Palpitations in primary care- InnovAit, July 2011
advertisement

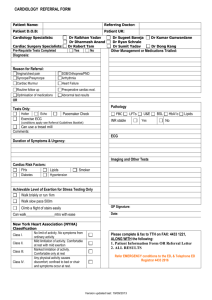
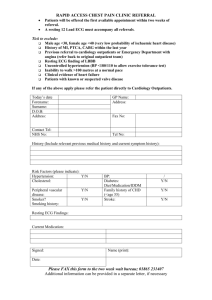
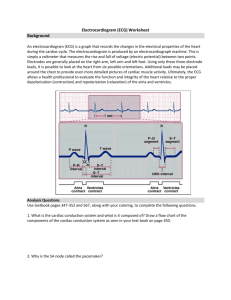
Palpitations in primary careInnovAit, July 2011 Aisha Bhaiyat Aim • Assessment • Management • ECG’s Palpitations • Prevalence – 16% of primary care consultations • 2nd commonest reason for gp referral to cardiology Assessment • • • • • • • • What does the patient mean by palpitation Rate Rhythm Missed/extra beat Associated symptoms Onset/offset Exacerbating/relieving Timings Assessments • • • • • Past medical history Drug history Family history Social history Examination Medical emergency • • • • • Systolic BP less than 90 mmHg Pulse less than 40 or greater than 150 Cardiac failure Chest pain Presyncope Management • • • • ECG Blood tests Ambulatary ECG Transthoracic echo – if structural cardiac abnormality suspected ECG abnormalities that may be present in those with palpitations Conduction abnormalities • BBB • Venricular pre-excitation • Prolongue QTc • Extreme 1st degree block • 2nd/3rd degree block • Other arrythmias eg AF Structural heart disease related • LVH • T wave/ST changes • Features of old MI Red Flags/high risk-urgent referral to cardiology • • • • • Exercise related palpitations Syncope/presyncope FH of sudden cardiac death/inherited heart dx ECG-high degree av block High risk structural disease Amber Flags/moderate risk-refer to cardiology • • • • History suggestive of recurrent tachyarrythmia Palpitation with associated symptoms Abnormal ECG (other than high av block) Structural heart disease Low risk-manage in primary care • • • • Skipped or thumping beats Slow pounding sensation ECG normal No structural heart disease Management and referral pathway for patients presenting with palpitations. Taggar J S , Hodson A, The assessment and management of palpitations in primary care InnovAiT 2011;4(7):408-413, By permission of oxford university press. Further considerations • Opportunistic health promotion • Driving – must cease if arrythmia likely to cause incapacity. Permitted once arrythmia identified and controlled for 4/52. DVLA need to be indentified only symptoms are disabling • Occupation • Genetics-HOCM, WPW, Brugada syndrome, Long QTS Key points • Consider lifestyle/psychological/other systemic medical causes • After initial assessment, patients risk should be stratified and managed appropriately • Other considerations - health promotion/ driving/occupation/genetics Useful websites • Heart Rhythm UK [www.hruk.org.uk/] • Arrhythmia Alliance [www.heartrhythmcharity.org.uk/] (most useful for patient information leaflets) • Sudden Adult Death Trust [www.sadsuk.org/] • Cardiac risk in the young [www.c-r-y.org.uk/]