Innovation for neck surgery
advertisement
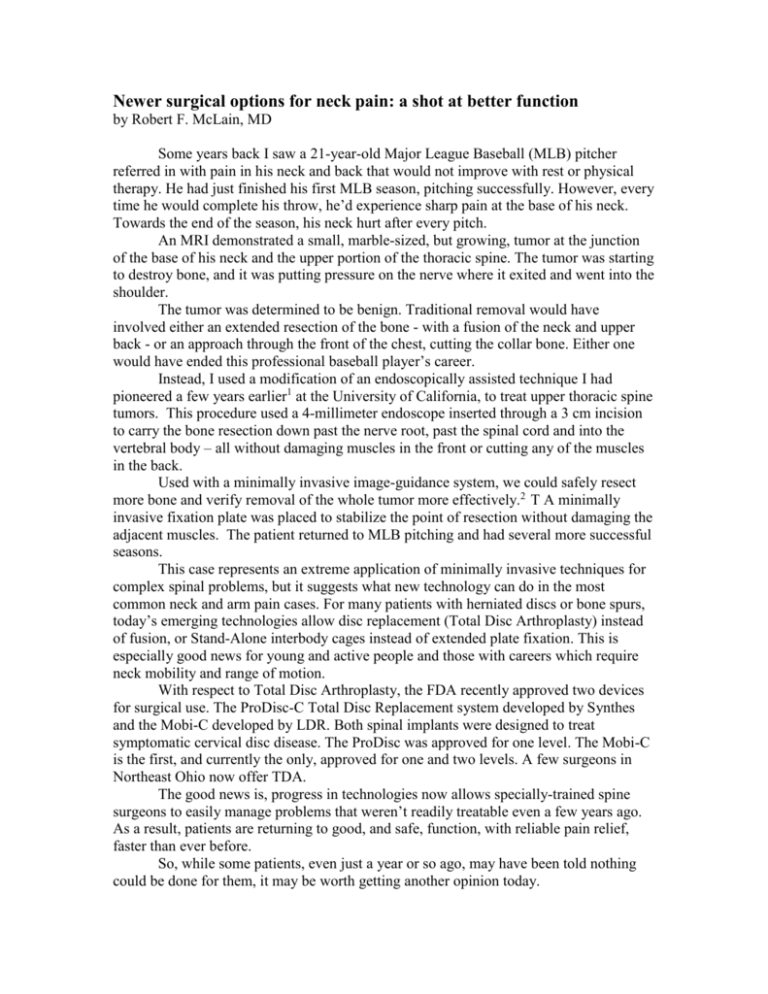
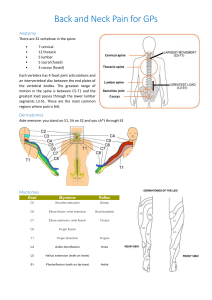
Newer surgical options for neck pain: a shot at better function by Robert F. McLain, MD Some years back I saw a 21-year-old Major League Baseball (MLB) pitcher referred in with pain in his neck and back that would not improve with rest or physical therapy. He had just finished his first MLB season, pitching successfully. However, every time he would complete his throw, he’d experience sharp pain at the base of his neck. Towards the end of the season, his neck hurt after every pitch. An MRI demonstrated a small, marble-sized, but growing, tumor at the junction of the base of his neck and the upper portion of the thoracic spine. The tumor was starting to destroy bone, and it was putting pressure on the nerve where it exited and went into the shoulder. The tumor was determined to be benign. Traditional removal would have involved either an extended resection of the bone - with a fusion of the neck and upper back - or an approach through the front of the chest, cutting the collar bone. Either one would have ended this professional baseball player’s career. Instead, I used a modification of an endoscopically assisted technique I had pioneered a few years earlier1 at the University of California, to treat upper thoracic spine tumors. This procedure used a 4-millimeter endoscope inserted through a 3 cm incision to carry the bone resection down past the nerve root, past the spinal cord and into the vertebral body – all without damaging muscles in the front or cutting any of the muscles in the back. Used with a minimally invasive image-guidance system, we could safely resect more bone and verify removal of the whole tumor more effectively.2 T A minimally invasive fixation plate was placed to stabilize the point of resection without damaging the adjacent muscles. The patient returned to MLB pitching and had several more successful seasons. This case represents an extreme application of minimally invasive techniques for complex spinal problems, but it suggests what new technology can do in the most common neck and arm pain cases. For many patients with herniated discs or bone spurs, today’s emerging technologies allow disc replacement (Total Disc Arthroplasty) instead of fusion, or Stand-Alone interbody cages instead of extended plate fixation. This is especially good news for young and active people and those with careers which require neck mobility and range of motion. With respect to Total Disc Arthroplasty, the FDA recently approved two devices for surgical use. The ProDisc-C Total Disc Replacement system developed by Synthes and the Mobi-C developed by LDR. Both spinal implants were designed to treat symptomatic cervical disc disease. The ProDisc was approved for one level. The Mobi-C is the first, and currently the only, approved for one and two levels. A few surgeons in Northeast Ohio now offer TDA. The good news is, progress in technologies now allows specially-trained spine surgeons to easily manage problems that weren’t readily treatable even a few years ago. As a result, patients are returning to good, and safe, function, with reliable pain relief, faster than ever before. So, while some patients, even just a year or so ago, may have been told nothing could be done for them, it may be worth getting another opinion today. References 1. McLain, RF. Endoscopically Assisted Decompression for Metastatic Thoracic Neoplasms. Spine, 23:1130-1135, 1998. 2. Moore, T, McLain, RF. Image-guided surgery in resection of benign cervicothoracic spinal tumors: a report of two cases. The Spine Journal, Vol 5 (2005), Issue 1, pp. 109–114.