Wellness Premium Credits
advertisement

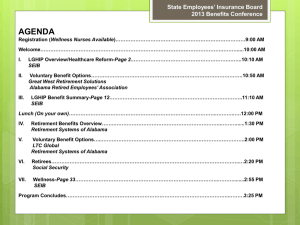
Embracing a Healthy Lifestyle through the State Health Plan New Plan Options and Incentives for 2014 Agenda • Why are we Making Changes for 2014? • New Plan Options for 2014 • Introducing New Wellness Incentives • Open Enrollment for 2014 • Additional Resources 2 Why Are We Making Changes for 2014? • The State Health Plan is providing more choice for members. The Treasurer conducted a listening tour across the state last year and the Plan has conducted various focus groups and surveys and the message has been clear, members have stated that they want more options. • Many of the changes and new choices are designed to encourage members to become more engaged in their health and take steps to live a healthier life. • The Plan also believes an engaged membership will help ensure that the State Health Plan remains financially stable in the years ahead. 3 Health Plan Options for 2014 NEW: Consumer-Directed Health Plan (CDHP) with HRA Enhanced 80/20 Plan • The current Standard 80/20 Plan with a new name to match the new features • A new health plan option • A high-deductible medical plan • • The current Basic 70/30 Plan with a new name A Health Reimbursement Account (HRA) to help offset the deductible • No incentives available • No $0 ACA Preventive Services • No $0 ACA Preventive Medications • $0 ACA Preventive Services • $0 ACA Preventive Medications • 85/15 Coinsurance New Wellness Incentives • $0 ACA Preventive Services • $0 ACA Preventive Medications • CDHP Preventive Medication List ($0 deductible) • New wellness incentives • • Reduced medical copay opportunities Traditional 70/30 Plan • Additional HRA funds for visiting certain providers Open Enrollment will be conducted October 1 – 31, 2013. You must complete enrollment—otherwise, you and your covered family members will be enrolled in the Traditional 70/30 Plan effective January 1, 2014. 4 A New Focus On Wellness Enhanced 80/20 Plan NEW: Consumer-Directed Health Plan (CDHP) with HRA • Wellness premium credits when: • Subscriber completes a Health Assessment • Subscriber attests for him/herself and spouse (if applicable) to not smoking...or to being in a smoking cessation program • Wellness premium credits when: • Subscriber completes a Health Assessment • Subscriber attests for him/herself and spouse (if applicable) to not smoking...or to being in a smoking cessation program • Selecting a Primary Care Provider (PCP) for self and all dependents • Additional wellness incentives • $15 copay reduction for utilizing the PCP (or someone in that practice) listed on the ID card • $10 specialist copay reduction for utilizing a Blue Options Designated Specialist • $0 inpatient hospital copay for utilizing a Blue Options Designated Hospital • Selecting a Primary Care Provider (PCP) for self and dependents • Additional wellness incentives • $15 added to the HRA when the PCP (or someone in that practice) listed on the ID card is seen • $10 added to the HRA when a Blue Options Designated Specialist is seen • $50 added to the HRA when a Blue Options Designated Hospital is utilized for inpatient services 5 Traditional 70/30 Plan • No incentives available • No $0 ACA Preventive Services • No $0 ACA Preventive Medications Wellness Premium Credits Wellness Activity How to Complete It When Members Can Take It Subscriber selects a Primary Care Provider (PCP) Log into the BEACON/eEnroll system to select a PCP. If members have trouble locating a provider, they can contact 888-234-2416. Subscribers don’t have to wait until October to choose a PCP. They can choose one NOW. If they change their mind, they can select a different provider any time. (It takes 5 calendar days to update in the system) Subscriber completes a confidential Health Assessment (HA) Through the State Health Plan website (www.shpnc.org), click on NC HealthSmart and member logs into Personal Health Portal. Health Assessments can also be completed by telephone at 800-817-7044. A new shorter assessment is NOW available on the Personal Health Portal. If the member has completed a Health Assessment since Nov. 1, 2012, through the Personal Health Portal, it will count toward the premium credit. Members may also complete the HA during Open Enrollment via the enrollment portal. Subscriber attests to being a nonsmoker/commits to a cessation program and attests for spouse if applicable Through the online enrollment system. For instructions, go to the State Health Plan website (www.shpnc.org), click on Important Forms under “Quick Links” and select Enroll in a plan. During enrollment, Oct. 1-31, 2013. To quit smoking, the Plan offers assistance through QuitlineNC. Members can access online at www.QuitlineNC.org or call 800-QUITNOW (800-784-8669) A PCP must also be selected for each dependent covered on the State Health Plan. 6 Who can be a Primary Care Provider? • A Primary Care Provider can practice: • General / Family Medicine • Internal Medicine • Pediatrics, or • Obstetrics and Gynecology • A Primary Care Provider can be: • Licensed Nurse Practitioners • Physician’s Assistants Specialty Providers cannot be selected as a PCP. 7 What Is a Blue Options Designated Provider? • Blue Options Designated providers meet BCBSNC criteria for: • Delivering quality health outcomes • Cost effectiveness • Accessibility by members • The Blue Options Designated provider network includes hospitals and certain types of specialists: • General Surgery • Ob-Gyn • Gastroenterology • Orthopedics • Cardiology • Neurology To find a Designated Blue Options provider, members may go online to www.shpnc.org and click on Member Services, then on “Find a Doctor or Facility” or call 888-234-2416 8 The Enhanced 80/20 Plan • An enhanced version of the current Standard 80/20 Plan, except • New name – The Enhanced 80/20 Plan • New incentives to encourage members to manage their health and lower their health care costs • Preventive Care – There will be no copays on Affordable Care Act (ACA ) preventive services or preventive medications. • Primary Care Provider (PCP) – To receive a $15 PCP copay reduction, a PCP must be selected by Oct. 31, 2013. • If the selected PCP is not available at the time of the appointment, the member may visit any provider in the same practice and still receive the copay reduction • If a member wants to change PCPs, they can go to their enrollment portal and select a new PCP. A new ID card with the PCP’s information will be mailed to the member. The PCP change must be made before visiting the new PCP. • Providers* - When a specialist or hospital is needed, members have the option to select a Blue Options Designated Provider: • Specialists – To receive a $10 Specialist copay reduction, choose a Blue Options Designated provider • Hospitals – To avoid a $233 Inpatient Hospital copay, select a Blue Options Designated Hospital *Members may visit any provider in the BCBSNC Blue Options network and be considered “in-network”. The additional rewards are tied to the incentives outlined above and throughout this presentation. 9 Lower Your Premiums with Wellness Premium Credits— The Enhanced 80/20 Plan Complete up to Three Wellness Activities By October 31, 2013 Enhanced Plan Premium Credits Subscriber attests to being a nonsmoker/commits to a cessation program and attests for spouse if applicable $20 per month Subscriber (only) completes a confidential Health Assessment (HA) $15 per month Subscriber and any covered dependents selects a Primary Care Provider $15 per month Reduce your premium by up to… $50 per month 10 Lower Your Health Care Costs with Wellness Incentives— The Enhanced 80/20 Plan Things you can do to reduce your costs… Enhanced Plan Incentives Visit the PCP listed on ID card Your copay is reduced by $15 Visit a Blue Options Designated specialist Your copay is reduced by $10 Get inpatient care in a Blue Options Designated hospital Your $233 copay is not applied Remember: Get preventive services through an innetwork provider in a non-hospital setting 100% coverage – this is provided at no cost to you ACA preventive medication list 100% coverage – this is provided at no cost to you 11 ACA Preventive Medications Drug or Drug Category Criteria Aspirin (to prevent cardiovascular events)-Generic OTC 81mg and 325mg Men ages 45 to 79 years and women ages 55 to 79 years Fluoride – Generic OTC and prescription products Children older than 6 months of age through 5 years old Folic Acid – Generic OTC and prescription products 0.4 – 0.8 mg Iron Supplements – Generic OTC and prescriptions products Women through age 50 years Children ages 6 to 12 months who are at risk for iron deficiency anemia Smoking Cessation – Generic OTC patches and gum Members must contact QuitlineNC for OTC product coverage Vitamin D – Generic OTC and prescription products Men and Women ages ≥ 65 who are at increased risk for falls Women’s Preventive Services & contraception coverage 1) Barrier contraception- i.e. caps, diaphragms 2) Generic hormonal contraception 3) Emergency contraception 4) Implantable medications 5) Intrauterine contraception Women through age 50 You must have a Prescription for these medication to have them covered at 100% 12 Enhanced 80/20 Plan Highlights in 2014 Coverage Annual Deductible In-Network Out-of-Network $700 individual/$2,100 family $1,400 individual/$4,200 family Coinsurance (after deductible is met) 20% of eligible expenses 40% of eligible expenses plus 100% of amount above the Plan’s allowed amount Coinsurance Maximum (excludes deductible) $3,210 individual/$9,630 family $6,420 individual/$19,260 family $30 copay for primary doctor; $15 copay if the PCP on the ID card is utilized Office Visits Inpatient Hospital Prescription Drugs (for 30-day supply) $70 copay for specialists; $60 copay if a Blue Options Designated specialist is utilized $233 copay, then 20% after deductible; copay not applied if a Blue Options Designated hospital is utilized Tier 1 $12 copay Tier 2 $40 copay Tier 3 $64 copay Specialty medications 25% up to $100 maximum per 30-day supply $0 for ACA Preventive Medications 13 40% after deductible $233 copay, then 40% after deductible Tier 1 $12 copay Tier 2 $40 copay Tier 3 $64 copay Specialty medications 25% up to $100 maximum per 30-day supply $0 for ACA Preventive Medications The Consumer-Directed Health Plan (CDHP) with HRA A different kind of health plan with two components High-Deductible Health Plan Health Reimbursement Account (HRA) • Covers the same services as other Plan options through the same PPO network • The Plan funds the members’ Health Reimbursement Accounts (HRA) annually • The deductible is higher than other Plan options, but the coinsurance is lower • HRA funding is based on the number of family members covered • In-network: $1,500 Individual/ $4,500 Family • Out-of-Network: $3,000 Individual/ $9,000 Family • After the deductible is met, the member only pays the 15% coinsurance • The deductible applies to both Pharmacy and Medical expenses • If the member reaches his or her deductible and coinsurance out-ofpocket maximum, the Plan pays 100% of the covered expenses for the rest of the benefit year (medical and pharmacy) 14 • $500 for employee/retiree only • $1,000 for employee/retiree + 1 $1,500 for employee/retiree + 2 or more dependents • HRA funds are used to pay a portion of the members’ deductibles & coinsurance • Once the HRA is depleted, the member must pay the remaining deductible & coinsurance • Incentives available to add value to HRA • Unused HRA funds are available the following year The Consumer-Directed Health Plan (CDHP) A High Deductible Health Plan is exactly what it says – A plan with a high front-end deductible. • After meeting the deductible the member pays a 15% coinsurance on all innetwork medical and pharmacy benefits except ACA preventive services and ACA preventative medications, which are covered at 100%. • The pharmacy and medical deductible and out-of-pockets are shared. • An additional CDHP preventive medication list is covered with no deductible meaning the member is subject to 15% of eligible expense only. 15 Consumer Directed Health Plan (CDHP): Pharmacy Benefits The Deductible Does Not Apply to Every Medication • Under the Affordable Care Act, many ACA preventive medications are paid at 100% • Medications on the CDHP Preventive medication are subject to 15% coinsurance with no deductible. Example of medications include those used to treat heart disease or stroke, asthma, and diabetes. These 2 different medication lists will be posted online at www.shpnc.org. 16 How The HRA Helps The Member Meet Their Deductible Coverage Type HRA Pays You Pay Total Deductible Employee Only Remaining Deductible $1,000 In-Network $1,500 First $500 Out-of-Network Remaining Deductible $2,500 $3,000 Employee + One Family Member In-Network Remaining Deductible $2,000 First $1,000 Out-of-Network Remaining Deductible $5,000 $3,000* $6,000 Employee + Two or more Family Members In-Network Out-of-Network Remaining Deductible $3,000 First $1,500 Remaining Deductible $7,500 $4,500* $9,000 *The HRA is a pooled account and is available to whichever family member needs it first. It is possible for one family member to use all the funds before another family member has a claim. 17 How the Consumer-Directed Health Plan with HRA Works Member presents HRA ID Card at Office Visit Total office visit of $175 submitted to BCBSNC by provider #6 #1 Member's Individual Deductible At end of the month, $15 credited to member’s HRA for visiting PCP on ID Card #5 Claim processes in primary claims system and applies towards $1,500 deductible – EOB/EOP issued Pharmacy claim automatically submitted to HRA Member reimbursed $65 Claim automatically rolls over to HRA for adjudication - $175 remitted to provider- Member picks up prescription at pharmacy and pays $65 because deductible has not been met #4 #2 #3 Beginning Deductible Office Visit Rx Remaining Deductible $1,500 ($175) ($65) $1,260 HRA Account First Medical Cost of the Year Beginning Balance $500 Office Visit ($175) Rx ($65) Remaining HRA Balance $260 PCP Incentive Reward $15 New HRA Balance $275 To monitor HRA balance and claim’s payments, members may go online to www.shpnc.org and click on My Member Services. 18 Lower Premiums with Wellness Premium Credits—CDHP Complete up to Three Wellness Activities By October 31, 2013 CDHP Premium Credits Subscriber attests to being a nonsmoker/commits to a cessation program and attests for spouse if applicable $20 per month Subscriber (only) completes a confidential Health Assessment (HA) $10 per month Subscriber selects a Primary Care Provider (and any covered dependents) $10 per month Reduce subscriber premium by … 19 $40 per month Lower Member Health Care Costs with Wellness Incentives—CDHP Things you can do to reduce your costs… CDHP Incentives Visit the PCP listed on ID card $15 added to the HRA Visit a Blue Options Designated specialist $10 added to the HRA Get inpatient care in a Blue Options Designated hospital $50 added to the HRA Remember: Get preventive care through an in-network 100% coverage – this is provided at provider in a non-hospital setting no cost to the member 100% coverage – this is provided at no cost to the member 15% of eligible expense with no deductible ACA preventive medication list CDHP preventive medication list 20 CDHP Highlights in 2014 Coverage Plan-Provided HRA Contribution Annual Deductible In-Network Out-of-Network $500 employee/retiree $1,000 employee/retiree + 1 dependent $1,500 employee/retiree + 2 or more dependents $1,500 individual/$4,500 family Coinsurance 15% of eligible expenses (after deductible is met) Out-of-Pocket Maximum for medical and pharmacy $3,000 individual/$9,000 family (includes deductible) 15% of eligible expenses; $15 added to HRA Office Visits if the PCP on the ID card is utilized; $10 (after deductible is met) added to HRA if a Blue Options Designated specialist is utilized Inpatient Hospital (after deductible is met) ACA Preventive Medication List CDHP Preventive Medication List $3,000 individual/$9,000 family 35% of eligible expenses $6,000 individual/$18,000 family 35% of eligible expenses 15% of eligible expenses; $50 added to HRA if a Blue Options Designated hospital is 35% of eligible expenses utilized $0 coinsurance, $0 deductible $0 coinsurance, $0 deductible 15% coinsurance, $0 deductible 15% coinsurance, $0 deductible 21 The Traditional 70/30 Plan • Traditional 70/30 Plan – The new name for the current 70/30 Basic Plan; there are no changes to the Plan’s benefits for 2014 • Copays and Deductibles – The copays and deductibles on the Traditional 70/30 PPO plan are the same as they are today on the 70/30 Basic Plan. There will be no opportunities for copay reductions on the Traditional 70/30 Plan. • Network Services – Members may visit any provider, but they will pay less when they go to a BCBSNC network provider • Preventive Services – Copays still apply to preventive services. 22 Traditional 70/30 Plan Benefit Highlights Coverage In-Network Out-of-Network Annual Deductible $933 individual/$2,799 family $1,866 individual/$5,598 family Coinsurance (after deductible is met) 30% of eligible expenses 50% of eligible expenses plus 100% of amount above the allowed amount Coinsurance Maximum (excludes deductible) $3,793 individual/$11,379 family $7,586 individual/$22,758 family Office Visits $35 copay for primary doctor $81 copay for specialists 50% after deductible Preventive Care $35 copay for primary doctor $81 copay for specialists Only certain services are covered Inpatient Hospital $291 copay, then 30% after deductible $291 copay, then 50% after deductible Tier 1 $12 copay Tier 1 $12 copay Tier 2 $40 copay Tier 2 $40 copay Tier 3 $64 copay Specialty medications 25% up to $100 maximum per 30-day supply Tier 3 $64 copay Specialty medications 25% up to $100 maximum per 30-day supply Prescription Drugs (for 30-day supply) 23 Monthly Premiums—Enhanced 80/20 Plan 2014 Enhanced Plan Premiums (Active Employees and Non-Medicare Primary Members) Coverage Type Employee/ Retiree Monthly Premium Dependent Monthly Premium Total Monthly Premium Wellness Premium Credits* Net Monthly Premium* Employee/Retiree Only $63.56 N/A $63.56 $50.00* $13.56* Employee/Retiree + Child(ren) $63.56 $272.80 $336.36 $50.00* $286.36* Employee/Retiree + Spouse $63.56 $628.54 $692.10 $50.00* $642.10* Employee/Retiree + Family $63.56 $666.38 $729.94 $50.00* $679.94* *Assumes completion of three wellness activities 24 Monthly Premiums—CDHP 2014 CDHP Premiums (Active Employees and Non-Medicare Primary Members) Coverage Type Employee/ Retiree Monthly Premium Dependent Monthly Premium Total Monthly Premium Wellness Premium Credits* Net Monthly Premium* Employee/Retiree Only $40.00 N/A $40.00 $40.00* $0* Employee/Retiree + Child(ren) $40.00 $184.60 $224.60 $40.00* $184.60* Employee/Retiree + Spouse $40.00 $475.68 $515.68 $40.00* $475.68* Employee/Retiree + Family $40.00 $506.64 $546.64 $40.00* $506.64* *Assumes completion of three wellness activities 25 Monthly Premiums—Traditional 70/30Plan 2014 Traditional Plan Premiums (Active Employees and Non-Medicare Primary Members) Coverage Type Employee/ Retiree Monthly Premium Dependent Monthly Premium Total Monthly Premium Employee/Retiree Only $0 N/A $0 Employee/Retiree + Child(ren) $0 $205.12 $205.12 Employee/Retiree + Spouse $0 $528.52 $528.52 Employee/Retiree + Family $0 $562.94 $562.94 Reminder: Wellness premium credits are not offered under the Traditional Plan. 26 Completing Open Enrollment • Action must be taken during Open Enrollment—October 1–31, 2013: • Choose a health plan • Decide whom to cover • Complete wellness activities • Remember, NC Flex Benefits enrollment in Oct. as well. • Online enrollment only – through the eEnroll or BEACON platform, depending on your agency • Choices are effective from January 1, 2014 through December 31, 2014 If you do not complete your enrollment by October 31, 2013, you, and any currently covered family members will be enrolled in the Traditional 70/30 Plan effective Jan. 1, 2014. 27 Enrollment Instructions BEACON • Employee Self Service (ESS), available on the BEACON website at https://mybeacon.nc.gov. Select the “My Benefits” link to begin enrollment. • For instructions, click on the “Read Before Beginning Online Enrollment” link. • Members without ESS access may contact BEST Shared Services at 919-707-0707 (in Raleigh) or 866-622-3784 (statewide) to complete enrollment by phone. eEnroll • All changes need to be done through the eEnroll system by logging in to the system at https:// shp-login.hrintouch.com to enroll. For assistance in navigating eEnroll members can call Benefitfocus Customer Service at 855-859-0966. 28 Resources for Members • Please READ your mail! • There will be 4 mailers sent to you to assist you in your decision. • SHP Website • There will be 4 instructional videos posted to the Plan’s website. • Premium Rate Calculator tool available online in September • Enrollment tour will be conducted across the state in October, more information will be included in one of your mailers • Sign up for our monthly electronic newsletter, Member Focus, which can be done by visiting the Plan’s website 29 Important Numbers • ELIGIBILITY AND ENROLLMENT for eEnroll Agencies 855-859-0966 • BEST SHARED SERVICES: BEACON 919-707-0707 • BLUE CROSS AND BLUE SHIELD OF NC (BENEFITS, CLAIMS and HRA) 888-234-2416 • EXPRESS SCRIPTS (PHARMACY QUESTIONS for Active/Non-Medicare Retirees) 800-336-5933 30 Thank you! www.shpnc.org www.nctreasurer.com 31