, how do α2 agonists work? What about reserpine and guanethidine? methyldopa, clonidine, and guanabenz act on the medulla sympatholytics (deplete NE from postganglionic sympathetic neurons) bad side effects all, like sexual dysfunction and depression 9. Which are the dihydropyridine agents? Non-dihydropyridines? What drug class and conditions can interact badly with non-dihydropyridines? Nifedipine and amlopdipine Verapamil and diltiazem B-blocker therapy, poor LV function, and poor conduction 10. When is hydralazine used? What adverse effects does it share with the rarely-used minoxidil? Arterial vasodilator; use in conjunction with ACE inhibitors and β-blockers for systolic heart failure Compensatory sodium and water retention, reflex tachycardia 11. When is an ACE inhibitor preferable to [thiazide] diuretics? What are adverse effects? If cough becomes an issue, what can you prescribe instead? Better renal function in patients with chronic kidney disease – especially good for diabetics Few adverse effects, just wath out for intravascular volume depletion or bilateral renal artery stenosis, since this can cause hyperactivation of RAAS ATII receptor antagonists (-sartans) 12. What two drug classes are better for elders? How about blacks? Which classes are worse? Dihydropyridine Ca++ blockers and diuretics i. Also better for blacks β-antagonists are more likely to cause SA or AV nodal dysfunction; theses populations are also less responsive to ACE inhibitors Ischemic Heart Disease 13. What combination with β-blockers can be lethal? When are bad times to administer β-blockers (3)? Verapamil and diltiazem can result in synergistic suppression of the SA node or AV node Decompensated heart failure Bronchospasm In variant/Prinzmetal angina; unopposed alpha vasoconstriction can cause coronary vasospasm 14. What drug class should be used instead to treat variant angina? What drugs from this class are safest to use when LV ejection fraction is reduced? Calcium channel blockers [use an alkaline earth metal to treat Prinz-metal] Amlodipine and felodipine 15. What are nitrates good for besides angina? Acute or chronic LV failure, because they reduce preload 16. Who should get statins? Anybody who has had an MI; LDL goal is 70 mg/dL or less 17. When do you use ranolazine? Refractory angina 18. What three drugs are adminisered at the start of unstable angina treatment? What three drug classes can be added for severe cases or NSTEMI? [NAHB angina with] Aspirin/heparin, β-adrenergic antagonists, and nitrates i. Calcium channel blockers can improve symptoms, but not mortality Eptifibatide and abciximab (GPIIb-IIIa antagonists), clopidogrel and prasugrel (ADP receptor antagonists), and bivalrudin (thrombin inhibitor) [ABCPE] i. The risk of increased bleeding is totally worth it! 19. If we decide to treat STEMI with thrombolytics, what four drugs can we use? Streptokinase activates plasmin Alteplase recombinant t-PA; contraindicated in stroke patients [all the time] tenecteplase genetically engineered t-PA; single dose reteplase genetically engineered t-PA; double doses 30 minutes apart [repeat once] 20. Why would you choose primary percutaneous intervention instead of thrombolytics? What would you use in your drug-eluding stent? What drug should you throw in post MI when you have used percutaneous intervention? It has a better mortality benefit compared to thrombolysis Sirolimus, everolimus, zotarolimus, or paclitaxel (cell cycle stoppers) Afterwards add clopidogrel to the ABCDE regimen (aspirin, beta blockers, x-cholesterol, etc.) Heart Failure 21. What is the most common cause of isolated diastolic HF? Why? Myocardial ischemia ATP is required for both cardiomyocyte contraction and relaxation 22. What is Laplace’s law? Wall stress is proportional to radius and pressure of a chamber, and inversely proportional to wall thickness 23. What drugs can improve congestive symptoms of HF, but do not reduce mortality? Loop diuretics, thiazide diuretics, and vasopressin antagonists 24. What drug actually reduces mortality in HF by reducing preload? Afterload (3)? Spironolactone – recall that systemic edema in HF is caused by RAAS activation and ADH i. Loop diuretics seem to work too, with lesser success Usually paired with ACE inhibitors, angiotensin receptor antagonists*, and β blockers i. beware hyperkalemia from combo and monotherapy 25. How do ACE inhibitors especially benefit HF and CAD patients? [test Q] Alter myocardial remodeling to be more adaptive and less harmful 26. *When do angiotensin receptor antagonists reduce mortality? Only when a patient with severe systolic HF is not also taking ACE inhibitors whatever though, administering both reduces hospitalizations, so why not? 27. Which agent causes a drug-induced lupus syndrome? When does it demonstrate a mortality benefit for HF? Hydralazine, a vasodilator when administered with nitrates; use it when patients can’t take an ACE inhibitor 28. Which drugs must only be used in the short term? Inamrinone and milrinone are PDE inhibitors and “ino-dilators”, that increase mortality if used long-term Dobutamine too