Nephrotic Syndrome Case Presentation
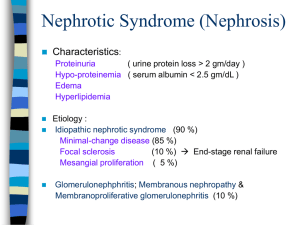
advertisement

Tuesday 4th January 2011 Dr Matthew Home NEPHROTIC SYNDROME CASE PRESENTATION CONTENTS Case presentation Definition Causes Guidelines References PREVIOUS HISTORY Born AGH Term (40 weeks) Apgars 71 / 95 Well since Immunisations up-to-date Four brothers (8, 11, 16, 17 yrs) all well No regular medications NKDA PRESENTATION S/B GP ~14/09/2010 Facial swelling – particularly periorbitally Loss of Appetite Flu symptoms (Rhinorheoa, Fevers) a few weeks before Arrange bloods and follow-up appointment Follow-up appointment not attended S/B GP again on 04/10/2010 Abdominal pain and distension Ankle swelling Continued loss of appetite “Drinking plenty of fluids” Increased urine volume No dysuria, haematuria or offensive urine Bowels - trace blood (Recent prolapse) No rash, fever BLOODS / URINE DIP (14/09/2010) Haemoglobin White Cell Count Platelets 13.4 8.8 492 g/dL x109/L x109/L 11.5 - 17.5 3.7 - 15.5 140 - 450 Sodium Potassium Bicarbonate Urea Creatinine Chloride 135 4.4 24.5 2 18 106 mmol/L mmol/L mmol/l mmol/L umol/L mmol/L 132 - 143 3.2 - 5.7 13 - 29 1.8 - 9.6 27 - 88 96 - 114 Calcium Total Protein Albumin ALT 12 Alkaline Phosphatase Total Bilirubin 2.07 35 less thn 10 IU/L 118 6 mmol/L g/l 2.14 - 2.62 56 - 77 Nov-39 IU/L umol/L 110 - 302 0 - 34 Vitamin D Free T4 Ferritin TSH 8.58 17 8.7 19 miu/L nmol/L 60 - 150 pmol/L 7.5 - 21.1 ng/mL 14 - 180 0.34 - 5.6 EXAMINATION P 118, BP 109/63, SaO2 99% RA Chest – Clear HS - I + II + 0 ENT - NAD Abdomen moderately distended (Ascites) No palpable L/S/K/K Peripheral odema + BLOODS ON ADMISSION (04/10/2010) Haemoglobin White Cell Count Platelets 13.7 7.7 437 g/dL x109/L x109/L 3.7 - 15.5 140 - 450 11.5 - 17.5 Sodium Potassium Bicarbonate Urea Creatinine Chloride 136 4.1 23.8 3.2 13 105 mmol/L mmol/L mmol/l mmol/L umol/L mmol/L 132 - 143 3.2 - 5.7 13 - 29 1.8 - 9.6 27 - 88 96 - 114 Calcium Total Protein Albumin Corrected Calcium Globulin ALT Alkaline Phosphatase Total Bilirubin 2.21 47 16 2.69 31 18 91 8 mmol/L g/l g/L mmol/L g/L IU/L IU/L umol/L 2.14 - 2.62 56 - 77 31 - 48 2.14 - 2.62 23 - 41 11-39 110 - 302 0 - 34 mmol/L IU/mL miu/L pmol/L 3.0 - 12.0 0 - 200 0.34 - 5.6 7.5 - 21.1 Blood Culture (Aerobic): No growth (5 days) VZV IgG Antibodies Plasma Glucose Antistreptolysin-O TSH Free T4 Thyroid Peroxidase Positive 4.8 1 10.72 7.5 Less than 10 URINE DIP Protein +++ DIAGNOSIS 1. 2. Nephrotic Syndrome Vitamin D Deficiency NEPHROTIC SYNDROME DEFINITION Nephrotic range proteinuria (> 1g/m2/day) Hypoalbuminaemia (<25 g/l) Oedema Classification Idiopathic (primary) nephrotic syndrome Minimal change (80-90%) Focal segmental glomerulosclerosis (FSGS) (10-20%) Secondary nephrotic syndrome (HSP, SLE, MPGN) Congenital nephrotic syndrome MINIMAL-CHANGE DISEASE (MCD) Also known as lipoid nephrosis or nil disease It refers to a histopathologic lesion in the glomerulus Disorder of T cells, which release a cytokine that injures the glomerular epithelial foot processes. FOCAL SEGMENTAL GLOMERULOSCLEROSIS ?viral- or toxin-mediated damage or intrarenal hemodynamic changes such as hyperperfusion and high intraglomerular capillary pressure 1. 2. 3. Injury to podocytes shrinkage/collapse of glomerular capillaries scarring (glomerulosclerosis) NEPHROTIC SYNDROME - CAUSES Idiopathic NS MCNS FSGS MPGN Membranous glomerulonephritis (MGN) IgA nephropathy Idiopathic crescentic glomerulonephritis Secondary nephrotic syndrome Infections Drugs Genetic nephrotic syndrome/congenital nephrotic syndrome Finnish-type congenital nephrotic syndrome (NPHS1, nephrin) Denys-Drash syndrome (WT1) Frasier syndrome (WT1) Diffuse mesangial sclerosis (WT1, PLCE1) Autosomal recessive, familial FSGS (NPHS2, podocin) Autosomal dominant, familial FSGS (ACTN4, α-actinin4; TRPC6) Nail-patella syndrome (LMX1B) Pierson syndrome (LAMB2) Schimke immuno-osseous dysplasia (SMARCAL1) Galloway-Mowat syndrome Oculocerebrorenal (Lowe) syndrome Congenital syphilis, toxoplasmosis, cytomegalovirus, rubel la Hepatitis B and C HIV/acquired immunodeficiency syndrome (AIDS) Malaria Penicillamine Gold Nonsteroidal anti-inflammatory drugs (NSAIDs) Interferon Mercury Heroin Pamidronate Lithium Systemic disease Systemic lupus erythematosus Malignancy - Lymphoma, leukemia Vasculitis -Wegener granulomatosis, Churg-Strauss syndrome, polyarteritis nodosa, microscopic polyangiitis, Henoch-Schönlein purpura (HSP) Immune-complex–mediated - Poststreptococcal glomerulonephritis NEPHROTIC SYNDROME - IDIOPATHIC Typical Features Atypical Features Age 1-10 years <1yr, >10years Normotensive Hypertensive Normal Adrenal Function Elevated Creatinine +/- microscopic haematuria Macroscopic Haematuria NEPHROTIC SYNDROME - INVESTIGATIONS Blood: FBC, U+E’s; Creatinine; LFT’s; ASOT; C3/C4; Varicella titres Urine: Urine culture and Urinary protein/creatinine ratio BP Urinalysis including glucose A urinary sodium concentration can be helpful in those at risk of hypovolaemia. Varicella status should be known in all children commencing steroids. Hepatitis B status may be appropriate in children at high risk. NEPHROTIC SYNDROME - REFERRAL Age < 1 yr Age > 10-12 yrs Persistent hypertension Macroscopic haematuria Low C3/C4 Failure to respond to steroids within 4 weeks NEPHROTIC SYNDROME - COMPLICATIONS Hypovolaemia Despite Infection Loss odema may be intra-vascularly depleted of complement components Thrombosis Loss of proteins and exacerbated by hypovolaemia TREATMENT Prednisolone Penicillin prophylaxis Salt/Fluid Restriction Vaccination +/- Ranitidine Albumin where indicated + Frusemide midinfusion MONITORING Remission – 3+ days of trace / - protein on dipstick testing Up to 60 - 70 % of children may have one or more relapse. Urine check twice weekly initially, then weekly TREATMENT OF RELAPSING NS Prednisolone Albumin Salt Restriction Penicillin Varicella vaccine Consider between relapses in children who are varicella seronegative. REFERRAL OF RELAPSING NS Referral to / Discussion with Paediatric Nephrology if Frequent relapsers Steroid dependency Steroid toxicity FREQUENT RELAPSES Frequent relapsers are diagnosed if there is: 2 or more relapses within the first 6 months of presentation 4 or more relapses within any 12 month period This becomes steroid dependency if the relapses are occurring during steroid tapering. Varicella status should be repeated 6 monthly in those who are non-immune. TREATMENT OF FREQUENT RELAPSES Low Dose Alternate Day Prednisolone Levamisole Cyclophosphamide Cyclosporin Mycophenylate Mofitil (MMF) OUR CASE - PLAN Prednisolone 60mg/m2 Ranitidine Penicillin V Dalavit Vit D Suppliments HAS 20% @ 5ml/kg with Frusemide 1mg/kg half way through x3 Urinalysis with each void Monitor daily urine output Daily weights – adjust fluid restriction accordingly Fluid restrict to 600ml/day D/W Leeds renal team CASE PROGRESS Review 15/10/10 Odema settled Persistent Proteinuira Pro+++ Penicillin V stopped Continue Prednisolone Review 29/10/10 Persistent Pro+++ Prednisolone changed to 40mg/m2 - 25mg alt days Review 22/10/10 Odema settled Persistent Proteinuira Pro+++ Penicillin V stopped Continue Prednisolone Review 13/11/10 Persistent Pro+++ Restart Penicillin V 125mg BD Referred to Paediatric renal team for ?renal biopsy REFERENCES www.gpnotebook.co.uk/ http://emedicine.medscape.com/ http://www.clinicalguidelines.scot.nhs.uk/ www.newcastle-hospitals.org.uk/