Session 05 (Prehospital Pharmacology)
advertisement
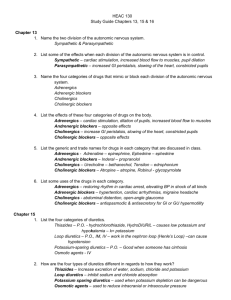
Prehospital Pharmacology Advanced Care Paramedicine Module: 6 Session: 5 Prehospital medicating Prescribed by GP Standing Orders Protocols Transfer orders (should be written) EMS administered Ace Inhibitors Inhibits the effect of the Angiotensin Converting Enzyme (ACE) in the lungs, blocking the conversion of Angiotension I to Angiotension II thus inhibits the release of ADH and helps decrease blood pressure. Captopril Enalapril Quinipril Benazepril Lisinopril Antibiotics Kills or disrupts/stops the growth and development of bacteria Amoxicillin Azithromycin Bactrim Ceclor Ceftin Ciprofloxacin Clarithromycin Cloxicillin Dicloxicillin Erythromycin Keflex Metrodiazanole Nitrofurantoin Penicillin PenVee Rifampin Suprax Tetracycline Vancomycin Vantin Antidysrhythmics Vaughn-Williams Classifications Class I Class II Class III Class IV Antidysrhythmics Class I Na Channel Blockers Slow the maximum rate of Phase 0 depolarization Slow conduction velocity Slow rate and force of contraction refractory period effects Mechanisms of Action Blocks Na influx through fast Na channels Antidysrhythmics Differential effects: Ia Increase duration of AP, prolonged repolarization, prolonged refractory period, decreased membrane responsiveness Decreased depolarization of SA node thus decreased pacemaker activity Also blocks K+ channels Ib Decreased duration of AP, decreased membrane responsiveness in ventricles Blocks activated and inactivated Na+ channels, depresses damaged or depolarized cells (eg. post MI) Does not block K+ channels Ic No effect or minimal increase in duration of AP & repolarization Decreased membrane responsiveness Decreased conduction velocity in atrial & ventricular cells Also blocks K+ channels Antidysrhythmics Class Ia Quinidine Procainamide Disopyramide Class Ib Lidocaine Tocainide (Mexilitine) Phenytoin Class Ic Flecainide Propanfenone Moricizine Antidysrhythmics Class II Beta Blockers Mechanisms of Action Blockade of ß-receptors Inhibition of norepinephrine release (bretylium) Propranolol Metoprolol Atenolol Antidysrhythmics Class III K Channel blockers Prolong action potential and affiliated refractory period Mechanisms of Action Do not alter normal fast Na conductance Do not compete for ß-receptors Bretylium Amiodarone (Has effects of all classes) Sotalol (no longer used – causes Torsades) Antidysrhythmics Class IV Ca Channel Blockers Mechanisms of Action Selectively block slow Ca channels Inhibit slow inward Ca current during phase 2 Decrease rate of phase 4 depolarization Effect on the “pacemaker in charge” Depress conduction velocity in purkinji system and AV node Decrease contractility in myocardium Vasodilatation (lower intracellular Ca in arterial muscle) Verapamil (Isoptin) Diltiazem Cardizem Nifedepine Plendil Antihistamines Compete with histamine for H1 and H2 receptors thus decreasing the histamines affect Chlorpheniramine Cyproheptidine Diphenhydramine Hydroxizine Promethazine Antihypoglycemics Treat diabetes by increasing the amount of sugar in the blood, and decreasing the amount transported into the tissues Diabeta Diabinese Glypizide Glyburide Metformin Tolinase Antifungals Acts primarily by damaging the permeability barrier in the membrane of the fungi. This leads to the inability for the cell to construct an intact membrane and leads to the death of the fungus Diflucan (Fluconazole) Canesten (Clotrimazol) Griseofluvin Ketoconazole Lamisil Nizoral Monostat Sopranox Tinactin Antituberculosis Inhibits RNA synthesis in bacteria Ethambutol Rifampin Isoniazid Pyrazinamide Streptomycin Antivirals Affects the reproduction of the virus. Acyclovir Amatadine Rimantadine 3TC Acyclovir Amatadine AZT DDI Quinivere Rimatadine Zovirax Anxiolytics Combat anxiety by binding with receptors (GABA) in the cerebral cortex and limbic regions. Valium Wellbutrin Xanax Benzodiazepines Bind with receptors (GABA) to decrease anxiety and prevent seizures Valium Versed Halcyon Beta 1 Specific Blockers Compete for the ß-1 receptor sites Blocadren Corgard Lopressor Tenormin Bronchodilators ß-2 agonists Albuterol Aminophylline Atrovent (anti-cholinergic) Metaproterenol Ventolin Cardiac glycosides Block ionic pumps in heart increasing Ca concentrations and contraction, decreasing rate and speed of conduction Digitalis Digitoxin Digoxin Lanoxin Cholesterol lowering Prohibits the synthesis of cholesterol Lopid Lozol Mevacor Zocor Diuretics Causes body’s water balance to shift, excreting water and some electrolytes Loop Diuretics inhibit reabsorption of sodium and chloride in the ascending Loop of Henle, thus excreting water and potassium. Most potent of the diuretics Thiazide Diuretics Affect the distal tubule blocking cotransport of Na-CL HCTZ Potassium-sparing Diuretics Furosemide (Lasix) Amiloride Aldactone Osmotic Diuretics pharmacologically inert nonelectrolyte which is freely filtered by the renal glomerulus and not reabsorbed from the nephron. Osmotically pulls large amounts of water from the cells which it carries with it when it is excreted Mannitol D50 Gastrointestinal Chlopromazine Dimenhydrinate Famotidine Loperamide Magnesium hydroxide Omeprazole Prochloperazine Scopolamine H2 blockers Blocks H2 receptors in the stomach Axid Pepcid Ranitidine Tagamet Cimetidine Migraine therapy Typically decrease the vasodilatation in the cranial vascualture relieving the headache Inderal Ergotamine Fiorinol Sumatripan Narcotics Act on the CNS to slow down all body systems and are used medically as cough suppressants or pain relievers High potential for abuse and for dependency Narcotics can be classified into three groups: Natural origin Codeine, Morphine, Fentanyl Semi-synthetic Heroin Synthetic Merperidine (Demerol), Methadone, Hydromorphone (Dilaudid) Non-Narcotic analgesics Relieve pain without producing unconsciousness or impairing mental capacities. Many of these drugs also have an antipyretic and/or an antiinflammatory effect Aspirin (ASA) Acetaminophen (Tylenol) Analgesic, antipyretic, and anti-inflammatory agent used for mild to moderate pain. It is contraindicated in peptic ulcer disease. It acts as a gastric mucosal irritant and has an anticoagulant effect. Similar to aspirin, but has no anti-inflammatory action. Ibuprofen Ibuprofen is indicated for the relief of mild to moderate pain. Has an anti-inflammatory agent. It is not to be given to patients in the third trimester of pregnancy or anyone with a history of gastrointestinal bleeding NSAIDS Non-Steroidal Anti-inflammatory Drug Inhibits the cyclooxygenase enzyme from synthesizing prostaglandins Alleve ASA Ibuprofen Indomethacin Relafen Toradol Voltaren Steroids Synthetic hormones Possess anti-inflammatory (glucocorticoid) and/or salt-retaining (mineralocorticoid) properties to varying degrees. Glucocorticoids Affect almost all body systems and cause varied metabolic effects Decrease inflammation Stabilization of leukocyte lysosomal membranes Inhibition of macrophage accumulation in inflamed areas Reduction of capillary permeability. Suppress immune responses Promote gluconeogenesis Redistribution of fat from peripheral to central areas of the body Reduce intestinal absorption and increase renal excretion of Ca Reduction of activity and volume of the lymphatic system Decreased immunoglobulin and complement concentrations Decreased passage of immune complexes through basement membranes Mineralocorticoids Affect electrolyte and fluid balance by acting on the distal renal tubule to promote Na reabsorption and K and H excretion. Steroids Glucocorticoids Mineralocorticoids Short Acting Fludrocortisone Cortisone Hydrocortisone Intermediate Acting Methylprednisolone Prednisolone Prednisone Triamcinolone Long Acting Betamethasone Dexamethasone Education Previous Training was “ see this... give this ” Education A&P Pathophysiology Drug specifics Drug specifics Class Mechanism of action Indications Contraindications Precautions Side effects Interactions Dosage Administration