Manual Handling
advertisement
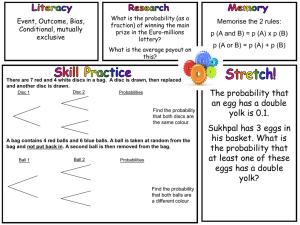
Sunshine Care Training Sarah Yorwerth & Tara Hollinshead What is Manual Handling? Manual Handling at Work involves: Lifting, Lowering, Pulling, Pushing or Carrying. Supporting People: Get in or out of bed Turn over in bed Sit up in bed Bathe Shower Use the toilet Sit in a chair Standing Walking Get up from the floor after a fall, or Get in and out of a vehicle. Legislation There are laws about safety at work. Those laws inform our policies and procedures. Workers as well as managers must Health and Safety law: Health and Safety at Work Act 1974 (HASAWA) Manual Handling Operations Regulations 1992 (2002) Provision and Use of Work Equipment Regulations 1998. Reporting of Injuries, Diseases and Dangerous Occurrences Regulations 1995. (RIDDOR) Health and Safety (First Aid) Regulations 1981. Lifting Operations and Lifting Equipment Regulations 1996 Your Spine The intervertebral discs are under constant pressure. As discs degenerate and weaken, cartilage can bulge or be pushed into the space containing the spinal cord or a nerve root, causing pain. Studies have shown that most herniated discs occur in the lower, lumbar portion of the spinal column. Sciatica is a condition in which a herniated or ruptured disc presses on the sciatic nerve, the large nerve that extends down the spinal column to its exit point in the pelvis and carries nerve fibres to the leg. This compression causes shock-like or burning low back pain combined with pain through the buttocks and down one leg to below the knee, occasionally reaching the foot A slipped disc occurs when the outer case of the disc ruptures (splits), resulting in the gel inside bulging and protruding out of the disc. The damaged disc can put pressure on the whole spinal cord or on a single nerve root. This means that a slipped disc can cause pain both in the area of the protruding disc and in the area of the body that is controlled by the nerve that the disc is pressing on. It is not always clear what causes a disc to break down, although age is a common factor in many cases. 1. Healthy disc 2. Nerve 3. Slipped disc 4. Damaged disc 5. Spinal cord As you get older, your spinal discs start to lose their water content, making them less flexible and more likely to rupture M.S.D’s • Osteoporosis is a metabolic bone disease marked by progressive decrease in bone density and strength. Fracture of brittle, porous bones in the spine and hips results when the body fails to produce new bone and/or absorbs too much existing bone. Women are four times more likely than men to develop osteoporosis. Caucasian women of northern European heritage are at the highest risk of developing the condition. • Fibromyalgia is a chronic disorder characterized by widespread musculoskeletal pain, fatigue, and multiple “tender points,” particularly in the neck, spine, shoulders, and hips. Additional symptoms may include sleep disturbances, morning stiffness, and anxiety. • Spondylitis refers to chronic back pain and stiffness caused by a severe infection to or inflammation of the spinal joints. Other painful inflammations in the lower back include infection in the bones of the spine and inflammation in the sacroiliac joints GoutIs a type of arthritis, crystals of sodium urate (which should be expelled through kidneys, builds up in tiny crystals) forms around the joints. There is usually swelling, severe pain, redness and affects the big toe. Develops rapidly to its worst in 6-24hours and lasts for 3-10 days. Contributory factors are age, gender (men 4xmore likely), obesity, high blood pressure, eating sardines and liver frequently, or drinking beer/spirits. Men who drink 2 or more sugar sweetened drinks a day are 85% more at risk. Treatment is exercise, balanced diet and taking NSAID’s. OsteoarthritisMost common MSD, 1 million people visit their GP every year. Symptoms include Mild inflammation around joints, cartilage damage, ‘knobbly’ bony growths. Affects the knees, hips, spine, big toe and hands. Most common in women over 50. Signs include grating sound, ‘knobbly’ joints, weakness and muscle wastage. Rheumatoid Arthritis: Is pain and swelling in the joints. Especially hands, feet and wrists. Most common in women, between the age of 40-70 around 580,000 in the UK are sufferers. It is an autoimmune disease(immune system attacks itself), it disposes cells in the lining of the joints. Joints become swollen, stiff and painful. Carpal Tunnel Syndrome: Is pain, numbness and tingling in fingers and thumb. It is the compression of the median nerve that controls sensation and movement. The Carpel Tunnel is a narrow passage in the wrist that controls the small bones and tough tissue. 50% of pregnant women get CTS but it does disappear about 3 months after birth. Wrist splints are usually worn to support the area. Surgery may be required to reduce to pressure in severe cases but a lot of cases disappear on their own. Back Pain Back pain (also known as dorsalgia) is pain felt in the back that usually originates from the muscles, nerves, bones, joints or other structures in the spine. half the adult population of the UK (49%) report low back pain lasting for at least 24 hours each year FOUR out of every FIVE adults WILL experience back pain at some stage in their life. 50% of those will experience another attack. Back pain is just as common in adolescents as in adults These chronic patients have considerable discomfort and account for approximately 80% of the social and health care costs. £512 million on hospital costs for back pain patients. acute (less than 4 weeks), sub acute (4 – 12 weeks), chronic (greater than 12 weeks NHS Top Tips Top 10 tips for a healthy back, including lifting advice, how to sit properly and back-strengthening exercises. 1. Exercise your back regularly. Walking, swimming (especially backstroke) and using exercise bikes are all excellent ways to strengthen your back muscles. 2. Always bend your knees and your hips, not your back. 3. Never twist and bend at the same time. 4. Always lift and carry objects close to your body. 5. Try to carry loads in a rucksack and avoid sling bags. 6. Maintain a good posture. Avoid slumping in your chair, hunching over a desk or walking with your shoulders hunched. 7. Use a chair with a backrest. Sit with your feet flat on the floor or on a footrest. Change how you sit every few minutes. 8. Quit smoking. It is thought that smoking reduces the blood supply to the discs between the vertebrae and this may lead to degeneration of these discs. 9. Lose any excess weight 10. Choose a mattress suited to your height, weight, age and sleeping position. Risk Assessing Before attempting to move someone, ask yourself: • Does the person need help to move? • Does the person require help or supervision? • Have you told the person you're moving them? • How heavy is the person you're moving? • Are you healthy and strong enough to move them? • Is there anyone who could help you? • How long will it take? • Is there enough space around you? • Are there any obstacles in the way? • Are you wearing suitable clothing and shoes? Think: P.E.A.C.E P.E.A.C.E • PERSON- Your Client • ENVIRONMENT – Look around you, is it safe? • ACTIVITY- What are you doing? • CARE WORKER- Freshness or Fatigue? • EQUIPMENT- What is available? Hazard or Risk You are stood at the side of the road. You want to cross. You look left, it is clear, you look right and there is a lorry approaching about 1500metres away. In that instance you perform a risk assessment. The hazard is coming towards you, you try to assess the vehicles speed, you assess that the risk of the vehicle hitting you is minimal, so you cross, and continue on your way. Hazard: Is any with the potential to cause harm. Risk: The chance that harm will occur and its severity Hazards The Risk Assessment CATEGORIES: LOW MEDIUM HIGH Eliminating : If you identify a HIGH risk activity, then you must TAKE ACTION to reduce the level of risk or try to remove it. Then you MUST REPORT it Reducing: You must however also give priory to LOW & MEDIUM risks too. Sometimes you cannot eliminate risk factors, but you can manage to reduce the risk to more acceptable level. Always read the care plan. Client characterises grading Completion of this section is to enable staff to assess what level of risk is apparent when handling the client, and considering all factors. A high risk client may require hoisting or more manual handling. The Assessor must take action to make the risk as a low a reasonably practical Detailed Assessment INANIMATE LOADS •T= •I= •L= •E= TASK- What has to be done, how and when and why? INDIVIDUAL- who is providing the task? Can this be safely managed by each member of staff? LOAD- The person or object be move, and factors which affect this ENVIRONMENT- Where is the activity taking place? Fall Prevention… Falls in the elderly are a problem for two reasons. They are more likely to happen than falls in younger people They are more likely to result in serious injury; e.g. 2 common fractures as a result: Wrist fractures (Colle’s fracture or dislocation), Femur fractures. Recurrent falls are defined as those occurring at least three times a year. Comorbidity is a serious problem both in terms of contributing to the cause of the fall and outcome. Falls are DEVASTATING but also EXPENSIVE. Falls can lead to morbidity and mortality. Loss of self-confidence and Reduced quality of life. NICE estimate falls cost NHS £2.3 Billion pounds per year. Risk Factors… Risk factors include: High Age. Female gender Low weight Previous falls Dependency on a Care giver. Orthostatic Hypotension (69% increased risk of having an injurious fall within 45 days after antihypertensive treatment) Medication (especially psychotropic) Polypharmacy (taking lots of medication!) Alcohol Abuse Diabetes Mellitus Confusion and Cognitive impairment Disturbed vision Disturbed balance or co-ordination Gait disorders. Urinary Incontinence Inappropriate footwear. Risk of Injury… Weak bones: With increasing age, conditions with predispose to weakness & fracture occur: Osteoporosis (metabolic bone disease) Osteomalacia (softening of the bone) Paget's Disease (bones become enlarged and weakened) Metastases/Mets.(to bone)(tumour spreads to the bone) Predisposition to falls: This includes the risk factors above. Dementia is a particular, impaired Visuospatial ability is an increased risk. Poor self-protection: Lack of protective subcutaneous fat. Neurological problems (forgetting to cushion the fall) Loss of Consciousness (syncope) Motor and Sensory problems. Multiple Contributory factors (stiff joints, drugs and environmental) The Scope… Consideration of some of the common conditions and risk factors predisposing falls in the elderly. Environment. Loose rugs or mats Electric leads Wet Surface Lighting Furniture Fittings Power and balance: Encourage to keep active. Strengthens muscles and maintains joint position sense and balance. Elderly people who have had a fall lose confidence and become less active. Activity must be encouraged. Modifications for individual’s needs Develop power and balance. Accessing the community. Medication: Drugs can contribute to falls in many ways- need to be reviewed regularly. Sedative medication, including Hypnotics. There is a particular risk of falls in agitated patients with cognitive impairments. Confusion from Psychotropic medication. Polypharmacy is common in elderly. Hypotension caused by: • Diuretics, Vasodilators, Alpha-blockers, Beta-blocks, Insulin Neurological… Minor strokes can cause significant weakness Parkinson’s disease impairs mobility (abnormal posture, freezing, frontal impairment, poor leaning balance and leg weakness) Parkinson’s Gait Parkinson’s Improvement Neuropathy may occur (e.g. Diabetes) Proximal myopathy- muscles become weak and slow to relax (Overactive thyroid, Cushing's syndrome and use of steroids. Impairment of co-ordination. Cognitive impairment e.g. Dementia. Loss of consciousness… Syncope Dizziness Arrhythmias (cardiac output) Convulsions (epilepsy) Drop attacks… Falls are called ‘drop attacks’ if there is no known cause. Cardiovascular disease Carotid Sinus Hypersensitivity (quick ‘low’ in blood pressure, or 3 second pause in the heart beat) Transient Ischaemic Attacks (mini-stroke) Orthostatic Hypotension (fall of at least 20mm Hg blood pressure) Dehydration Visual Disturbance… Cataracts Macular Degeneration Central Retinal Artery/Vein occlusion Visual field defects. Prevention… This means taking measures to prevent falls before they happen! Increasing exercise and physical activity Reviewing medication Changing adverse environmental factors Improving management of any medical conditions. A good history… Was it tripping over something or loss of balance? Loss of Consciousness? History of falls? Drug history Alcohol? Home assessment, Risk Assessment and falls prevention. Examination: Cardio vascular, neurological, functional (gait), MMSE, Vision. NICE (National Institute for Clinical Excellence) People at Risk of Falls: All patients over 65 years. All patients between 50-64 judged by a clinician due to their condition. An assessment should include: Cognitive impairment Continence problems Falls history Footwear Health Problems Medication Postural instability, mobility/balance problems Syncope syndrome Visual impairment. ABUSIVE PRACTICE • Many of the manoeuvres and lifts passed on over the years are no longer acceptable in every day practice. • A number of these techniques are now considered to be harmful to the client and carers, and also regarded in some instances as physical abuse and rough handling The Nursing & Midwifery Council (2002) defines physical abuse as: ‘Any physical contact which harms clients or is likely to cause them unnecessary and avoidable pain and distress.’ Such abuse can occur due to health and care staff handling clients in a rough manner, often due to ignorance or poor application of manual handling techniques. It can be defined as any method of handling where the carer places a hand or arm under the clients armpit. The use of this lift can cause damage to the carer’s spine, shoulders, wrist and knees. The Drag Lift. Condemned technique in 1981 For the client, there is the potential of injury to the should and armpit. Risk of fractures to the upper arm and dislocation of the shoulder The orthodox (cradle lift) The Orthodox lift involves two carers placing their hands beneath the arms or behind the back and underneath the client’s leg. The involves carer lifting at arms length whilst twisting at the trunk and hold the load away from the centre Condemned technique since 1987. This is likely to cause injury to the clients shoulders and knee’s. The ‘Through arm’ Lift/slide The through-arm lift/slide often occurs whereby two health or care professionals work together at either side of the client to move or slide them into a sitting position on the bed. It can also pose a risk to the carer in relation to their posture and position whilst handling on bed. Condemned technique in 1998. Damage could occur to pressure areas. This lift applies pressure to the clients forearm and underarm. This can make the manoeuvre potentially painful. The Shoulder lift/slide The shoulder or Australian slide/lift is another manoeuvre whereby a client can be moved on a bed by two carers working together. This technique results in dangers to the carer due to an uneven loading, with force applied to one shoulder. Condemned technique in 1996. This lift involves moving or support a client with their arms or hands around the handlers neck. This is particularly dangerous. If the client does not stand, or collapses when his or her arms are around the handlers neck, all their weigh is hung around the neck Bear Hug Condemned Technique. If the client falls backwards their instinct will be to remain clamped around the handlers neck, so causing them to fall. Follow Guidelines • Back injuries cost the UK £5billion in all sectors. • Over 119 million working days are lost each year. • Each year at least 5000 employees in health and social care need time off. • Half of all injuries in the health care sector are related to handling loads. • Every year 4000 nurses are forced into retirement because of back related problems.