The Acute Red Eye
advertisement

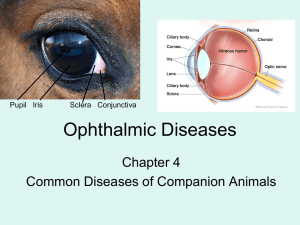
The Acute Red Eye Jonathan Goh Background One of the most common eye complaints May present to GP, ED, or Optometrist Varied aetiologies (a lot!) Commonly self limiting / benign But – serious sight threatening pathology may present as an acute red eye Initial approach History Onset Location – bilateral / unilateral / sectoral Painful or painless – discomfort, gritty, foreign body sensation, itch, ache, sharp, pain on movement Visual disturbance Photosensitivity Discharge – watery or purulent Trauma to eye – e.g. hammering ?contact lens Anyone else with red eye Recent travel POHx and PMHx Examination Inspect whole patient Visual Acuity + pin hole Conjunctiva – bulbar and palpebral (evert lid) Sclera Cornea – clarity, fluorescein (abrasions, ulcers), sensation Pupil – shape, reaction, accomodation Eye movements – painful? Full?, diplopia? Fundoscopy / slit lamp Fluorescein Tonometry Lymph nodes - preauricular Common Causes Conjunctiva Conjunctivitis Bacterial Viral Allergic Subconj haemorrhage Scleritis and episcleritis Pterygium Pingueculum Cornea Ulcer / abraision Bacterial keratitis Herpetic keratiis Foreign body Anterior chamber Anterior uveitis/iritis/vitritis Eye lids Blepharitis Chalazion / stye Sub tarsal FB Canaliculitis Dacrocystitis Marginal keratitis Angle-closure glaucoma Herpes Zoster ophthalmicus Trauma Preseptal and orbital cellulitis Case 1 28 YO male Previously well 2 day history of red eyes, grittiness and mucopurulent discharge Difficulty opening eyes on waking Vision clears on blinking Conjunctivitis Bacterial Viral Allergic Gonoccocal / Chlamydial Conjunctivitis - Bacterial Usually bilateral (within 48 hrs) 70% Gram+ve: Streptococcus pneumoniae, Staphylococcus aureus 30% Gram-ve: Haemophilus influenzae, Morxella catarrhalis Symptoms: Grittiness / burning, mucopurulent discharge, matting of eye lids, crusting, NO photophobia, NO visual disturbance Signs: Crusty/purulent lids, conjunctival hyperaemia, mild papillary reaction, oedematous conjunctiva/lids, diffuse injection of conjunctiva (tends to be worse in fornices) NO corneal or anterior chamber involvement Treatment: Hygiene, topical antibiotics for 5 days (e.g. chloramphenicol) Conjunctivitis - Viral Acute onset Uni or bilateral Usually adenovirus type 3, 4,or 7 History of URTI, may be epidemic May develop late keratitis Symptoms: Grittiness, watery/serous discharge, NO visual disturbance Signs: Watery, discharge, Preauricular LN, diffuse conj injection, eye lid oedema, follicles Treatment: Supportive, hygeine, eye lubricants, may take weeks to resolve Conjunctivitis - Allergic IgE mediated Tends to be seasonal Bilateral Symptoms: itch, +/- watery discharge, NO visual disturbance FHx of atopy Signs: diffuse conj injection bilaterally, papillae, chemosis, mild eyelid swelling Treatment: avoid allergen, cold compresses, topical antihistamines, mast cell stabiliser, NSAIDs, vasoconstrictor Conjunctivitis – Chlamydial and Gonococcal Sexually active – genitals>hand>eye (can also occur in new born via birth canal) Chlamydial: subacute, FB sensation, purulent discharge, preauricular LN Gonococcal: Hyperacute presentation with purulent discharge +++, chemosis, papillary reaction, preauricular LN, May lead to infection keratitis Swab – N gonorrhoea: microscopy G-ve diplococci, cultures Treatment: refer to ophthalmologist, systemic antibiotics Workup for STIs Conjunctivitis Case 2 70 YO F Noticed that part of the white of her eye became bright red after a bout of coughing. No pain, no visual disturbance, no discharge. PHx: AF (warfarin), T2DM, COPD, HTN Subconjunctival Haemorrhage Due to bleeding of conjunctival or episcleral vessel Spontaneous, trauma, systemic illness, anticoagulation, unilateral Hx of anticoagulants/platelets, bleeding disorder, trauma/rubbing, coughing/vomiting Symptoms – red eye, no visual disturbance or pain or discharge Ensure no penetrating injury Check BP, INR (warfarin), lubricate, reassure Case 3 24 YO male apprentice welder presents at 8pm Previously well Sudden onset foreign body sensation, photophobia, tearing, mild conjunctival redness, some visual deterioration. Ultraviolet keratitis / flash burn Tends to occur 8-12 hours after exposure UV damages corneal epithelium Symptoms: Foreign body sensation, tearing, blurring of vision, photophobia Signs: Superficial punctate keratitis (stains with fluorescein), conjunctival injection, chemosis, belpharospasm Treatment: Epithelium usually recovers in 1-3 days, lubricants, analgesia, mydriatics Case 4 35YO male Previously well Poked in right eye Immediately complains of FB sensation, photophobia, tearing, red eye, decreased vision. Corneal abrasion Corneal epithelial defect Commonly due to trauma Symptoms: pain, FB sensation, photophobia, tearing, conjunctival injection Signs: corneal epithelial defect, stains with fluorescein, FB under eyelid Treatment: topical antibiotics, lubricants, analgesia Case 5 5 YO boy Previously well Reaching up to grab something from a shelf in laundry, accidentally spills ammonia on face. Comes in crying, painful red eyes, and decreased vision. Corneal chemical burn Ophthalmic emergency Acid or alkali Alkali penetrate further. Acids coagulate protein forming a protective barrier Causes necrosis of conjunctival and corneal epithelium and stroma possibly leading to perforation. Can lead to corneal opacification, vascularisation, symblepharon Treatment: COPIOUS IRRIGATION, sweep fornices, urgent referral to ophthalmologist, analgesia Corneal Ulcer Destruction of epithlium and stroma due to an infection Risk factors: contact lens, trauma, ocular surface disease, immunosupression Bacterial Often Hx of contact lens use Epithelial defect + opacified base Bacterial Staph epidermidis, Strep pneumoniae, Strep pyogenes, Haemophilus influenza, Morazella catarrhalis, Neisseria spp. Symptoms: pain, watering/discharge, blurred vision, photophobia, discharge Signs: Corneal ulcer, corneal oedema, hypopyon, chemosis, hypopyon Treatment: Urgent referral to ophthalmologist, never patch, cultures, topical antibiotics. Fungal Aspergillus, Candida, or Fusarium Satalite infiltrates common, feathery edges Hx of trauma with organic material Corneal Ulcer Viral Herpes Simplex Virus Usually due to reactivation of Type 1 (can be Type 2) Involvement of CNV1 Hx of stress / immunosupression Symptoms: photophobia, tearing, pain Signs: Dendritic ulcer with terminal bulbs, Reduced corneal sensation, Hutchinson’s sign Treatment: urgent referral to ophthalmologist Usually topical antiviral treatment + mydriatic Case 6 30 YO female Previously well Presents with unilateral red eye with mild pain. States she had a similar episode a few months ago which resolved by itself. Episcleritis and scleritis Episcleritis: inflammation of the episclera (thin membrane covering sclera) Causes: Idiopathic, associated with vascular/connective tissue disorders Rapid onset, grittiness, dull headache, +/- watery discharge, NO visual disturbance Focal areas affected – radial configuration of vessels Usually self limiting, may be recurrent Scleritis: inflammation of sclera Infectious, autoimmune mediated May have visual disturbance Scleral oedema/discoloured, congestion of scleral plexus, irregular blood vessels Nodular, diffuse, necrotizing Anterior, posterior Treatment: URGENT REFERAL to ophthalmologist Acute angle-closure glaucoma Due to iris blocking trabecular meshwork outflow tract resulting in raised IOP Damages optic nerve head Worsened by mydriasis – pupil dilation Symptoms: severe ocular pain, blurred vision, halos, headache, nausea/vomiting, abdominal pain. Signs: diffuse injection, corneal oedema (hazy), pupil fixed irregular and mid dilated, raised IOP, ciliary injection Treatment: urgent referral to ophthalmologist, aim is to reduce IOP Acetazolamide, glycerol, mannitol, topical timolol, prednisolone acetate, pilocarpine (miosis, opens TM), peripheral iridotomy Uveitis Inflammation of the iris, ciliary body or choroid. Anterior (iris and ciliary body) 50-70% idiopathic, associated with systemic diseases, infective (TB, syphilis, leprosy, HSV, HZV, HIV, fungal) Sudden onset, red painful eye, tearing, visual disturbance, photophobia Perilimbal injection, flare and cells in AC, keratic precipitates, hypopyon, pupil sluggish Treatment: Urgent ophthalmology referral, mydriatics, analgesia, steroids (after consult with ophthal) May need work up for vascular/inflammatory disorders Consequences: cataracts, glaucoma, retinal detachments, band keratopathy Pitfalls Beware the “unilateral bacterial conjunctivitis” Always check visual acuity Don’t patch corneal ulcers Call for help early