Nephrotic Syndrome - Sydney Paediatrics
advertisement

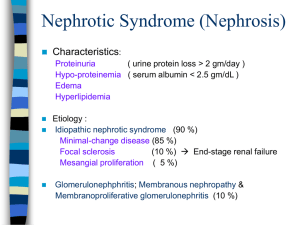
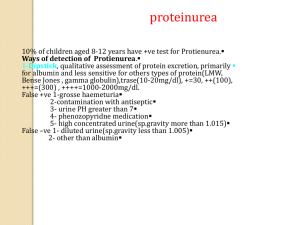
Nephrotic Syndrome Fact Sheet Disclaimer: This fact sheet is for education purposes only. Please consult with your doctor or other health professional to make sure this information is right for your child. What is it? Nephrotic Syndrome is a condition which affects the kidneys. It causes the loss of large quantities of protein in the urine, so that the level of protein in the blood drops. Symptoms Proteins in the blood usually keep fluid within the blood stream. When proteins are lost in the urine, fluid leaks into the body tissues causing swelling (oedema). Swelling is particularly noticeable around the eyes and lower legs, but can occur anywhere in the body, including inside the abdomen, which can cause vomiting and diarrhoea. Children with nephrotic syndrome may feel tired. Some children may not pass as much urine as normal and sometimes frothing of the urine is noticed. Who gets it? Nephrotic syndrome is uncommon. Every year approximately two to seven children in every 100,000 develop nephrotic syndrome, so in any one year less than 50 children in Sydney will develop it. . Nephrotic syndrome often starts between the ages of two to five years, affecting twice as many boys as girls. How is it Diagnosed? A simple urine test will detect high levels of protein. A blood test will show low levels of protein. What causes it? In most cases there is no known cause of nephrotic syndrome. Treatment Corticosteroid medication (prednisolone or prednisone, also known as steroid medications) will be prescribed for your child. Most children with nephrotic syndrome respond well to steroid treatment. The protein disappears from the urine and then the swelling is lost within a week or two. This is called remission. Some children take longer to go into remission. The term remission is used rather than cure because protein loss in the urine can return and swelling can come back. This is known as a relapse. Most children will relapse at least once and some several times. Each relapse requires more steroid treatments. Sometimes coughs and colds can trigger a relapse. Please note, corticosteroids are different to steroids used by body builders (anabolic steroids). What should I know about the steroid treatment? Your child will need a course of high dose steroids with each relapse. Not all children experience side-effects from steroid treatment and any effects are temporary and will stop when the course of steroids has finished or reduced to low every other day doses. Some common side-effects are increased appetite which may lead to weight gain, swollen cheeks, behavioural changes such as temper tantrums and moodiness, and acne in adolescent children. A review of trials found that giving a long course of steroids after the first episode reduces the risk of relapses in the future, without an increase in serious side effects. If your child becomes ill while taking steroids, he/she may require extra treatment. Always remember to tell new doctors that your child has been taking corticosteroids. What do I have to do at home? You need to test your child’s first urine for protein every morning unless told otherwise. Normally the testing strips will be Multistix®. There is no need to test the urine for other substances at home. It is essential you keep a diary of all your child’s urine results for each day and bring it with you to each clinic visit. This is very important as it enables the doctor or nurse to review your child’s progress. The doses of Prednisolone (or prednisone) given each day and any other treatment should be recorded next to the daily urine result. You may also wish to include any other comments, for example, your child’s appearance or how they are feeling. (See Nephrotic Syndrome Diary Record). The urine results in the diary will show how your child is responding to treatment or when they have relapsed. Records that are complete and accurate give the doctor or nurse a good idea of your child’s general health and progress. If your child’s urine shows ‘protein 3+’ or ‘protein 4+’ for three days in a row then this could mean there is a relapse and you should contact your doctor or nurse. If they have no protein (negative) or trace for three days in a row they are in remission and should be well. What other treatment may be necessary? Some children with nephrotic syndrome relapse more frequently and begin to have side effects from the steroids. Other treatments may be used to help your child have longer periods of remission, therefore reducing the amount of steroids taken. Your doctor will tell you about such medications if it is necessary. There are a small group of children with nephrotic syndrome who do not respond to steroid treatment and continue to have lots of protein in their urine. These children usually require a kidney biopsy to investigate what is happening inside the kidney. The doctor will always discuss the need for further treatment or investigations before a biopsy or other medications are suggested. Is there a special diet? You need to encourage your child to eat a balanced healthy diet. It is a good idea for all members of the family to also follow a healthier eating plan. A ‘no added salt’ diet is encouraged especially when they are in a relapse. Avoid adding salt to food at the table and try to reduce the intake of processed foods, for example potato chips, tinned and packet foods. Can my child lead a normal life? Yes. You do not need to keep your child off school, even when they relapse. Children should only miss school if they are really unwell with symptoms. There is no need to restrict their activity. Exercise is important for all the family. A full level of activity is possible when in remission and many children continue to manage a full range of sports and activities even when in a relapse. What about childhood illnesses? Proteins are used in the body for growth and repair and form part of the immune system. When your child has heavy protein loss in the urine they will be more susceptible to infections. If your child develops diarrhoea and/or vomiting while taking any of the medications contact your doctor or nurse. Medications used to treat Nephrotic Syndrome suppress your child’s immunity. Your child could become very unwell if in contact with chicken pox or measles. Let the hospital know if your child has been in close contact with another child with chicken pox or measles. Speak to your child’s school about the possibility. What about immunisations? Steroids can reduce the effect of immunisations and your child may be unwell or relapse if immunisations are given without medical advice. If your child is due immunisations please discuss this with your doctor. What about holidays? Unless your child is having complications a normal family holiday will be possible. Discuss your plans with the doctor or nurse and ensure you take enough medications with you should a relapse occur whilst you are away. What is the outlook for children with nephrotic syndrome? For some children relapses may go on happening for many years. As they become older the relapses usually become less frequent and virtually all children will eventually grow out of the condition. It is not possible to predict when the relapses will cease but a relapse is very uncommon if the child’s urine has been protein free for five years. There is no risk of developing kidney failure in children with the usual types of nephrotic syndrome that continue to respond well to steroid treatment. This means that your child will not need dialysis or a transplant as long as the protein goes when they are given steroids. You should call the doctor or nurse if: - - your child is puffy and unwell, with any of the following symptoms: fever, dizziness, feeling sick or complaining of abdominal pain. Abdominal pain is very important, particularly if your child has cold hands, feet and nose. If this happens, it means that the blood has become thicker, and you need to contact your doctor straight away your child has a fever 38° or above and is in relapse your child has diarrhoea or vomiting you think your child has had close contact with chicken pox or measles your child requires immunisations