Resuscitation in Pregnancy
advertisement
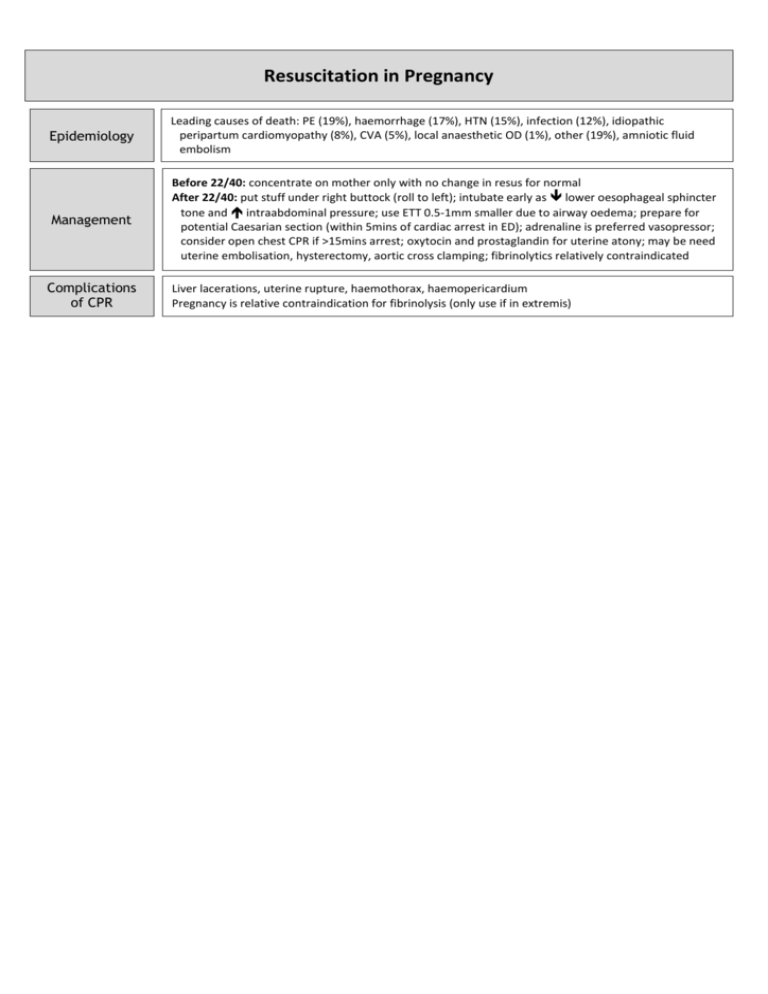
Resuscitation in Pregnancy Epidemiology Leading causes of death: PE (19%), haemorrhage (17%), HTN (15%), infection (12%), idiopathic peripartum cardiomyopathy (8%), CVA (5%), local anaesthetic OD (1%), other (19%), amniotic fluid embolism Management Before 22/40: concentrate on mother only with no change in resus for normal After 22/40: put stuff under right buttock (roll to left); intubate early as lower oesophageal sphincter tone and intraabdominal pressure; use ETT 0.5-1mm smaller due to airway oedema; prepare for potential Caesarian section (within 5mins of cardiac arrest in ED); adrenaline is preferred vasopressor; consider open chest CPR if >15mins arrest; oxytocin and prostaglandin for uterine atony; may be need uterine embolisation, hysterectomy, aortic cross clamping; fibrinolytics relatively contraindicated Complications of CPR Liver lacerations, uterine rupture, haemothorax, haemopericardium Pregnancy is relative contraindication for fibrinolysis (only use if in extremis) TVUS: Empty gestational sac + Empty gestational sac + USS Investigation In Fetal Demise No cardiac activity + No yolk sac No fetal pole + + diameter <20mm = inconclusive do follow up gestational sac diameter >15mm (7/40) OR >21mm (8/40) (90% specificity) gestational sac diameter >9-16mm OR CRL >5-6mm (non-viable) gestational sac diameter >10-13mm gestational sac diameter >18-20mm (non-viable) If beta-hCG above discriminatory zone (>2000) and no IUP, or mass in ovary / tube = likely ectopic (90% PPV) If beta-hCG >6500 and no fetal heart seen on USS = 80% chance of miscarriage If beta-hCG below discriminatory zone (<2000) and inconclusive scan = pregnancy unknown location 48hr follow up (serial beta-hCG’s or repeat USS) Management If unstable: ?cervical shock resus, IV fluids, atropine 600mcg IV if bradycardic (to max 3mg), speculum ASAP; can consider uterine compression, vaginal packs, compression of abdominal aorta, urinary catheter, ergometrine / oxytocin Empathy; pan when toileting Rh prophylaxis – early pregnancy bleeding, singleton, <13/40 250iu IM early pregnancy bleeding, multipleton, >13/40 625iu IM Chance of Rh- mother developing antibodies to Rh+ child is <20% regardless (ie. 15%) of whether antiD is given; Kleihaur done to quantify fetomaternal haemorrhage and thus work out amount to give; of mother’s serum has detectable anti-D antibodies at 24-48hrs then correct dose has been given; if given after 3-10/7, still has some effect; 1ml protects against 6mls of fetal blood; 85% Caucasians are Rh +ive; antiD decreases risk from 1% to 0.3% Complete: conservative management Incomplete / inevitable: women’s preference 1) ERPOC – infection risk, cervical trauma, uterine perforation, intrauterine adhesions 2) Medical – misoprostol 600mcg PO (PGE1 analogue uterotonic; used in MTOP, miscarriage, induction of labour; stable, low cost, easy to give, patient acceptance; contraindications: previous uterine surgery ( risk of uterine rupture) 3) Watch and wait – longer duration of PV bleeding and pain, need for blood transfusion Discharge with Early Pregnancy Clinic referral if: bleeding not severe, easy hospital access, good discharge advice (come back if deterioration, avoid sex and tampax if threatened), cervical os closed, >6/40 with IUP on scan USS before discharge if: can’t get to EPAC <72hrs, high maternal anxiety and in-hours, >6/40 with no IUP on USS Refer gynaecology if: ?ectopic (unilateral pain, severe, pain, PMH ectopic / tubal surgery / PID), ?actively miscarrying (heavy bleeding / products / USS evidence of miscarriage), unwell, non-viable fetus on USS