The role of antifungal drug monitoring
advertisement
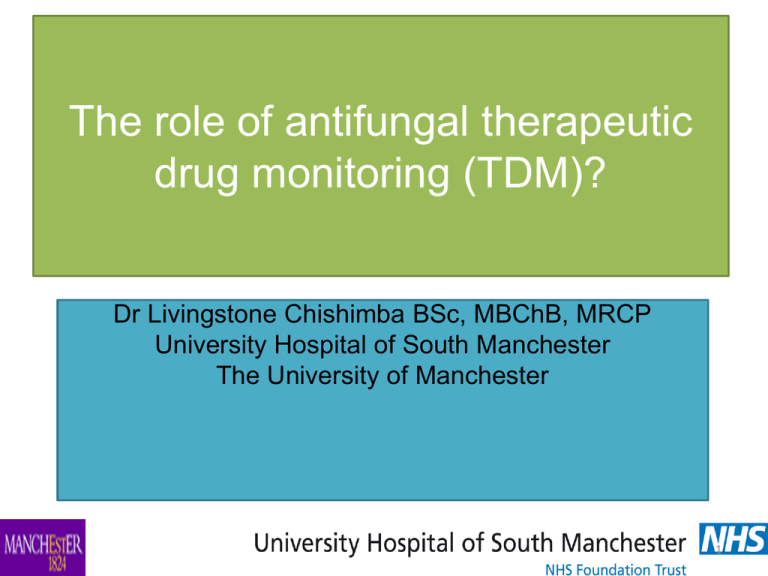
The role of antifungal therapeutic drug monitoring (TDM)? Dr Livingstone Chishimba BSc, MBChB, MRCP University Hospital of South Manchester The University of Manchester 1 Outline • PK affects the antifungal effect • Potential indications for TDM-general • Implications of TDM – Itra,vori, posa, • Efficacy and safety • Studies and evidence • Clinical implication 2 Issues • Why monitoring? • Who to monitor? • What? When? Where ? • What action? • clinically relevant ? – exposure–response relationships – exposure–toxicity relationships 3 TDM-which drugs?-general • compounds with ; – a narrow therapeutic window • Warfarin, theophyllins • variable pharmacokinetics (PK) – itra • physiological instability 4 Clinical objectives of TDM Optimise efficacy Minimise toxicity 5 Hope WW et al. Curr Opin Infect Dis 2008; 21: 580 Clinical use of TDM • drug-drug interactions • check compliance • change of dosage • patient failing therapy 6 Antifungal TDM • Itraconazole • Voriconazole • Posaconazole 7 Itraconazole Itraconazole 8 Two formulations of itraconazole Capsules Excipients differ between generic formulations, and systemic exposure may differ Cyclodextrin excipient 20-50% higher bioavailability Suspension 9 Itraconazole exhibits nonlinear PK Itraconazole, ng/mL plasma Time to steady state ~14 days Once linear clearance achieved, t1/2 ~24 hours Hours Barone JA et al. Antimicrob Agents Chemother 1993; 37: 778 10 Itraconazole: PK and variability • Itraconazole poorly soluble at physiological pH • Absorption of itraconazole tablets is variable; requires acidic environment, which is often absent in critically ill patients • Increased bioavailability with food and cola • Itraconazole suspension is often poorly tolerated (gastrointestinal), leading to compliance problems 11 Variability in itraconazole PK affects the antifungal effect Pulmonary fungal burden Significant relationship between drug level and fungal burden Peak itraconazole concentrations (mg/L) Berenguer J et al. Antimicrob Agents Chemother 1994; 38: 1303 12 Itraconazole: dose-response relationship in rabbits with IA 13 Berenguar et al, AAC 1994;38:1303-8 Itraconazole: incidence of proven invasive fungal infections Capsules • Itraconazole trough concentrations of <0.5 mg/L associated with higher mortality (p= 0.039) Solution • Easier to get better levels with suspension Total Favours itraconazole Favours control Glasmacher et al JCO 2003 14 100 Toxicity and itraconazole concentrations 80 100 60 40 20 Probability of toxicity (%) %Toxicity 40 60 80 20 0 0 0 5 0 5 10 15 20 10 15 20 Itraconazole concentration mg/L ITZ plasma concentration 25 25 NOTE that the highest quintile consists of values ≥ 25.6 mg/L. The line is a logistic regression fit to the individual measurements. 15 Lestner, Clin Infect Dis 2009 In press Itraconazole: concentration-toxicity relationship 100 • 216 patients • mostly capsules 80 Probability of toxicity Pro b a b ility o f t o xic ity ( %) 60 40 A range of AE, most common: •Fluid retention •Gastrointestinal intolerance 20 0 0 5 10 15 20 25 Itra c o n az o le c o n c e n tr at io n m g /L Trough itraconazole concentrations (mg/L) 16 Lestner JM et al. Clin Infect Dis 2009; 49: 928 Itraconazole: concentration-toxicity relationship 100 80 Probability of toxicity Pro b a b ility o f t o xic ity ( %) 60 Probability of toxicity low<17.1>high 40 20 0 0 5 10 15 20 25 Itra c o n az o le c o n c e n tr at io n m g /L Trough itraconazole concentrations (mg/L) 17 Lestner JM et al. Clin Infect Dis 2009; 49: 928 Voriconazole 18 Voriconazole • Displays nonlinear PK in adults, with saturable clearance • Disproportionate changes when dose altered • ~5 days to achieve steady state concentrations • Exhibits linear PK in children • Children may metabolise more quickly • Dose escalation may be required Trifilio SM et al. Antimicrob Agents Chemother 2009; 53: 1793 19 Walsh TJ et al. Antimicrob Agents Chemother 2004; 48: 2166 Voriconazole - metabolism • 98% metabolised by liver • Primarily metabolised by CYP2C19 and CYP3A4, less by CYP2C9. • Genotype status for CYP2C19 and/or co-administration of drugs that modulate CYP2C19 or CYP3A4 activities do affect voriconazole plasma levels. • – PC BRASS, – OAK DEVICESS 3-5% caucasians, 15-20% Asians have genetic polymorphism of CYP2C19 - slow metabolisers • Cirrhosis / prior alcohol abuse, likely predictors of slow metabolisers 20 Voriconazole datasheet Therapeutic drug monitoring may be useful to optimise therapy for individual patients 9 V or i conazol e C oncent r at i on ( mg/ L) 8 A “fast’ metaboliser with relatively low concentrations, who is failing therapy 7 6 5 Dosage escalation from 200 mg bd to 300 mg bd 4 3 2 1 0 0 29 58 87 116 145 174 203 232 261 290 319 348 T i m e (h o u rs ) 21 A “slow’ metaboliser: dosage escalation may be too risky and this could be prevented with TDM 9 Dosage escalation from 200 mg bd to 300 mg bd V ori conazol e C oncent r at i on ( mg/ L) 8 7 6 5 4 3 2 1 0 0 29 58 87 116 145 174 203 232 261 290 319 348 T i m e (h o u rs ) 22 Voriconazole: exposure-response relationships • There have been REAL difficulties linking drug exposure with effect because: – Good PK was not done in the trials (trough, random, mean levels) – Assessing patient outcome is really tough • Random levels of < 2.05 mg/L associated with poorer outcome (Smith et al AAC 2006) • 15% of patients in recent studies have no detectable levels of drug in serum! (Trifilio et al 2007) 23 Efficacy and safety of voriconazole • 26 patients (ABPA, n=21, SAFS=5) • Poor relationship between dose and – Clinical efficacy • ?Good relationship between – Dose, TDL and AEs Chishimba L, denning D et al 2011 (unpublished data) 24 Chishimba L, denning D et al 2011 (unpublished data) 25 Posaconazole 26 Posaconazole • Displays linear PK with dosages of 50-800mg • Saturation of absorption above 800mg/day • ~7-10 days to achieve steady state concentrations • Minimal differences between peak and trough levels • Similar blood concentrations found in juveniles with comparable efficacy and safety Courtney R et al. Antimicrob Agents Chemother 2003; 47: 2788 27 Krishna G et al. Antimicrob Agents Chemother 2007; 51: 812 Posaconazole as salvage therapy for invasive aspergillosis: exposure-response relationship 28 Walsh TJ et al. Clin Infect Dis 2007; 44: 2 Posaconazole: concentration-response relationship from prophylaxis studies Clinical failure of 25% at levels of 0.71mg/L Clinical failure: • death • fungal infection • drug stopped • use of other antifungals http://www.fda/cder/foi/nda/2006/022003s000_Noxafil_ClinPharR.pdf. 2005 Antifungal TDM-Which drug to monitor? Necessary • Itraconazole • Voriconazole (especially IV, children, complex case) • Flucytosine 30 Antifungal TDM-Which to drug to monitor? Desirable • Posaconazole (probably) Unnecessary • Amphotericin B • Echinocandins (not much data though) • Fluconazole (unless short gut and oral administration, or compliance) 31 Itraconazole TDM: clinical practice • Targets – HPLC: >0.5 mg/L – Bioassay >5 mg/L • Low levels with capsules usually due to suboptimal absorption – Administer with food or cola – Stop H2 antagonists, PPIs – Check for drug interactions (rifampicin, phenytoin, carbamazepine). – Can increase from 200 mg b.i.d to 300 mg b.i.d • Change to suspension – Monitor compliance – Understand variance 32 Voriconazole TDM in clinical practice • Target: pre-dose (only) should be monitored – greater than 1.0 and less than ~5.5mg/L • Monitor for duration of therapy • Give loading dose – preferably iv • Look for and expect nonlinear behaviour when adjusting dose 33 Posaconazole TDM in clinical practice • Targets not well defined – Trough >0.5mg/L prophylaxis – Trough 0.5-1.5mg/L therapy • Absorption affected by a number of factors: – frequency of dosage (saturable) – food, gastric pH and mucosal health • Side effects: – insufficient data to determine if dose-dependent • To increase levels: – may not be any benefit going >800mg/day – fractionate dose – give with fatty food 34 Andes D et al. Antimicrob Agents Chemother 2009; 53: 24 Take home message • Linear PK: itra and posa • None linear PK: vori • Dose alteration not only on TDL but on clinical response, Aes • Consider drug interactions – PPI, antiepileptics , macrolides • time-diet timing etc if not able to achieve TDL but clinical outcome most important. – frequency of dosage (saturable) – food, gastric pH and mucosal health • but much more work required using population PK modelling to reach the goal of truly individualising therapy! 35