Brucella, Haemophilus, Staphylococcus, Streptococcus
advertisement

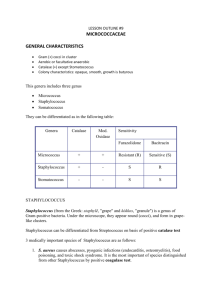
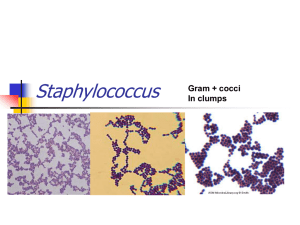
BRUCELLA MAIN SPECIES Brucella melintensis Brucella abortus Brucella suis NORMAL HABITAT Obligate intracellular pathogens of animals B. melitensis mainly found in goat and sheep B. abotus infects cattle B. suis found in pigs and occasionally in goat Other animal including horse, camel, eland and wild rodents ROUTES OF INFECTION Mosquitoes helps in transfer Brucella from animal to human Also by ingesting unpastuerized milk or milk products, enter damaged skin or eyes, inhaled in airborne particles or aerosols. LABORATORY DIAGNOSTICS MICROSCOPIC OBSERVATION Non-motile Gram negative Coccobacili Show bipolar staining Rarely found in direct smear from uncultured specimen On Gram stain they appear as dense clumps of Gram-negative coccobacilli and are exceedingly difficult to see. CULTURE CHARACTERISTICS Mostly cultured from blood of high fever patient(Brucellosis) Isolation is extremely rare in chronic brucellosis In all blood culture, they need carbon dioxide Blood culture should be kept in 4 – 6 weeks before result as no organisms isolated To reduce the risk of contamination, use the diphasic medium such as Castaneda or tryptic soy broth or agar Brucellae are aerobic with enriched of carbon dioxide BIOCHEMICAL TESTS SEROLOGY TESTS Urease and hydrogen sulphide production All brucella strains are catalase positive Possess two antigens called A and M Famous test serum: Rapid slide agglutination test Tube agglutination titration test SEROLOGY TEST It is crucial to be able to differentiate Brucella from Salmonella which could also be isolated from blood cultures and are Gram-negative. Testing for urease would successfully accomplish the task; as it is positive for the Brucella and negative for the Salmonella. HAEMOPHILUS MEDICAL IMPORTANT SPECIES Haemophilus influenzae Haemophilus aegyptius Haemophilus ducreyi NORMAL HABITAT H.influenzae (mostly non-capsulated strains), H. parainfluenzae and H.aegyptius is normal flora of the upper respiratory tract Infections causing: 1. Pyogenic meningitis 2. Acute epiglottitis 3. Cellulitis, middle ear infection,etc CONJUCTIVITIS LABORATORY DIAGNOSIS MICROSCOPY Small, non-motile, Gram negative rods or coccobacili Long thread-like form in old csf culture MICROSCOPIC OBSERVATION CULTURE OF H.INFLUNZAE H.influenzae grows better in aerobically compare to anaerobically The optimum temperature for growth 35 – 37oC The are X and V factor Both represent in blood agar and permit the culture to grow H.influenzae and H.aegyptius need X and V factor, H. parainfluenzae need V factor and H.ducreyi need X factor BIOCHEMICAL TESTS Not usually used to identify hemophilus 6 biovars of H.influenzae are recognized based on the indole, urease and ornithine decarboxylase (ODC) reactions of the diff strains SEROLOGY Consist of 1 – f serotypes Mostly causing meningitis belong to serogroup b Most strains that cause chronic bronchial disease are non-capsulated Antimicrobial sensitivity Resistant towards chloramphenicol, ampicilin, tetracycline, erythromycin and cotrimoxazole H. ducreyi is sensitive to sulphonamides Ampicillin resistant are common STAPHYLOCOCCUS & STREPTOCOCCUS STAPHYLOCOCCUS Staphylococcus aureus Staphylococcus epidermidis Staphylococcus saprophyticus INTRODUCTION Are microbial flora of the skin, upper respiratory tract and intestinal tract S.aureus usually cause abscesses, boils, conjuctivitis, pneumonia, septicemia, food poisoning and scalded skin syndrome S. epidermidis causing bacteraemia S. saprophyticus causing cystitis and acute urethritis LABORATORY DIAGNOSIS Microscopy Non-motile Non capsulate Gram positive cocci Arrangement single or in pair Size 1 µm diameter CULTURE Grow well in aerobically and also in present of carbon dioxide Temperature between 10 – 420C, optimum temperature are between 35 - 370C S.AUREUS Produce yellow to cream in blood and chocolate agar (heated agar) Occationally produce white 1-2 mm in diameter colonies Some strain produce beta-hemolytic when grown aerobically Colonies are slightly raised and easily emulsified on a slide Non- lactose fermenter in MacConkey agar Mannitol salt agar is a useful differential and selective agar to identify S.aureus ON BLOOD AGAR S.EPIDERMIDIS Colony is white Non hemolytic in blood agar S. saprophyticus Maybe white or yellow There are non-hemolytic in BA Not grow anaerobically No growth in MacConkey agar BIOCHEMICAL REACTIONS S.aureus DNAse test will be positive for S.aureus but negative in other species Catalase test will be positive in all staphylococcus but negative in all streptococcus S. epidermidis and S. saprophyticus Coagulase negative DNAse negative Catalase positive ANTIMICROBIAL SENSITIVITY Erythromycin Clindamysin Fucidin Vancomycin Many strains of S.aureus are penicillin-resistant S.epidermidis are more resistant than S.aureus to antibiotics S. saprophyticus less resistant to antibiotics than S.aureus and S.epidermidis STREPTOCOCCUS Streptococcus pyogenes Streptococcus agalactiae Enterococci TO BE CONTINUE.. Explain what happens in the following biochemical tests: i) Indole test ii) Methyl red test 8 marks) b) Write the scientific name of a bacterium that gave positive results for both tests. (2 marks) QUESTION State all group of gram positive and gram negative bacteria.